Definition
Seizures are caused by transient, paroxysmal, and synchronous discharges of groups of neurons in the brain. Although considered abnormal, seizures can occur in both normal and abnormal brain tissue. Seizures are one of the most common neurologic disorders and may occur at any age. More than 10% of the population will have a seizure or a few seizures during a lifetime. The clinical manifestations of seizures depend on the location and number of the neurons involved in the seizure discharge, the spread of the discharge to other parts of the brain, and the duration of the discharge. Seizures may be caused by a transient abnormality of brain function resulting from such clinical events as hypoglycemia, hyponatremia, and drug toxicity. In these circumstances, a person usually has only a single seizure or a few seizures at most; treatment of the underlying abnormality corrects the seizure disorder.
Epilepsy is defined as recurrent seizures. Epilepsy occurs in 1% to 2% of the population. The incidence of epilepsy is high in infancy but decreases during childhood; it is lowest in adolescence and adulthood but increases greatly in the elderly.
Epilepsy may result from hereditary or acquired factors. Hereditary epilepsies typically have a complex pattern of inheritance, with simultaneous involvement of multiple genes, and the identity of genes that govern susceptibility remains largely unknown.2 An increasing number of hereditary epileptic syndromes have been traced to mutations in genes that encode for ion channels—membrane-spanning proteins that form selective pores for sodium, potassium, chloride, or calcium ions and that provide the basis for regulating excitability in the central nervous system. Diseases resulting from mutated ion channels are termed channelopathies.3
Acquired epilepsy is often the result of a chronic, static neurologic abnormality. Causes include head trauma, CNS infection, structural brain malformations, vascular malformations, strokes, and cerebral neoplasm.
Classification
The International League Against Epilepsy has classified epileptic seizures on the basis of clinical and electroencephalo-graphic criteria [see Table 1]. Proposed in 1981, this classification is widely accepted by neurologists but is still not well known among nonneurologists. The classification divides seizures into three major categories: partial, generalized, and unclassified.4
PArTIAL SEIZuRES
Partial seizures are described as either simple or complex, depending on whether consciousness remains intact or is impaired during the seizure.5 Simple partial seizures can arise from any neocortical region. The manifestations fall into four categories: motor, sensory, autonomic, or psychic. Motor symptoms include focal myoclonus of a limb or region of the hand or face. Sensory symptoms include seeing colored spots or lines, as occurs with discharge in the primary visual cortex. A common autonomic symptom in mesial temporal lobe epilepsy is a rising epigastric sensation. Psychic symptoms may involve memory (e.g., deja vu), affect, or other complex phenomena.
In complex partial seizures, the focal discharge involves brain regions subserving awareness or spreads widely enough to reach those regions, whereby the patient loses conscious contact. Although the patient’s level of consciousness is a key component of the definition of complex partial seizures, this information may be difficult to obtain. During altered conscious contact, patients are unable to respond to commands, interact with their surroundings, or recall events that occurred during the seizure. A report of behavior observed by a witness such as a family member can be important for differentiating a simple seizure from a complex one. For example, a patient may lose the ability to speak during a simple seizure originating in the dominant temporal, frontal, or parietal cortex. However, if the patient followed commands during a seizure or recalled specific verbal information, the physician can conclude that the patient retained cognition during the seizure.
Complex partial seizures usually begin with arrest of motion and a blank stare. Automatisms (e.g., simple hand movements), oroalimentary behavior (e.g., tasting movements or swallowing), or verbal utterances may occur either initially or during the seizure. If the patient is engaged in a complex motor task at the beginning of a seizure, that activity may continue, but the accuracy of the behavior will deteriorate. Key historical points are the duration of the seizure, because most complex partial spells last only a minute or two, and the stereotyped nature of behaviors. A seizure is stereotyped when the behaviors are the same or similar for each seizure. At the termination of the seizure, the patient may be momentarily confused, fatigued, or disoriented. This alteration is of critical diagnostic importance and must be sought with leading questions by the physician. Postictal effects differentiate a complex partial seizure of temporal lobe origin from an absence seizure; in the latter, the patient does not have any postictal symptoms.7
|
Table 1 International Classification of Epileptic Seizures* |
|
Partial (Focal, Local) Seizures Simple partial seizures (consciousness not impaired) |
|
Motor signs |
|
Somatosensory or special sensory symptoms |
|
Autonomic symptoms or signs |
|
Psychic symptoms |
|
Complex partial seizures (consciousness impaired) |
|
Simple partial onset followed by impaired consciousness |
|
Consciousness impaired at onset |
|
Partial seizures evolving to generalized seizures (tonic, clonic, or tonic-clonic) |
|
Simple partial seizures evolving to generalized seizures |
|
Complex partial seizures evolving to generalized seizures |
|
Simple partial seizures evolving to complex partial seizures evolving to generalized seizures |
|
Generalized Seizures (Convulsive or Nonconvulsive) |
|
Absence seizures |
|
Typical (brief stare, eye flickering, no emotion) |
|
Atypical (associated with movement) |
|
Myoclonic seizures |
|
Clonic seizures |
|
Tonic seizures |
|
Tonic-clonic seizures |
|
Atonic seizures |
|
Unclassified Epileptic Seizures |
*From the Commission on Classification and Terminology of the International League Against Epilepsy.4
Complex partial seizures may be heralded by sensory, auto-nomic, or psychic symptoms that precede impairment of consciousness. These symptoms are referred to as an aura.
Simple and complex partial seizures may secondarily generalize and produce a tonic-clonic seizure or a convulsion. Spread of discharge from a localized focus to encompass the entire brain is common, but clinically, most partial seizures do not progress to a secondarily generalized tonic-clonic seizure.
Because the focal manifestation of a secondarily generalized convulsion may not be identified by observers or recalled by the patient, it is best to assume that a newly diagnosed generalized tonic-clonic seizure originated from a focus until such a process can be excluded.8 Focal processes to consider in an adult with new-onset partial or tonic-clonic seizures include brain tumor, cerebral infarction, or infection.
Generalized Seizures
Generalized seizures cause a spectrum of behavior from the nonconvulsive pattern of simple absence seizure through my-oclonus to the fully developed generalized tonic-clonic seizure.4 Absence seizures, which are manifestations of an epilepsy syndrome that begins in childhood, are brief, usually lasting 10 seconds or less. The seizures are not preceded by an aura or followed by postictal effects. During an absence seizure, the patient has arrest of behavior and a blank stare. Occasionally, mild clonic manifestations occur, such as subtle eyelid blinking and changes in postural tone. A specific electroencephalographic pattern of generalized spike-and-wave discharges at 3/sec occurs during absence seizures. This EEG abnormality can be activated by deliberate hyperventilation. EEGs taken between seizures (interictal) may show unrecognized absence seizures or short bursts (usually less than 3 seconds) of the generalized discharge. Patients with these abnormalities have normal intellectual and neurologic function.
Atypical absence seizures differ from simple absence seizures in that onset occurs at an earlier age in childhood, the interictal EEG background is abnormal, and the EEG discharges are slower than 3/sec. Patients with these seizures may also have atonic and myoclonic seizures. Patients with atypical absence seizures may be mentally retarded.
Myoclonus consists of brief jerks or contractions of a specific muscle or group of muscles. Hypnagogic myoclonus is both common and normal. Focal myoclonus may be caused by destructive lesions of the brain stem or spinal cord. Metabolic disease, hypoxia, toxic processes, and infectious disease may cause focal or diffuse myoclonus. Myoclonus associated with epilepsy is commonly symmetrical. Myoclonus is a component of several epilepsy syndromes and occurs before or as a part of both absence and generalized tonic-clonic seizures. One important syndrome to identify is juvenile myoclonic epilepsy (see below). Myoclonic seizures may be caused by disorders other than primary brain dysfunction; these include metabolic diseases or genetic brain disorders such as Lafora disease.
Atonic seizures involve a sudden loss of postural tone and may cause falls, with trauma to the head or body. This treatment-refractory seizure type is often associated with the Lennox-Gastaut syndrome.
Convulsions are the most common type of generalized seizures.
Table 2 International Classification of Epilepsies, Epilepsy Syndromes, and Related Seizure Disorders*
|
Localization-related (focal, local, partial) epilepsies+ |
Idiopathic |
|
Benign childhood epilepsy with centrotemporal spikes |
|
|
Childhood epilepsy with occipital paroxysms |
|
|
Primary reading epilepsy Symptomatic |
|
|
Temporal lobe epilepsy Frontal lobe epilepsy |
|
|
Parietal lobe epilepsy Occipital lobe epilepsy |
|
|
Chronic progressive epilepsia partialis continua |
|
|
Cryptogenic (presumed to be symptomatic but cause is unknown) |
|
|
Temporal lobe epilepsy Frontal lobe epilepsy Parietal lobe epilepsy |
|
|
Occipital lobe epilepsy |
|
|
Chronic progressive epilepsia partialis continua |
|
|
Generalized epilepsies |
Idiopathic |
|
Benign neonatal convulsions (familial and non-familial) |
|
|
Benign myoclonic epilepsy in infancy |
|
|
Childhood absence epilepsy |
|
|
Juvenile myoclonic epilepsy |
|
|
Epilepsy with generalized tonic-clonic seizures on awakening |
|
|
Symptomatic |
|
|
Nonspecific etiology |
|
|
Early myoclonic encephalopathy Early infantile epileptic encephalopathy with suppression burst |
|
|
Other symptomatic generalized epilepsies |
|
|
Cryptogenic |
|
|
West syndrome (infantile spasms) |
|
|
Lennox-Gastaut syndrome |
|
|
Epilepsy with myoclonic-astatic seizures |
|
|
Epilepsy with myoclonic absences |
|
|
Specific syndromes (disease states in which seizures are a presenting or predominant feature) |
|
|
Undetermined epilepsies |
Generalized and focal features |
|
Neonatal seizures |
|
|
Severe myoclonic epilepsy of childhood |
|
|
Epilepsy with continuous spike waves during slow-wave sleep |
|
|
Acquired epileptic aphasia (Landau-Kleffner syndrome) |
|
|
Other undetermined epilepsies without unequivocal generalized or focal features |
|
|
Special syndromes |
Situation-related seizures |
|
Febrile convulsions |
|
|
Isolated seizures or status epilepticus |
|
|
Seizures caused by an acute or toxic event, such as alcohol or drug overdose, eclampsia, or hyper-glycemia |
*From the Commission on Classification and Terminology of the International League Against Epilepsy.4
+Syndrome defined by seizure type and other clinical features, including anatomic localization and etiology.
They are characterized by loss of consciousness associated with apnea and violent contractions of the musculature of the trunk and extremities. Frequently, patients suffer mouth trauma and have bladder incontinence. Salivation often increases, and both pulse rate and blood pressure rise during the seizure. Most generalized convulsions begin with a tonic phase, in which there is sustained contraction of all muscles with extended legs and either flexed or extended arms. This phase lasts for several seconds and is followed by a clonic phase, in which there are rhythmic contractions of the limbs that begin with high-frequency, low-amplitude movements and then gradually decrease in frequency for several seconds to a few minutes. Some patients may have only tonic seizures or only clonic seizures. A sequence of alternating tonic and clonic movements may be observed in patients with primary generalized seizures. After the violent muscle contractions subside, the patient enters a postictal phase, in which breathing resumes and unresponsiveness is followed by gradual recovery of consciousness. The patient may remain confused for several minutes or longer and may subsequently complain of muscle pain and headache. This sequence of behavior is stereotyped, occurring regardless of cause. If a localized structural lesion in the brain cannot be found, the convulsion is an idiopathic or a primary generalized seizure. If the convulsion is preceded by a partial seizure, it is said to be a secondarily generalized seizure. About 75% to 85% of convulsions in adults are preceded by partial seizures.
Epilepsy Syndromes
In 1989, the International League Against Epilepsy recognized that many patients with seizures have brain abnormalities that affect their quality of life independent of the epilepsy alone. This classification4 recognizes that an epilepsy syndrome encompasses not only the behavior during a seizure but also the EEG changes, the patient’s mental and motor development, and the family history [see Table 2]. Because the repertoire of seizure manifestations is limited, similar seizure types may be found as components of several syndromes with widely divergent prognoses. Defining a specific epilepsy syndrome often requires repeated assessment, evaluation of development, and review of responses to treatment. Syndromes are considered to be either benign or progressive. These terms are usually applied to ultimate outcome of intellectual function and survival. Although some syndromic seizures are benign in their impact on intellectual function, lifelong treatment with antiepileptic drugs (AEDs) may be required. Five pertinent epilepsy syndromes are described in this subsection: febrile seizures, benign childhood epilepsy with centrotemporal spikes, childhood absence epilepsy, juvenile myoclonic epilepsy, and chronic progressive epilep-sia partialis continua.
Febrile Seizures
Febrile seizures affect 2% to 5% of children. These seizures typically occur before 6 years of age. Although one third of children who have a febrile seizure will have recurrent febrile seizures, only a small minority develop afebrile seizures. A syndrome called febrile seizures plus is now recognized; patients with this syndrome have febrile seizures that continue beyond 6 years of age or have associated afebrile tonic-clonic seizures. Febrile seizures plus is self-limited, with seizures typically ceasing by mid-adolescence. The syndrome appears to be genetic, with an autosomal dominant inheritance pattern. In turn, febrile seizures plus appears to be one manifestation of a broader syndrome termed generalized epilepsy with febrile seizures plus, whose spectrum of clinical manifestations also includes febrile seizures. Genetic linkage studies have mapped the syndrome to multiple loci.9,10 Patients with this syndrome may have febrile seizures in childhood, followed by a quiescent interval of many years and then the onset of seizures of a different type.
Benign Childhood Epilepsy With Centrotemporal Spikes
This common syndrome is characterized by hemifacial motor seizures that are brief, partial, usually nocturnal, and occasionally generalized. Patients also have somatosensory symptoms such as facial twitching and tongue numbness. These children develop normally and have no focal changes evident on brain imaging. The EEG shows sleep activation of high-voltage cen-trotemporal spikes, with a blunt configuration and a characteristic slow wave. Complete remission by the mid-teenage years is usual in more than 90% of cases.11
Childhood Absence Epilepsy
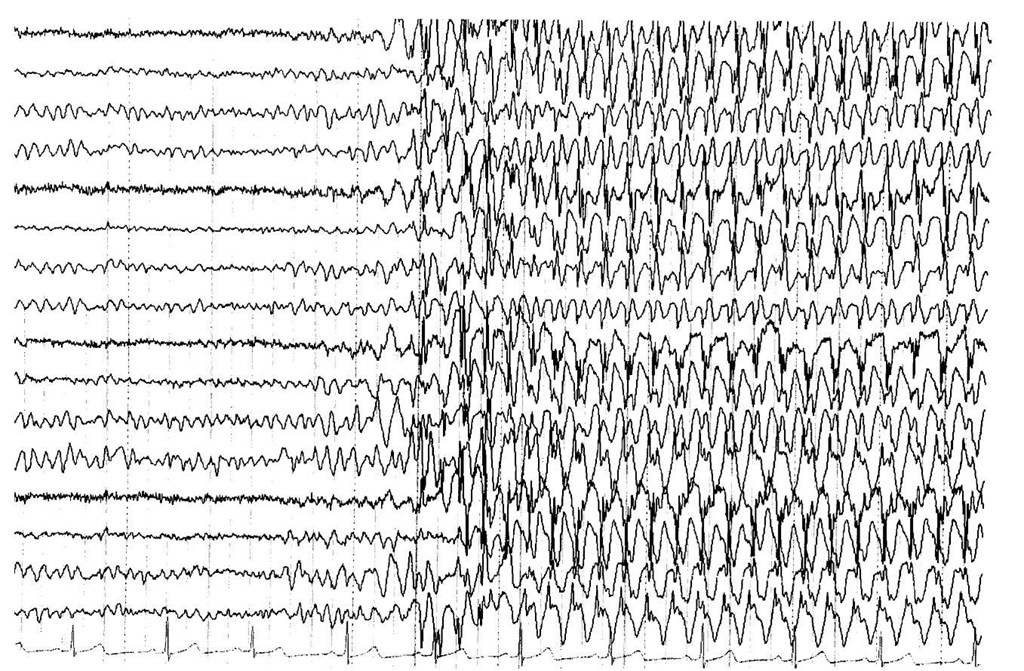
The prevalence of childhood absence epilepsy is estimated to be 2% to 8%. The associated EEG abnormality of spike-and-wave discharges at 3/sec occurs in the milieu of a normal background EEG pattern [see Figure 1].12 Remissions of 80% are reported in patients with uncomplicated absence seizures. However, tonic-clonic seizures develop in some cases, and only 30% of those patients have complete resolution without antiepileptic medication. Patients who are at least 15 years old at onset of absence epilepsy also do not have a good prognosis for complete resolution without antiepileptic medication.13 Remission is most likely with short duration of illness, which highlights the need for early identification of patients and rapid institution of treatment. Factors associated with a good prognosis are normal intelligence quotient (IQ) and no history of generalized tonic-clonic seizures. Unfortunately, tonic-clonic seizures complicate the course of absence epilepsy in about 50% of patients.11 Risk factors for development of tonic-clonic seizures include later age at onset of absence epilepsy, difficulty in controlling absence seizures with medication, and abnormal background activity on the EEG.12,14 Before the development of broad-spectrum drugs, some patients were given an additional drug to prevent tonic-clonic seizures. This dual-drug approach has been supplanted by the use of valproate, a broad-spectrum medication with combined efficacy against both absence and generalized tonic-clonic seizures. Discussion of treatment with patients and parents must include informing them of the risk of developing tonic-clonic seizures.15
Juvenile Cyclonic Epilepsy
Although the onset of juvenile myoclonic epilepsy occurs in childhood, the disorder typically persists throughout adulthood. Juvenile myoclonic epilepsy is genetically transmitted; patients typically have a family history of seizures. The genetic defect is an abnormality on the short arm of chromosome 6.
Patients with juvenile myoclonic epilepsy have characteristic myoclonic jerks, generalized tonic-clonic seizures, and photo-sensitivity that is revealed by EEG. Precipitants of seizures include sleep deprivation, stress, and alcohol use. The myoclonic jerks are quite prominent in the morning and may involve the large muscles of the legs. The correct diagnosis is important because these seizures are usually well controlled with valproate.
Figure 1 Electroencephalogram obtained from electrodes affixed to the patient’s scalp and reformatted with analog-to-digital conversion. The normal background patterns are interrupted by generalized polyspike and then spike and slow-wave discharges at 3/sec. This EEG is typical for that recorded from patients with childhood absence epilepsy. The dark vertical lines denote 1 second; the sensitivity is 7 ^V/mm.
The prognosis for normal intellectual function is usually good; however, the outlook for drug-free remission is poor.13
Chronic Progressive Epilepsia Partials Continua
Patients with partial seizures or a focal brain abnormality may experience continuous focal seizures. The EEG shows continuous focal spikes and slow waves. Prognosis is related to the underlying pathogenic lesion and is usually not associated with progression in clinical pattern. The childhood form (Rasmussen encephalitis)16 begins with focal seizures involving motor systems and then progresses to motor deficits and mental deterio-ration.11 This rare form of encephalitis also occurs in adults.
Diagnostic Evaluation
Whereas the patient’s history forms the basis for characterization of seizures, several laboratory studies are required to establish the diagnosis, management regimen, and prognosis in epilepsy. Most patients with epilepsy have more than one type of seizure. Integrating the clinical and laboratory data can allow the clinician to identify the epilepsy syndrome involved; this provides a powerful tool for patient care.
Electroencephalography
An EEG is a graphic or electronic display of amplified physiologic brain activity recorded from electrodes attached to a patient’s scalp in a standardized array. Focal or generalized seizure patterns interrupting background patterns confirm the diagnosis of epilepsy. Because sleep increases epileptiform activity, the diagnostic yield of an EEG is improved when the patient is sleep deprived, so that natural sleep will occur during the study. Patients with partial seizures arising in mesial temporal lobe structures often have a normal EEG on the initial study. Repeated EEGs are needed to obtain a confirmatory study. Diagnostic patterns include focal spikes, sharp waves, or spike-wave complexes [see Figure 2]. Generalized abnormalities range from momentary suppression of background rhythms to clusters of multiple rapid spikes to the classic pattern of spike-and-wave discharges at 3/sec characteristic of absence epilepsy.
Video-Electroencephalographic Monitoring
In most patients with epilepsy, routine EEG provides sufficient diagnostic information. In selected patients with recurrent unprovoked seizures that are refractory to therapy, the combination of video and EEG can help confirm the diagnosis of a seizure disorder and classify seizure type. In some cases, video-EEG monitoring discloses physiologic or psychological disorders that have been confused with epilepsy. Video-EEG monitoring can be performed on an outpatient basis or in an epilepsy monitoring unit.