Ankylosing spondylitis
Ankylosing spondylitis may affect the thoracic cage because of arthritic involvement of the costovertebral articulations14 [see 15:III Seronegative Spondyloarthropathies]. The chest may become relatively fixed in a hyperexpanded position, leading to an elevated midposition lung volume. The reduced compliance of the chest wall causes moderate restriction of vital capacity and total lung capacity. A typical physical finding is limited expansion of the chest wall on inspiration, despite normal findings on auscultation and percussion of the chest and normal muscle strength. Nonetheless, the alteration in function is almost never severe enough to produce symptoms, and this deformity does not produce respiratory failure.
Deformities of the sternum
Deformities of the sternum and costochondral articulations are potentially dramatic in radiographic and physical appearance and may induce psychological problems, but functional consequences are rare. There are two main varieties of deformity: pectus excavatum, an inward concavity of the lower sternum, and pectus carinatum, an outward protuberance of the upper, middle, or lower sternum.
Respiratory Compromise
Pectus deformity is present in fewer than 0.5% of the general population and appears to be more common in patients with other evidence of structural or connective tissue disease, such as scoliosis, Marfan syndrome, Poland syndrome, or Pierre Robin syndrome. In these circumstances, ventilatory function impairments may result from the underlying disease rather than the pectus deformity. For example, defects in bronchial cartilage development may lead to repeated pneumonia and result in bronchiectasis.
Treatment
In most cases of pectus deformity, no significant functional limitations are caused by the deformity. Lung volumes are preserved, and cardiovascular function is normal. Surgical correction is therefore generally restricted to patients who have severe deformity accompanied by evidence of lung restriction or cardiovascular dysfunction. Although the severity of the pectus deformity may be assessed by determining the ratio of the transverse diameter of the chest to the anteroposterior diameter as measured by computed tomography, it is not clear whether this index predicts improvement in lung function with surgery.15 A few patients with cardiac compression or with lung restriction from pectus excavatum experience functional improvement after surgical repair. Right and left ventricular end-diastolic volumes also may improve as cardiac compression is relieved.16
Surgical correction may result in modest improvements in lung volumes, ventilatory capacity, and exercise capacity in patients with severe pectus deformities but may worsen the condition of patients with good preoperative lung function.17,18 Surgical correction for only cosmetic reasons may be associated with worsening of lung function. New surgical techniques are being developed that may improve outcome.19
Flail chest
Flail chest is an acute process that may lead to life-threatening abnormalities of gas exchange and mechanical function. Stability of the thoracic cage is necessary for the muscles of inspiration to inflate the lung. In flail chest, a locally compliant portion of the chest wall moves inward as the remainder of the thoracic cage expands during inhalation; the same portion then moves outward during exhalation. Consequently, tidal volume is diminished because the region of lung associated with the chest wall abnormality paradoxically increases its volume during exhalation and deflates during inhalation. The result is progressive hyp-oxemia and hypercapnia. Multiple rib fractures, particularly when they occur in a parallel vertical orientation, can produce a flail chest. The degree of dysfunction is directly proportional to the volume of lung involved in paradoxical motion. Patient management may be complicated by other manifestations of trauma to the chest, such as splinting of ventilation because of pain, contusion of underlying lung, or hemothorax or pneu-mothorax. Positive pressure inflation of the lung or negative pressure applied to the chest wall corrects the abnormality until more definitive stabilization procedures can be undertaken.
The pathophysiologic disturbances of flail chest may also result from nonclosure of the wound after median sternotomy is performed. Any dehiscence of the sternal wound will lead to separation, loss of stability, and prominent inward motion during inspiration. The magnitude of the inward motion is directly related to the extent of the sternal separation and to the degree of negativity of inspiratory intrathoracic pressures. This condition is often the cause of difficulty in weaning a patient from mechanical ventilatory support after major cardiac surgery.
Other, rare causes of localized chest wall instability include destruction of the ribs from malignant disease (e.g., multiple myeloma) or from metabolic disorders (e.g., osteitis fibrosa cystica).
Neuromuscular Disorders That Affect Respiratory Function
Processes that interfere with the transfer of central neural output to the muscles that expand the rib cage, such as abnormalities of the spinal cord, peripheral nerves, neuromuscular junctions, or muscles, can lead to ventilatory impairment. Whereas central control problems allow creation of adequate inspiratory pressures by voluntary efforts [see 14:VI Ventilatory Control during Wakefulness and Sleep], central neural output abnormalities are characterized by an inability to generate normal respiratory pressures, either automatically or intentionally. Some diseases, such as poliomyelitis, can involve both the central controller and the peripheral neuromuscular apparatus.
Overview of Neuromuscular Disorders Affecting Respiration
Pathophysiology
Several factors are common to the neuromuscular disorders of the thoracic cage. The respiratory midposition volume is maintained at near-normal levels, whereas total lung capacity decreases (because of inspiratory muscle weakness) and residual volume increases (because of expiratory muscle weakness). Vital capacity is diminished along with maximal static inspiratory pressure.
Because muscle strength and vital capacity can be substantially diminished without causing respiratory failure, the presence of respiratory failure with hypoxemia and hypercapnia indicates either extreme progression of the primary process or the effects of complications such as atelectasis caused by retained secretions from ineffective cough, pneumonia, or pulmonary thromboembolism. Onset of hypoxemia, hypercapnia, or both in the presence of reasonable inspiratory muscle function suggests the presence of a complication rather than progression of the primary process. In the acute setting, the need to distinguish between a complication and progression makes monitoring of maximal static inspiratory pressures (which assesses muscle strength) superior to measuring serial vital capacity, because vital capacity may be diminished by either a complication or progression.
Neuromuscular disorders that persist for months are associated with chronic decreases in compliance of both the chest wall and the lungs. It is unknown whether the decreases in lung compliance are the result of microatelectasis, altered surfactant, or mild fibrotic changes resulting from recurrent infections. Venti-lation-perfusion mismatch occurs in the lungs of patients with these disorders and may lead to hypoxemia that is disproportionate to the degree of hypoventilation. Decreases in chest cage compliance have been attributed to gradual stiffening of the cos-tochondral and costovertebral articulations and to fibrotic changes or spasticity of the muscles of the rib cage.
The diminution in lung volume that occurs in chronic neuro-muscular disorders is caused by the combined effects of muscle weakness and secondary alterations in the mechanical properties of the lung and chest wall. Hence, for patients with chronic disease, measurement of vital capacity is a more accurate indicator of the total impact of the disorder than is maximal inspiratory pressure. Attempts to improve lung compliance by periodic hyperinflations with intermittent positive pressure breathing have usually not proved successful.
In contrast to the mechanical disorders of the thoracic cage, which preserve an effective cough, expiratory muscle weakness in the neuromuscular disorders prevents generation of sufficient expiratory velocities for a forceful cough. The extreme example is cervical spinal cord injuries in which paralysis of the abdominal and intercostal muscles severely reduces but does not eliminate spontaneous cough. Ineffective or absent cough eliminates a first-line defense against respiratory tract infection and is particularly troublesome when combined with airway mucus hyper-secretion, as occurs in asthma or chronic bronchitis. Pneumonia followed by respiratory failure is a common cause of death in patients with neuromuscular syndromes.
Respiratory Compromise
Patients with neuromuscular disorders must be awake to maintain ventilation. During sleep, hypoxemia and hypercapnia develop or worsen and may contribute to complications such as cor pulmonale. The degree of hypoxemia that develops with sleep is related to the severity of the abnormalities in lung mechanics and to the degree of derangement in gas exchange that is present while the patient is awake.
In the absence of major complications, the patient with neuro-muscular involvement is often disproportionately tachypneic in relation to the decrease in tidal volume. The resulting increase in minute ventilation more than offsets the increase in dead space ventilation. Thus, early in the course of the illness, PaCO2 is often low. The basis for the tachypnea may be microatelectasis, which also accounts for mild arterial hypoxemia. Microatelectasis probably develops because of the patient’s inability to take intermittent deep breaths or sighs, which results in changes in alveolar surface forces. As weakness progresses, tidal volume decreases, dead space ventilation increases, and alveolar hypoventilation with worsening hypoxemia ensues [see Table 1]. The decision whether to treat with mechanical ventilatory support must then be made. Long-term results depend on the nature and prognosis of the neuromuscular process and on the potential success of a specific therapy.
Treatment
Whether the primary disorder is acute (e.g., Guillain-Barre syndrome), intermittent (e.g., myasthenia gravis), progressive (e.g., amyotrophic lateral sclerosis), or chronic (e.g., quadripleg-ia), onset of a pulmonary complication and the accompanying increase in mechanical load and decrease in gas-exchanging ability may precipitate overt and life-threatening respiratory failure [see Table 3]. Because the patient is unable to produce an effective cough, even minor causes of increased airway secretions, such as a viral tracheobronchitis, may lead to major respiratory compromise. Maintenance of bronchopulmonary drainage and the early treatment of infections are essential for avoidance of complications. Acute episodes precipitated by such complications usually respond well to specific treatment plus supportive measures, including bronchopulmonary drainage and mechanical ventilation.
Diaphragmatic paralysis
In the absence of respiratory complications, neuromuscular syndromes rarely progress to the point of hypercapnic respiratory failure unless diaphragmatic weakness or paralysis is present. Thus, quadriplegic patients who have a preserved phrenic nerve and diaphragmatic function (e.g., C7 spinal cord transection) almost never progress to hypercapnic respiratory failure unless a major pulmonary complication supervenes or CNS-depressant drugs are administered. Because diaphragmatic paralysis or paresis uniformly accompanies hypercapnic respiratory failure caused by any of the neuromuscular syndromes, it is not usually considered apart from these disorders. However, because certain forms of diaphragmatic paralysis have distinguishing clinical features, they are best considered as discrete entities.
Bilateral Diaphragmatic Paralysis
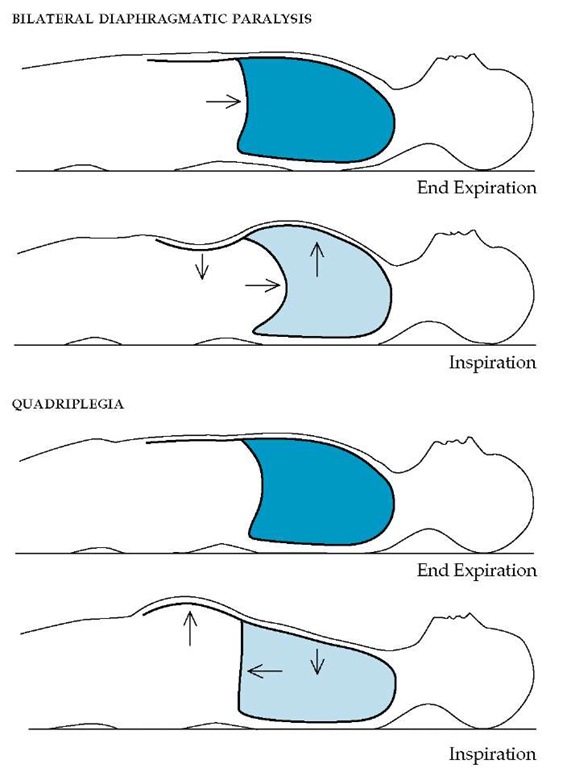
Respiratory compromise Bilateral phrenic nerve interruption or injury may result in an isolated partial or complete diaphragmatic paralysis. Causes include cervical and thoracic surgery, cold cardioplegia for cardiac surgery,21 trauma, multiple sclerosis, and neuralgic amyotrophy.22 Orthopnea may be a prominent symptom. With the patient supine, the hydrostatic force of the abdominal contents pushes the patient’s diaphragm into the thorax. Negative intrapleural pressures generated by the accessory muscles cause the diaphragm to be sucked further into the thorax during inspiration, producing a paradoxical inward motion of the upper abdomen as the thorax expands [see Figure 3]. As a result, mechanical and gas exchange abnormalities similar to those seen in flail chest develop. In the upright position, patients often experience a dramatic increase in vital capacity, improvement in gas exchange, and alleviation of symptoms because the weight of the abdominal contents offsets the negative in-trapleural pressures and, therefore, the diaphragm no longer ascends with inspiration. Despite improvements in lung function when in the upright position, patients with bilateral diaphragm paralysis experience a significant reduction in exercise capacity.
Table 3 Neuromuscular Syndromes Associated with Respiratory Failure
|
Site of Lesion |
Disorder |
|
Spinal cord |
Quadriplegia |
|
Amyotrophic lateral sclerosis |
|
|
Poliomyelitis |
|
|
Spinal muscular atrophies |
|
|
Peripheral nerves |
Guillain-Barre syndrome |
|
Diphtheritic neuropathy |
|
|
Neuromuscular junctions |
Myasthenia gravis |
|
Eaton-Lambert syndrome |
|
|
Botulism |
|
|
Drug-induced weakness |
|
|
Muscles |
Muscular dystrophies (e.g., Duchenne dystrophy, myotonic dystrophy) |
Treatment Sleeping in an upright position or nocturnal use of a thoracoabdominal cuirass negative-pressure device can facilitate breathing during sleep. In a limited study, bilateral plication of the diaphragm resulted in improved lung function and allowed patients to sleep in a supine position.24 The bilateral diaphragmatic pacemaker, although expensive and time consuming to place and stabilize, is an alternative for selected patients.
Unilateral Diaphragmatic Paralysis
Unilateral diaphragmatic paralysis is most often detected as an asymptomatic radiographic finding. The paralyzed hemidi-aphragm maintains its normal contour but is displaced cepha-lad. On fluoroscopy, the paralyzed hemidiaphragm may descend slightly on normal inspiration, mimicking normal contraction. However, with a sudden forceful inspiration (so-called sniff test), the paralyzed portion of the diaphragm ascends further into the thorax, opposite to the direction of the normally functioning side. It is driven cephalad by the sudden increase in in-tra-abdominal pressure and the sudden fall in intrathoracic pressure occasioned by the sniff. Thus, a fluoroscopic sniff test helps confirm the diagnosis of unilateral diaphragmatic paralysis.
Most cases of unilateral diaphragmatic paralysis are the result of neoplastic invasion of the phrenic nerve. Compression or destruction of the phrenic nerve by surgery, trauma, or enlarging lymph nodes or aneurysmal vessels may also cause the condition. Idiopathic cases, which may stem from an isolated phrenic neuropathy or acute infectious neuritis, appear to be evenly divided between the right and left sides and are usually permanent. Reversible paralysis is a rare complication of acute pneumonia and more commonly follows cardiac surgery in which the phrenic nerve is transiently injured by the ice slurry used to achieve cardioplegia. A thorough history and a CT scan of the thorax usually suffice for the workup of patients with unilateral diaphragmatic paralysis.
Respiratory compromise Vital capacity and total lung capacity are reduced 15% to 20% below normal levels with the patient upright and are reduced significantly more with the patient supine. A modest degree of reduction in exercise capacity is also seen.23 Nonetheless, in the absence of associated pleuropul-monary disease, most adult patients with unilateral diaphragmatic paralysis but without a coexisting pulmonary disease remain asymptomatic.
Treatment Infants are more dependent than adults on bilateral diaphragm function for adequate respiratory pump function because their more deformable chest wall moves inward with inspiration along with the paralyzed hemidi-aphragm. Plication of the diaphragm may be necessary to prevent flail motion in infants with ventilatory failure associated with unilateral diaphragm paralysis. Plication may also improve the lung function of symptomatic adults with unilateral diaphragmatic paralysis.
Figure 3 In a supine patient with bilateral diaphragmatic paralysis (top), at end expiration the weight of the abdominal contents forces the paralyzed diaphragm cephalad. With inspiration, only the accessory muscles contract, elevating the anterior chest wall, creating a negative intrathoracic pressure, and forcing the diaphragm further cephalad. The result is a paradoxical inward motion of the abdominal wall with inspiration. The diaphragm of a supine patient with quadriplegia caused by a spinal cord injury at or below the level of C4 (bottom) contracts and descends normally on inspiration, causing the anterior abdominal wall to protrude. However, because the paralyzed intercostal muscles fail to stabilize the rib cage, the anterior chest wall is pulled paradoxically inward during inspiration by the negative intrathoracic pressure generated by the diaphragm.
Postoperative Diaphragmatic Dysfunction
A transient form of diaphragmatic dysfunction occurs after upper abdominal surgery. In the hours after surgery, lung volumes and maximal inspiratory pressures fall and A-aDO2 increases. At the same time, tidal volume decreases and respiratory frequency increases. These changes may be caused by irritation of the diaphragm that produces reflex inhibition of phrenic nerve function. As a result of postoperative diaphragmatic dysfunction, atelectasis and hypoxemia occur. Deep breathing that focuses on inspiratory effort, possibly facilitated by incentive spirometry or by direct encouragement, may alleviate these abnormalities.
Spinal cord syndromes Functional Transection
Functional transection, most often caused by trauma from motor vehicle or diving accidents, must be at or below the level of the C4 cervical nerve segment if the patient is to survive. If tran-section occurs above this level, the diaphragm ceases to function and breathing stops. For the quadriplegic patient, breathing is maintained solely or predominantly by the diaphragm.
Respiratory compromise The degree of compromise of lung function is directly related to the level of injury.26 Patients with mid- to low-cervical injury are completely dependent on diaphragmatic function, producing problems with several aspects of breathing. Because the diaphragm is active only during inspiration, cough—which requires activity by expiratory muscles, including those of the abdominal wall—is almost totally absent. Intercostal muscles are required to stabilize the upper rib cage against inward collapse when negative intrathoracic pressures are produced by descent of the diaphragm. Thus, with diaphragmatic breathing alone, there is a paradoxical inward motion of the upper thorax during inspiration [see Figure 3]. The result is a diminished tidal volume for any level of diaphragmatic activation. Any sparing of the lower cervical segments allows some activity by accessory muscles and diminishes paradoxical motion. Paradoxical motion also diminishes as the condition becomes chronic because of stiffening of the thorax. In patients with injuries of the thoracic spine, inspiratory function is preserved, but expiratory function proves difficult because of abdominal muscle weakness.
Treatment When the quadriplegic patient is upright, the weight of the abdominal contents pulls on the diaphragm, and because abdominal muscle tone has been lost and cannot provide restraining action, diaphragmatic shortening ensues. Thus, the diaphragm is less effective with the patient in this position, and platypnea may result. Abdominal binders serve to replace lost abdominal muscle tone and should be used whenever tidal volume falls with the patient upright. An inflatable anterior air bladder in the binder may be used to assist ventilation in patients with marginal respiratory function. External abdominal compression may be used to help these patients cough. Quadriplegic patients have a mild degree of bronchial hyperresponsiveness caused by parasympathetic tone from the uninjured vagus nerve that is unopposed by sympathetic tone from the spinal cord.27 Use of an anticholin-ergic bronchodilating agent or a beta2-adrenergic agonist will reverse this abnormality.28 Inspiratory muscle training with a resistive device can improve lung function and reduce dyspnea in these patients.29
Respiratory failure almost never occurs in quadriplegic patients in the absence of a complication such as pneumonia, atelec-tasis, septicemia, or pulmonary thromboemboli; therefore, mechanical ventilation is required only during such complications.
Anterior Horn Cell Disease
Amyotrophic lateral sclerosis Anterior horn cell disease is most commonly seen in patients with amyotrophic lateral sclero-sis30 [see 11:IV Cerebrovascular Disorders]. Although the disease causes weakness of the muscles of breathing and an associated restrictive abnormality in most patients, only a minority of patients have respiratory symptoms at presentation. Respiratory failure may not be seen until an episode of bronchitis or aspiration pneumonia produces an acute event.
Supportive measures administered during the acute event often return the patient to a stable condition. In most patients, however, respiratory failure caused by diaphragmatic involvement proves fatal within 3 to 4 years of the onset of symptoms.
Poliomyelitis Sporadic cases of poliomyelitis still occur in the United States. When anterior horn cells involving innerva-tion of the diaphragm are affected, the patient may require ventilatory support, either continuously or during acute pulmonary events.
Spinal muscular atrophy Spinal muscular atrophy represents a heterogeneous collection of heredofamilial disorders that primarily involve spinal motor neurons. Patients with the slowly progressive infantile form, Werdnig-Hoffmann disease, may survive until late childhood. With the onset of a rapid growth phase during puberty, kyphoscoliosis develops and complicates the muscle weakness associated with these disorders.
Disorders of the peripheral nerves
Guillain-Barre Syndrome
Respiratory insufficiency that requires artificial ventilation develops in 20% to 25% of patients with Guillain-Barre syndrome25 [see 11:11 Diseases of the Peripheral Nervous System]. Duration of ventilatory support averages 2 months, but periods of up to 30 months have been reported.31,32 Approximately 30% of patients, however, can be extubated within 2 weeks. Mortality is less than 5%; the majority of survivors recover completely. A small minority may have persistent weakness and may be susceptible to recurring episodes of respiratory failure in association with respiratory infections. The chronic form of demyelinating polyneu-ropathy may account for some of these persistent abnormalities [see 11:11 Diseases of the Peripheral Nervous System].
Toxin-Induced Neural Dysfunction
Peripheral nerve function may also be impaired by toxins from algae or plankton. Certain fish (grouper and snapper) or shellfish consume and concentrate toxins that may in turn be consumed by humans. Although many of the shellfish-related toxins have been associated with respiratory failure, mortality has been highest in connection with the ingestion of puffer fish, a delicacy in Japan.
Diphtheria
Cardiac and neural toxicity occurs in approximately 20% of cases of diphtheria [see 7:1VInfections Due to Gram-Positive Bacilli]. Clinical features and management of the neurologic syndrome are similar to those of Guillain-Barre syndrome.
Disorders of Neuromuscular Transmission
Myasthenia Gravis
Myasthenia gravis is the most common disorder affecting neuromuscular transmission. Respiratory failure may occur during myasthenic crisis (acute episode of the basic disease process) or cholinergic crisis (increased weakness caused by an excess of anticholinergic medication), or it may occasionally follow initiation of glucocorticoid therapy. In patients with long-standing myasthenia, myopathy with severe diaphragmatic paresis may develop and lead to chronic respiratory failure. The principles of respiratory monitoring and ventilatory support for myasthenia are similar to those for the other neuromuscular syndromes.33
Myasthenic Syndrome
The myasthenic (Eaton-Lambert) syndrome may be confused with myasthenia gravis. As with other paraneoplastic syndromes, there may be coexistent cerebellar ataxia or carcinoma-tous neuropathy. The prognosis is not good, and respiratory failure may occur as a terminal event.
Drug-related Muscle Paralysis
Paralysis lasting several hours can occur after a single dose of succinylcholine in patients with reduced functional pseudo-cholinesterase, as seen in those with severe liver disease, myxedema, or malnutrition; pregnant patients; and patients with a genetic deficiency. A syndrome of prolonged muscle paralysis or weakness can develop after the extended administration of postsynaptic paralytic agents to facilitate mechanical ventilation, especially in patients with renal failure.
A number of other commonly used drugs can interfere with neuromuscular transmission. The mechanism can involve anesthetic-like action at the presynaptic level (e.g., with clindamycin or propranolol), postsynaptic curarelike action (e.g., with lin-comycin, polymyxin B sulfate, chloroquine, or procainamide), or stabilization of postsynaptic membranes (e.g., with gentamicin, streptomycin, or neomycin).35 Delayed recovery from anesthesia and difficulty in withdrawing a patient from ventilatory support should suggest a possible drug effect. Patients affected by these drugs often have mild or latent myasthenia; occasionally, concurrent electrolyte disturbances, such as hypokalemia, hypocal-cemia, or hypomagnesemia, combine with drug effects to produce contributory muscle weakness in myasthenic patients. In severe cases, especially those involving antibiotic-induced postoperative muscle weakness, respiratory failure can ensue; venti-latory support, correction of associated electrolyte disturbances, and withdrawal of the drug usually lead to recovery.
Botulism is an uncommon condition caused by ingestion of a polypeptide toxin produced by Clostridium botulinum [see 7:V Anaerobic Infections]. In addition to specific therapy, careful monitoring and provision of ventilatory support in the event of respiratory failure are required.
Disorders of the muscles
A number of muscle disorders can produce respiratory abnormalities. Patients with mitochondrial myopathy can present with unexplained dyspnea.36 A specific abnormality of the diaphragm thought to be myopathic can occur in patients with systemic lupus erythematosus, producing the so-called shrink-ing-lungs syndrome.37 Patients with pseudohypertrophic (Duchenne) dystrophy, myotonic dystrophy, and other forms of muscular dystrophy have a more severe disorder and are predisposed to pulmonary complications, and respiratory failure is a frequent cause of death.38,39 Chronic alveolar hypoventilation caused by inspiratory muscle weakness may develop late in the course of a disease. Expiratory muscle weakness impairs cough in some patients, and accompanying weakness of the muscles of deglutition often leads to aspiration of food, which may precipitate acute deterioration. Chronic alveolar hypoventilation may also develop in patients with adequate muscle strength, which suggests that their disease may involve a defect in central control mechanisms. As with all neuromuscular syndromes, CNS-de-pressant drugs should be avoided whenever possible or given in minimal doses when necessary. Inspiratory muscle training may delay the onset of chronic respiratory failure.40 Nocturnal ventilation with noninvasive techniques, such as nasal intermittent positive pressure ventilation or external negative pressure ventilation, may be useful in the later stages of these diseases.41