Measles
Measles (rubeola) is a highly infectious disease caused by a paramyxovirus of worldwide distribution. The measles virus was once one of the most common and important global pathogens, but infections caused by this agent are now becoming rare in developed countries, where vaccine use is widespread. In areas where vaccines are not widely used, measles remains a major health problem. It is estimated that worldwide, over 800,000 deaths occur each year from measles
Epidemiology
Humans are the principal reservoirs of measles virus, which is spread by respiratory droplet aerosols produced by sneezing and coughing. The disease may be contagious from several days before the onset of rash to up to 5 days after lesions appear. The attack rate for exposed susceptible contacts may exceed 90%; asymptomatic infections are rare.
Vaccines have dramatically reduced the incidence of indigenous measles in the United States and have eliminated the disease altogether in some developed countries. However, large outbreaks still occur in unvaccinated or suboptimally vaccinated populations, and an outbreak has even been reported in a highly vaccinated population.2-4 In the United States, women born after the licensure of measles vaccine transfer less measles antibody to their infants than do older women, which may leave infants of vaccinated mothers with heightened susceptibility to measles.5
In undernourished children in developing countries, measles can cause a devastating illness, and case-fatality rates may reach or exceed 25%.6 Before widespread vaccine use, epidemics occurred every 2 to 3 years in developed countries, and the illness developed in 95% of urban dwellers before they reached 15 years of age. Outbreaks occurred primarily in late winter and early spring. In 1989, the World Health Assembly instituted major efforts to reduce measles morbidity and mortality through implementation of control strategies. By 1996, estimated incidence and death rates were reduced by 78% and 88%, respectively.1,7,8 In the Americas, between 1990 and 1996, the number of new measles cases decreased from 246,607 to 2,109 (a decrease of 99%), and vaccine coverage increased from 77% to 85%. In 2000, only 100 confirmed measles cases were reported in the United States, the lowest number on record.1 Molecular epidemiologic studies suggest that most cases in the United States now result from importation of virus.1,9,10
Pathogenesis
The portals of entry for measles virus include cells of the respiratory tract and possibly the conjunctivae. After undergoing local replication and spreading to regional lymph nodes, measles virus is disseminated to distant sites, particularly skin and mucous membranes, by a leukocyte-associated viremia. Lesions on mucous membranes (Koplik spots) appear as bluish-white specks on an erythematous base. Histologically, Koplik spots are composed of epithelioid giant cells with cytoplasmic and nuclear inclusions that contain microtubular aggregates; inflammatory cells and in tercellular edema are present. Lesions of the skin also demonstrate inclusions and microtubular aggregates, suggesting that active viral replication occurs in skin as well as in mucous membranes. Infectious virus can be isolated from leukocytes, urine, conjunctivae, and respiratory secretions. Antibody appears in the serum as viremia ceases. Leukopenia may accompany the illness, together with lymphocyte hyporesponsiveness.
Diagnosis
Clinical Features
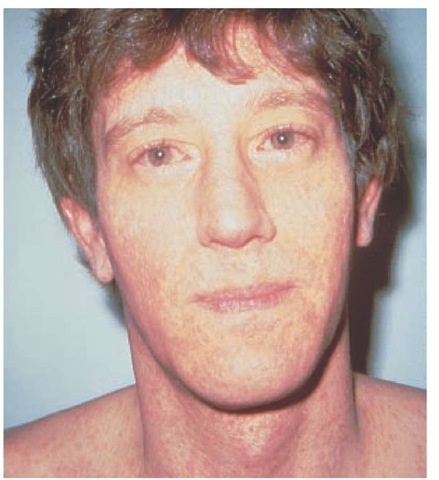
Approximately 9 to 11 days after a person is initially exposed to the virus, malaise, fever, conjunctivitis, photophobia, perior-bital edema, coryza, and cough develop. Cough may be severe, although generally nonproductive, and temperature may reach 40.6° C (105.1° F). Within 2 to 3 days, Koplik spots may appear on the buccal mucosa and occasionally on the conjunctivae. The skin rash, which erupts 2 to 3 days later, usually appears at the hairline and spreads downward during the next 3 days as systemic symptoms subside [see Figure 1]. Lesion density is greatest above the shoulders, where macular lesions may coalesce. The rash lasts 4 to 6 days and then fades from the head downward. Desquamation may be present but is usually not severe. Complete recovery without scarring generally occurs within 7 to 10 days from the onset of the rash.
A severe atypical presentation of measles may appear in persons who were immunized between 1963 and 1967 with killed measles virus vaccine and who were later exposed to the wild virus. After a prodrome of fever, headache, abdominal pain, and myalgias, a rash develops on the hands and feet and advances toward the head. The eruption may be vesicular, urticarial, mac-ulopapular, or hemorrhagic and is most prominent along body creases. Pneumonia, pleural effusion, and hilar lymphadenopa-thy are common in atypical measles. All persons vaccinated after 1967 received the live attenuated measles vaccine, which is rarely, if ever, associated with the atypical measles syndrome.
Laboratory Tests
In an epidemic setting, observation of the characteristic rash, fever, coryza, and conjunctivitis is sufficient to establish the diagnosis. However, as measles declines in prevalence, clinical acumen in diagnosis also diminishes. Multinucleated giant cells can often be detected in stained smears of nasal secretions, and measles antigen can be demonstrated in such cells by immuno-fluorescence. The virus can be isolated from nasal secretions or urine by cultivation of such materials on primate cell monolay-ers. A rise in hemagglutination inhibition antibodies during a period of 2 to 3 weeks confirms the diagnosis. Confirmation by measles-specific IgM enzyme immunoassay is also available.
Differential diagnosis
Sporadic cases of measles must be differentiated from other viral exanthems, secondary syphilis, scarlet fever, and drug reactions. Atypical measles may resemble Rocky Mountain spotted fever, meningococcemia, or varicella.
Complications
Measles is usually benign and uncomplicated. Complications occur more commonly in adults, malnourished children, and immunocompromised patients. Measles is associated with severe pulmonary and neurologic complications in up to 80% of immunocompromised children and adults with cancer or HIV infection, with case-fatality rates of 40% to 70%; rash is absent in 30%.11,12 Measles virus may further suppress host immune responses, leading to reactivation of latent tuberculosis or super-imposition of new bacterial pneumonia, particularly in malnourished children.
Measles virus infection often involves the central nervous system, but clinically apparent encephalomyelitis is rare (one in every 1,000 to 2,000 measles patients). CNS involvement may precede the rash but usually begins 4 to 7 days after the eruption appears. The onset of encephalomyelitis is often precipitous and is characterized by a rise in fever, sudden mental deterioration, and seizures; motor defects and cerebellar ataxia are common. An autoimmune demyelinating process may be involved in the pathogenesis of measles encephalomyelitis, which is fatal in about 10% of patients.
Subacute measles encephalitis may complicate measles in im-munocompromised hosts 1 to 7 months after exposure; the patient has seizures and altered mental status, but results of cere-brospinal fluid analysis are normal.13 Diagnosis may require brain biopsy for histology, immunocytochemical analysis, or polymerase chain reaction (PCR) detection of viral RNA.12 In rare instances, a subacute sclerosing panencephalitis occurs as a complication of measles in children infected before 2 years of age, but the panencephalitis develops after a latent period of several years. Other measles complications include thrombocytopenia with associated purpura or bleeding, myocarditis, pericarditis, hepatitis, and severe keratitis progressing to blindness.
Treatment and prevention
Therapy for measles is mainly supportive. A meta-analysis has suggested that in areas where vitamin A deficiency may be present, an oral dose of 200,000 IU of vitamin A for 2 days can reduce morbidity and mortality in children.14 Ribavirin, either intravenous or aerosolized, has been proposed for certain complications of measles (i.e., encephalitis or pneumonitis),11,12 but controlled trials are lacking.
Postexposure prophylaxis can be provided for high-risk patients (e.g., pregnant women and immunosuppressed children) by administering immunoglobulin intramuscularly at a dosage of 0.25 to 0.50 ml/kg body weight within 6 days after exposure.
In vaccination guidelines in the United States, two immunizations are suggested for children before school enrollment to reduce the chance of primary vaccine failure. Vaccination is recommended for nonpregnant women of childbearing years and may be considered for institutionalized adults or individuals working in day care centers [see CE:V Adult Preventive Health Care]. Severely immunocompromised individuals should avoid measles vaccination because of the risk of vaccine-associated diseases, such as inclusion body encephalitis or pneumonitis.
The effort to eradicate measles from the United States relies on identification and immunization of susceptible children, adolescents, and adults; on strict enforcement of more comprehensive school immunization requirements; and on strengthening of surveillance and outbreak-control measures.
Figure 1 A case of measles in a young man is characterized by maculopapular rash and conjunctivitis.
Mumps
Mumps virus is a pleomorphic, enveloped, single-stranded RNA paramyxovirus capable of causing parotitis, epididymo-orchitis, and CNS disease. Because of widespread vaccination efforts, its role as a major cause of childhood morbidity has greatly diminished.
Epidemiology
Mumps virus has worldwide distribution, and infection is seen more commonly in winter and spring. Humans are the only natural host. Infection is uncommon in persons younger than 1 year, and congenital infection is rare but can lead to fetal loss in the first trimester. Approximately 11% of cases of mumps are observed in children between 1 and 4 years of age, 52% in children between 5 and 14 years of age, and 11% in children older than 15 years.
A live mumps virus vaccine was approved for use in the United States in 1967; its use was facilitated by subsequent incorporation with measles and rubella (MMR) vaccine. Since its widespread use, mumps cases have fallen by over 99.5%, from 185,691 cases in 1968 to 906 cases in 1995.15 Healthy People 2010, a comprehensive set of health objectives created under the auspices of the United States Department of Health and Human Services, has targeted mumps for elimination in the United States by 2010.18
Pathogenesis
Mumps virus spreads from person to person by direct contact with nasopharyngeal secretions. Virus is shed in saliva from as long as 6 days before to 5 days after clinical onset. Incubation ranges from 2 to 4 weeks (mean, 18 days). Initial replication occurs in the pharynx, followed by viremic dissemination. Both humoral and cell-mediated immune responses are induced and correlate with cessation of viremia and salivary virus excretion.
Diagnosis
Clinical Features
Two thirds of cases are symptomatic, with initial symptoms of malaise and fever predominating. Painful swelling of the parotid gland is the characteristic feature of infection. It may be unilateral, and other salivary glands may be involved. However, parotitis occurs in only 30% to 40% of all cases of mumps virus infection.
An unvaccinated child who presents with tender parotitis generally has mumps; further diagnostic testing is not required. In older age groups, other entities (sarcoidosis, tumors, alcohol abuse, drug side effects, and other viral or bacterial infections) should be considered. In persons without parotitis who have or-chitis, aseptic meningitis, encephalitis, or other obscure syndromes (e.g., myocarditis or pancreatitis), mumps should be considered [see Complications, below].
Laboratory Tests
Definitive diagnosis of mumps can be made by virus isolation from the oropharynx, CSF, or urine or by virus serology. Rapid detection by PCR techniques is now possible in some laboratories.19
Complications
Epididymo-orchitis occurs in up to 38% of postpubertal males with mumps and is usually unilateral. Subsequent sterility is uncommon, although testicular atrophy may occur.
CSF pleocytosis occurs in at least 50% of patients with mumps,20 although symptomatic meningitis is less common. A lymphocyt-ic pleocytosis is seen, with an elevated protein level and a normal to low (10%) glucose level. Symptomatic encephalitis occurs in one of 6,000 cases and presents as decreased consciousness and focal neurologic deficits. Most patients with encephalitis recover completely, although 0.5% to 2.3% of patients with mumps encephalitis may die. Other neurologic complications may include hydrocephalus; deafness; and rare cases of demyelinating disorders, transverse myelitis, Guillain-Barre syndrome, and cerebellar ataxia.21 Deafness may be sudden, unilateral, and permanent.15
Pancreatitis, mastitis, and oophoritis have been observed in patients with mumps. Myocarditis occurs and in rare cases can be fatal.22 Endocardial fibroelastosis, an infrequent sequela of myocarditis, has been associated with mumps infection.23 Mumps can cause polyarticular or monoarticular arthritis; it generally affects adult males and is self-limited (usually less than 8 weeks).
Treatment and prevention
Treatment of patients with mumps is largely supportive, although anti-inflammatory agents may be useful in cases of severe orchitis or arthritis. Administration of immune globulin does not prevent mumps and is not recommended. Prevention can be achieved in well over 90% of persons by the use of live attenuated mumps vaccine, administered twice as part of the recommended MMR vaccine regimen15 [see CE:VAdult Preventive Health Care].
Rubella
Rubella, or German measles, is usually a benign febrile exan-them, but when it occurs in pregnant women, it can produce major congenital malformations. The infective agent is a single-stranded RNA virus of the Togaviridae family.
Epidemiology
Humans are the only known natural hosts for the rubella virus, which appears to be spread by respiratory droplets. The virus is moderately contagious but less so than measles. Before the introduction of a rubella vaccine, in 1969, epidemics occurred in the United States at 6- to 9-year intervals, predominantly in children younger than 15 years. Since the widespread use of rubella vaccine, the incidence of rubella has decreased by 99%.25 Outbreaks continue to occur, primarily in young adults in hospitals, colleges, prisons, and prenatal clinics, but no major epidemics have occurred in the United States since 1964. Susceptibility rates in young adults vary, with the greatest proportion of cases now seen among persons of Hispanic origin.25,26 Rubella outbreaks have recently been identified in processing plants for meat and poultry where many foreign-born workers are em-ployed.26 Less than 10 confirmed cases of congenital rubella syndrome are reported in the United States annually, almost all of them in infants of foreign-born mothers.26
Pathogenesis
Initially, the rubella virus replicates in the nasopharynx and regional lymph nodes. After the virus invades the bloodstream, it may spread to the skin and distal organs or, transplacentally, to the developing fetus. The virus may be present in throat washings or blood for several days before the appearance of the rash and up to 2 weeks after its onset. In rare cases of rubella arthropathy, the virus may persist in peripheral leukocytes or in synovial cells for months to years.
A pregnant woman infected with rubella is at risk for transmitting the virus to her fetus. Damage to the fetus is most likely to occur if the mother is infected within the first 2 months of gestation (fetal abnormalities are observed in 40% to 85% of such cases).27,28 Infection within the third month is associated with fetal defects in 20% to 40% of cases, whereas infection during the fourth month is associated with fetal defects in 10% of cases. Mechanisms of fetal damage are not clear but may include viral cytolysis, chromosomal breaks, reduced cell multiplication, and alteration of fetal blood supply. As a result, fetal growth may be retarded, and defects may develop in multiple organ systems. Despite the production of fetal antibodies, the rubella virus can persist in the fetus and newborn and can be excreted for months to years after birth.
Diagnosis
Clinical Features
After an incubation period of 12 to 23 days, a mild prodrome of malaise, headache, fever, and mild conjunctivitis may develop. Postauricular, suboccipital, and posterior cervical lymphade-nopathy often precede the rash, which begins on the face and forehead. Within 1 to 5 days, the discrete maculopapular lesions spread over the trunk and extremities and may coalesce. The rash usually disappears within 3 days.
Laboratory Tests
The presence of rubella can be confirmed by virus isolation, by PCR detection, or by demonstration of seroconversion in response to rubella antigens. Virus isolation is often difficult because rubella virus does not cause cytopathic effects on the cell lines that are generally employed in diagnostic laboratories. Antibodies are often present shortly after rash appears and increase in titer during the next 2 to 3 weeks. Measurements of specific IgM antibodies to rubella virus are particularly useful in new-borns: raised IgM levels denote recent infection and are specific for fetal infection because IgM antibodies do not cross the placenta. Elevated IgM antibodies may return to nondiagnostic levels by 3 to 6 months, and persistence of IgG antibodies beyond this period may also help diagnose neonatal infection.25
Differential diagnosis
Rubella may be confused with other viral exanthems (e.g., those caused by enteroviruses, parvoviruses, or adenoviruses), scarlet fever, or drug eruptions.
Complications
The most common complications of rubella are arthropathies of the fingers, wrists, and knees; they occur predominantly in young women. Such arthropathies consist of arthralgia or frank arthritis, and recurring joint symptoms may persist for a year or more. Encephalitis and thrombocytopenia are rare complications of acute rubella. Encephalitis occurs in one in 6,000 cases,15 and thrombocytopenia, which is sometimes associated with pur-pura or hemorrhage, occurs most often in children.
Congenital rubella syndrome, also a rare complication of acute rubella, may manifest itself as defects in one or many organ systems. Hearing impairment is the most common single defect (60%).25 Heart malformations, particularly patent ductus arteriosus and peripheral pulmonic stenosis, are also common (45%), as are cataracts (25%), microcephaly (27%), and mental retardation (13%). Malformation of bone metaphyses may also be present, together with hepatosplenomegaly, thrombocytopenia, interstitial pneumonitis, myocarditis, and thrombocytopenic purpura. Congenitally infected infants are often of low birth weight (23%), and they excrete rubella virus for prolonged periods. Late complications may result from imbalances of cellular and humoral immunity, from immune complex deposition, or from prolonged viral replication. Diabetes mellitus and other endocrine abnormalities may be late complications of congenital rubella, as is subacute sclerosing panencephalitis.
Treatment and prevention
Beyond the fetal period, rubella is mild and self-limited. Current treatment of congenital rubella syndrome is only supportive. The Centers for Disease Control and Prevention (CDC) has developed detailed recommendations for dealing with rubella outbreaks focused on patient isolation, identification and vaccination of susceptible persons who have no contraindications to rubella vaccine, and counseling of susceptible pregnant women.26 These recommendations are available on the Internet at http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5012a1.htm.
Pregnant women infected with rubella virus who are asymptomatic may still transmit rubella to their fetuses. Thus, testing of immune status is advisable for women of childbearing age and for hospital employees who have no history of rubella vaccination. About 10% to 15% of such persons are seronegative and should be vaccinated when not pregnant. Women should avoid becoming pregnant for 28 days after vaccination against rubella.30
Measles, Mumps, and Rubella Vaccine
Because they fear possible complications from MMR vaccination, some parents question the safety of the vaccine, and in some cases, they are refusing its use in their children. These parents may cite research suggesting that MMR vaccination may be a risk factor for inflammatory bowel disease31 and autism.32 Subsequent research, however, has not supported this hypothesis.
In addition, although receipt of the MMR vaccine has been associated with an increased risk of febrile seizures 8 to 14 days after vaccination, those children were not found to be at higher risk for subsequent seizures or neurodevelopmental disabilities.
Parvovirus
Although only recently recognized as a human pathogen, parvovirus B19 is now appreciated as a cause of several syndromes in both children and adults. Parvovirus B19, a small (20 to 26 nm), single-stranded DNA virus, causes erythema infectio-sum (fifth disease) in normal persons, aplastic crises in persons with underlying hemolytic disorders, chronic anemia in im-munocompromised hosts, and fetal loss in pregnant women.