Musculoskeletal injuries in the female athlete are for the most part similar to those in the male athlete. However, there are differences in the incidence of these injuries and in the sports in which they tend to occur.1 Stress fractures are more common in the female athlete because of the higher prevalence of eating disorders and subsequent osteopenia in females. In addition, for reasons that are not completely elucidated, the female athlete has a higher rate of noncontact anterior cruciate ligament (ACL) injuries than the male athlete. Finally, as a function of greater participation by females in certain sports, such as dance and gymnastics, injuries specific to those sports are more common in females.
Stress Fractures
Stress fractures result from an imbalance between bone resorption and formation secondary to repetitive submaximal loads. Extrinsic mechanical causes that can induce this imbalance include duration, frequency, and intensity of load; muscle fatigue; and the shock-absorbing capacity of sports equipment. Intrinsic causes for abnormalities in bone remodeling include the nutritional and hormonal milieu, as well as endocrine disorders that are beyond the scope of this topic. Disordered eating, amenorrhea, and low bone mineral density—the so-called female athlete triad—can result in osteoporosis in young women.1 Insufficient caloric intake for the expenditure required for sports is thought to lead to changes in the pulsatile secretion of gonadotropin-releasing hormone and abnormalities in luteinizing hormone, which in turn produce the menstrual irregularities found in some female athletes.2
Amenorrhea and oligomenorrhea may cause loss of 2% of bone mass a year, especially when these conditions occur during late adolescence and early adulthood—periods during which peak bone mass is acquired.3 When amenorrhea is present for more than 3 years, treatment with calcium and estrogen will not reverse this bone loss; nor is there evidence that treatment with oral contraceptives prevents stress fractures.4 Many studies report increased stress fracture rates in athletes with menstrual irregularities, even when dual-energy x-ray absorptiometry indicates that their bone density lies within the normal range.4 Epi-demiologic studies of stress fractures in athletes and military recruits have shown that these injuries are 1.5 to 4 times more common in females than in males.5-7 This differential between male and female athletes is especially notable for stress fractures in the pelvis, femoral neck, and metatarsals.
General treatment guidelines
Recommending that the patient rest the affected body part— the standard treatment for stress fractures—is insufficient for female athletes. Instead, the physician needs to address any features of the athlete’s training habits, nutritional and menstrual status, or equipment that may have contributed to the stress fracture. This will ensure that once the fracture heals, the patient will not be exposed to the same factors that led to the fracture.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are con-traindicated in the treatment of pain related to stress fractures, because there is evidence that NSAIDs may interfere with fracture healing.8,9 When pharmacologic pain control is needed, acetaminophen usually suffices.
A stress fracture is healed when the involved bone is no longer tender to palpation and the patient is able to tolerate either impact on the bone or the use of muscles that place stress on the bone. Progressive return to the desired activity level ensues. For lower-limb fractures, the patient can begin a so-called amphibious rehabilitation program when she can walk without discomfort. In this program, patients begin by jogging in water that is chest high and gradually progress to waist-high water. They then move out of the water and onto land. The decrease in buoyancy provides a gradually increasing load to the bone, giving it a chance to adapt. The next step is sport-specific rehabilitation: the athlete resumes her former training regimen for her sport but starts with a time or distance that is about a third of that at the time of fracture. The mileage or time is then increased at a rate of 10% to 15% a week.
Pubic ramus stress fractures
Pelvic stress fractures make up only 1% to 5% of all stress fractures in all runners, but they are significantly more common in female runners. The most common site is the inferior pubic ramus. In a military population, Hill and colleagues found that 11 of 12 pubic ramus fractures were in female recruits.10
Pathophysiology
A crossover running style and overstriding may contribute to the higher incidence of pubic ramus stress fractures in female athletes. The term crossover running refers to adduction of the lower extremity across the line of gait progression. This may occur more commonly in women because of their wider pelves. Overstriding refers to excessive flexion of the lower extremity; it is usually done either to gain speed or to keep up with a taller running partner. Both crossover running and overstriding create repetitive pull by the adductor musculature at its origin on the pubic ramus. Sometimes this pull results in adductor tendinitis; at other times, it results in inferior pubic ramus stress fractures.
Diagnosis
The patient complains of groin or medial thigh pain that increases with activity, especially impact, and is relieved by rest. The physician should ask whether the patient runs with a taller partner. The differential diagnoses of adductor tendinitis, osteitis pubis, and pain originating in the hip joint can be sorted out through careful physical examination and imaging studies.
Physical examination findings Painless range of motion of the hip essentially rules out the hip as the origin of the pain. The key physical findings in pelvic stress fracture include tenderness to palpation of the pubic ramus and difficulty standing on one leg. Pain with resisted use of the adductor muscles is common but is not helpful for sorting out the other possible diagnoses. Pain during passive adductor stretch is more consistent with tendinitis.
Imaging studies Unless the fracture is very recent, it will appear on an anteroposterior radiograph of the pelvis as a lucent line in the pubic ramus, often surrounded by callus [see Figure 1]. When the radiograph is unremarkable but a stress fracture seems likely, the physician should obtain either a bone scan or a magnetic resonance imaging scan. Bone scans are very sensitive, although not specific, and usually suffice to make the diagnosis. MRI can reveal a stress fracture; alternatively, it may show fluid in the adductor tendons or edema on both sides of the symphysis pubis in patients with tendinitis or osteitis pubis, respectively.
Treatment
The patient should stop impact activity, as well as other activities that cause pain. If walking is painful, then crutches should be prescribed for a few weeks, or until the patient can walk without pain. Swimming is often well tolerated as long as the patient avoids the whip kick, which uses the adductor muscles. Bicycling may not be tolerated, because despite the lack of impact, the bicycle seat often presses right on the area of the fracture, creating discomfort.
Pubic ramus stress fractures may take from 2 to 5 months to heal. Surgical treatment is not indicated.
Femoral neck stress fractures
Femoral neck stress fracture is relatively uncommon, accounting for less than 10% of all stress fractures,7 but it is two to four times more common in women than in men.6,11 Moreover, this fracture typically does not occur in the recreational or novice athlete but rather in athletes who participate in high-level training six or more times a week and who have been involved in regular training for more than 2 years.6 If the diagnosis is missed, a femoral neck stress fracture may progress to complete fracture, with potentially devastating consequences.
Pathophysiology
In epidemiologic studies, femoral neck stress fractures have been associated with overuse and with demineralization. Weak hip musculature and a discrepancy in leg length of greater than 0.5 in. may contribute as well.
Diagnosis
Patients with a femoral neck stress fracture complain of groin or thigh pain, often referred to the medial knee (via the obturator nerve). The pain increases with weight bearing or impact activity.
Physical examination findings Tenderness to palpation of the femoral neck is rare because of the thickness of the soft tissues in this area. Passive log-rolling of the lower limb may produce pain. If not, active straight-leg raising and passive movement of the hip to its maximal range of motion should be performed; these maneuvers will produce pain in patients with a femoral neck stress fracture. Standing on only the affected limb often produces pain. The Trendelenburg sign is sometimes positive. When none of these findings are present, the examiner should check patellar tendon reflexes, quadriceps muscle strength, and ankle dorsiflexion strength to assess L3 and L4 nerve root function. Strength testing of the hip flexor muscles can yield confusing results in this setting because weakness may be from inhibition by pain rather than a neurologic deficit.
Imaging studies In two thirds of the cases of femoral neck stress fractures, the fracture does not appear on radiographs.12 Bone scans are so sensitive (93% to 100%) that increased uptake is commonly seen in military recruits whose fractures are asymptomatic. MRI is accurate (100% with MRI, as compared with 68% with bone scan), sensitive, and specific.12 If an in-trapelvic lesion seems possible, the radiologist can be asked to include the pelvis in the hip MRI, or vice versa.
Differential Diagnosis
The differential diagnosis for groin or anterior thigh pain includes adductor tendinitis, osteitis pubis, and pubic ramus stress fracture (see above). In addition, pressure on either the obturator nerve or the femoral nerve from an intrapelvic mass, as well as disk disease at the L2-L4 levels, can produce pain in the same distribution.
Treatment
The treatment depends on the location of the stress fracture in the femoral neck. The superolateral aspect of the neck is under tension; consequently, patients with fractures at this site are at increased risk for complete fracture and displacement. The inferomedial aspect of the neck is under compression; for that reason, complete fracture is less likely. Therefore, medial femoral neck stress fractures are usually treated by the avoidance of weight bearing on the involved limb until the patient is pain free. This may take months. Follow-up radiographs should be obtained monthly, or sooner if symptoms change. Swimming and cycling are not allowed because of the forces across the hip joint induced by the musculature. Patients with medial femoral neck stress fractures should be referred to an orthopedic surgeon if they show no improvement in symptoms after 3 months or if follow-up radiographs show propagation of a fracture line.
Figure 1 In a patient with a stress fracture of the inferior pubic ramus, the fracture will appear on an anteroposterior radiograph of the pelvis as a lucent line in the pubic ramus (arrow), often surrounded by callus.
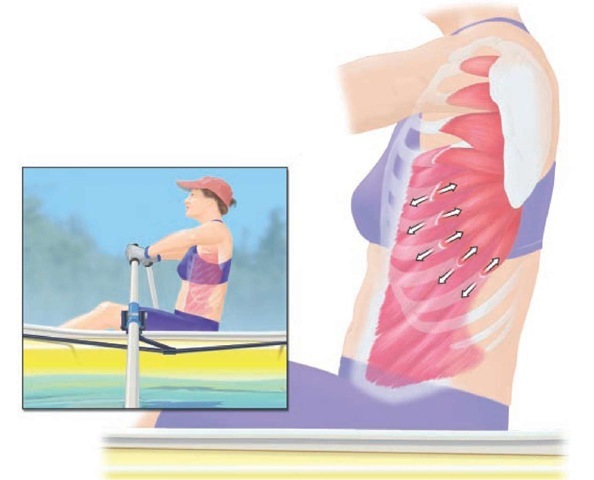
Figure 2 Stress fractures of the ribs in women rowers typically occur in ribs five through nine, on the anterolateral to posterolateral aspect of the rib. The fractures may result from repetitive stress at the shared site of insertion of the serratus anterior and the external oblique muscles; the serratus anterior pulls the ribs up and back, whereas the external oblique pulls the ribs down and in.
Lateral femoral neck stress fractures are usually treated with internal fixation and thus require immediate referral to an orthopedic surgeon. Although internal fixation is debated, no prospective studies have compared operative and nonoperative treatment of the lateral femoral neck stress fracture because of the fear that nonoperative care will result in complete fracture, with its risk of subsequent avascular necrosis, malunion, or nonunion.12
Rib stress fractures in rowers
Rib stress fractures account for 7.4% of all injuries in the female rower. These fractures typically occur in ribs five through nine, on the anterolateral to posterolateral aspect of the rib.13
Pathophysiology
Ribs five through nine share the insertion of the serratus anterior and the external oblique muscles; the serratus anterior pulls the ribs up and back, whereas the external oblique pulls the ribs down and in [see Figure 2]. Holden and Jackson attribute these fractures to repetitive stress on the ribs from the pull of these muscles.14
Diagnosis
Clinical manifestations Rowers with rib stress fractures present with chest or thoracic back pain that increases during rowing or weight lifting. Coughing also produces pain.
Physical examination findings Patients have tenderness to palpation on the affected rib, usually between the anterior and posterior axillary lines. Compression of the rib cage in an anterior to posterior direction and from side to side increases pain in patients with rib fractures, because these maneuvers produce bending stress on the rib cage. This finding holds even when the compression is applied away from the tender rib. When the problem is muscular, rib-cage compression does not usually produce pain. Muscle and rib injures cannot be differentiated on the basis of resisted muscle use.
Imaging studies The diagnosis of rib stress fractures is confirmed by bone scan.
Differential Diagnosis
The differential diagnosis of rib stress fracture includes muscle strain involving the serratus anterior, pectoralis, or inferior trapezius. Pulmonary or cardiac problems must also be excluded.
Treatment
The athlete should stop rowing. If coughing produces significant pain, a rib belt can be prescribed. While waiting for the fracture to heal, the athlete may do core strengthening and scapular stabilization exercises, omitting the serratus anterior. Once the rib is nontender, serratus strengthening exercises should be added, with gradual return to rowing. Surgical treatment is not indicated for this fracture.
Multidirectional Shoulder Instability
Shoulder problems are especially prevalent in athletes who engage in swimming, racquet sports, and softball. These sports involve frequent overhead use of the arm, which, in the presence of instability, can cause secondary impingement under the acromion. Shoulder problems are also common in gymnasts, who use the shoulder as a weight-bearing joint.15 Acquired laxity has been noted in gymnasts, weight lifters, and swimmers who use the butterfly stroke or the backstroke. Laxity, however, is not synonymous with instability; the term instability refers to symptomatic laxity.
Shoulder instability can result from acute trauma or repetitive microtrauma; it may also be atraumatic and multidirectional. Traumatic shoulder instability is more common in males, whereas multidirectional instability is believed to be more common in females, although the literature in this regard is contro-versial.16 Generalized ligamentous laxity, which may play a role in shoulder instability, has been noted in numerous studies of multidirectional instability. McFarland and colleagues observed that in 178 asymptomatic high school and college athletes, the shoulder could be subluxated posteriorly in 65% of females compared with 51% of males; generalized laxity was also significantly more common in the female athletes.17
Pathophysiology
Shoulders with multidirectional instability have large inferior capsular pouches that extend both anteriorly and posteriorly. Often, the tissue in the rotator interval between the supraspina-tus and subscapularis tendons is attenuated.15 Some authors have theorized that proprioception is abnormal in these patients, or that weak rotator cuff muscles fail to generate an adequate compressive force against an intact labrum. This type of muscular force is especially important for stabilizing a lax shoulder.
Diagnosis
Clinical Manifestations
Patients with multidirectional shoulder instability often present with pain rather than dislocations. The pain occurs during activities of daily living while the shoulder is in the middle of its range of motion, rather than in the extreme ranges normally associated with traumatic dislocations. The pain is aggravated by overhead use of the arm. Subluxations and dislocations may occur during low-demand activities such as carrying objects with the arm at the side. In extreme cases, the patient is able to voluntarily subluxate or dislocate the glenohumeral joint, as well as reduce it spontaneously.
When a patient presents with pain rather than instability, the differential diagnosis is broad and can include stress fractures, rotator cuff injuries, and tumors, in addition to referred pain from the cervical nerve roots or heart.
Physical Examination Findings
Diagnostic criteria for multidirectional shoulder instability include the demonstration of subluxation in multiple directions in a patient with a history of midrange symptoms.15 Frequently, the contralateral shoulder is also lax but not symptomatic. The examination should start with an evaluation of the entire kinetic chain, looking for spinal postural abnormalities, hip weakness, and scapular dyskinesia. The one-legged-instability screening test can be informative.18
Figure 3 In a patient with multidirectional shoulder instability, pulling down on the arm at the side may produce inferior translation of the humeral head, as demonstrated by an indentation or dimple beneath the acromion (sulcus sign).
On examination of the shoulder girdle, the distance between the scapula and the thoracic spine should be symmetrical bilaterally. During range of motion of the arm, the scapula should rotate laterally as the arm elevates. The scapula should not wing away from the thorax. The rotator cuff muscles should be tested with and without scapular retraction. If muscle strength improves with scapular retraction, the functional weakness is more likely from poor scapular stabilization, rather than cuff weakness per se.
Pulling down on the arm at the side may produce inferior translation of the humeral head, as demonstrated by an indentation or dimple beneath the acromion (sulcus sign) [see Figure 3]. This test is positive when the inferior translation exceeds 1 to 2 cm; it reflects insufficiency of the superior glenohumeral ligament and capsular rotator interval. The same finding when the arm is tested while abducted 90° reflects attenuation in the inferior capsule.
The degree of instability can be further assessed with the so-called load-and-shift test. With the patient in the supine or lateral decubitus position, the examiner uses one hand to apply an axial load, pushing upward on the arm to force it into the socket, and uses the other hand to shift the patient’s arm posteriorly or anteriorly.15 The glenohumeral joint may dislocate or subluxate in more than one direction (e.g., inferiorly, posteriorly, or anteriorly), with the patient experiencing symptoms in one or more directions.