The cutaneous manifestations of systemic diseases are so numerous and varied that a single topic could not cover them all, even in a cursory way. Instead, this topic reviews key cutaneous manifestations of systemic diseases that should be recognized by most physicians, and it highlights recent developments in the diagnosis and management of such disorders. For fuller discussions of specific diseases, including their cutaneous manifestations, readers are referred to the topics devoted to these conditions.
In many of the disorders presented in this topic, workup and therapy of the underlying systemic condition are essential to a favorable outcome. A finding of cutaneous sarcoidosis, for example, should prompt a search for systemic sarcoidosis. In other conditions—for example, recessive dystrophic epidermolysis bullosa—treatment of the skin disorder is key to the management of the systemic disease.
Cardiopulmonary and Vascular Diseases
Sarcoidosis
The cutaneous manifestations of sarcoidosis are as varied as its systemic manifestations [see 14:V Chronic Diffuse Infiltrative Lung Disease]. Papules around the eyes or nose are most characteristic. The term lupus pernio refers to noncaseating granulo-mas that result in translucent, violaceous plaques of the ears, cheeks, and nose [see Figure 1]. Involvement of underlying bone can occur. Diagnosis is made by skin biopsy. Treatment with in-tralesional corticosteroids is traditional, and oral antimalarials and methotrexate have been used with success. More recently, infliximab has been successfully used for the treatment of sar-coidosis.1 Other tumor necrosis factor-a (TNF-a) blockers such as etanercept have been used to successfully treat arthritis and skin lesions associated with sarcoidosis.2 Infliximab has also been used to treat lupus pernio.
There has been an increase in the use of interferon for the treatment of hepatitis C and multiple sclerosis, and a number of reports of sarcoidosis have been attributed to this treatment. In-fliximab therapy has been found to effect a response in these cases.
In some patients with sarcoidosis, erythema nodosum, characterized by deep, tender erythematous nodules, occurs on the lower extremities. Lupus pernio is associated with a more chronic course of sarcoidosis, whereas erythema nodosum indicates a more acute and benign disease.
Granulomatous vasculitis
Wegener Granulomatosis
Wegener granulomatosis is associated with both distinctive and nonspecific mucocutaneous signs. Palpable purpura is one of the most common skin findings, but ulcers, papules, nodules, and bullae have also been described. In addition to upper and lower pulmonary symptoms [see 14:IV Focal and Multifocal Lung Disease], saddle-nose deformity, nasal ulcerations, and septal perforation should suggest the diagnosis of Wegener granulo-matosis. Definitive diagnosis is made by demonstrating a necro-tizing granulomatous vasculitis in a patient with upper and lower respiratory tract disease and glomerulonephritis. Cyto-plasmic antineutrophil cytoplasmic autoantibodies (c-ANCA) are often present. Standard therapy is with cyclophosphamide and corticosteroids. TNF-a blockers have proved to be effective for some patients with refractory Wegener granulomatosis.6
Lymphomatoid Granulomatosis
Lymphomatoid granulomatosis is a rare, destructive, angio-centric disorder that results from Epstein-Barr virus-associated B cell lymphoproliferative disease.7 This condition can be associated with skin lesions. Typically, patients develop erythematous papules or nodules that may or may not ulcerate.8 This disorder is clinically distinguishable from Wegener granulomatosis by the absence of upper respiratory tract involvement. Diagnosis is established by demonstrating a granulomatous necrotizing infiltrate with atypical lymphoid cells around blood vessels. Lym-phomatoid granulomatosis is usually fatal; however, rituximab has been used successfully to treat this condition.9
Churg-Strauss Syndrome
Churg-Strauss syndrome, or allergic granulomatous angiitis, most commonly presents as asthma and eosinophilia; however, related skin lesions develop in up to 40% of patients. Symmetrical, palpable purpura and petechiae of the lower extremities are the most common findings; these lesions show a leukocytoclas-tic vasculitis on skin biopsy. Cutaneous nodules caused by ex-travascular necrotizing granulomas and papules of the elbows also occur.10 One of the clues to the diagnosis of this disorder is the presence of perinuclear antineutrophil cytoplasmic antibodies (p-ANCA).11
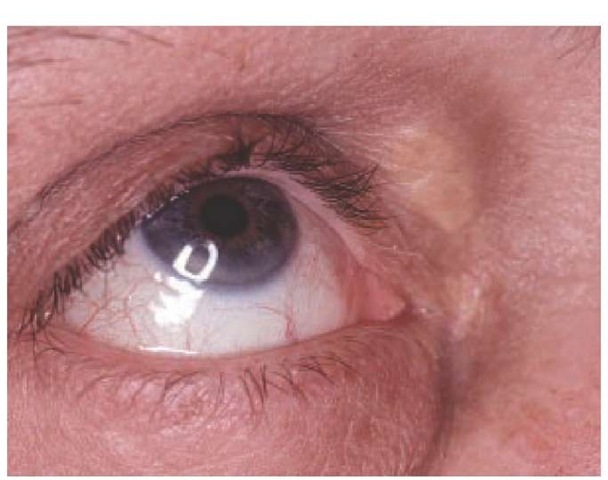
Figure 1 Characteristic facial lesions of sarcoidosis, called lupus pernio, are shown.
Figure 2 Xanthelasma and arcus senilis are shown in a patient with hypercholesterolemia.
Hyperlipoproteinemia
Xanthomas are cutaneous manifestations of hyperlipoproteinemias. Several types of xanthomas occur with different lipid abnormalities. Xanthelasmas of the eyelids [see Figure 2] are the most common manifestations of familial hypercholesterolemia; however, in at least half the people who have eyelid lesions, plasma lipid levels are normal. Planar xanthomas are flat yellow plaques that can involve the palms, soles, neck, and chest. They can occur in patients with primary biliary cirrhosis or multiple myeloma. Tuberous xanthomas are large yellow or red nodules that appear on the extensor surfaces of joints, such as on the elbows and hands, but are not attached to underlying tendons. They can occur in patients with elevated triglyceride or cholesterol levels. In contrast, tendinous xanthomas, which can appear in patients with familial hypercholesterolemia, are fixed to underlying tendons of the elbows, ankles, knees, and hands. Eruptive xanthomas occur when plasma triglyceride levels suddenly become elevated. Skin lesions consist of small yellow papules that often resolve with lowering of triglyceride levels.
Kawasaki disease
Kawasaki disease, also called mucocutaneous lymph node syndrome [see 15:VIII Systemic Vasculitis Syndromes], is a disorder in children that can be complicated by coronary artery occlusion and myocardial infarction, coronary artery aneurysms, ECG abnormalities, cardiac arrhythmias, or myocarditis.12 It has been suggested that a toxin secreted by Staphylococcus aureus is responsible for this disease, but proof of the precise cause remains elusive.13 Diagnosis is based on clinical criteria that include fever, conjunctivitis, lymphadenopathy, and rash. In addition to a generalized erythematous eruption, abnormalities of the oral mu-cosa, as well as swelling and erythema of the hands and feet, may develop. Striking desquamation of the palms and soles ultimately occurs. Perianal and scrotal erythema and scaling are common as well. Thrombocytosis is a late finding, with platelet counts increasing to more than one million over 2 weeks after the onset of the disease. Approximately 15% to 25% of untreated children develop coronary artery aneurysms that may lead to sudden death.14 Treatment with intravenous immunoglobulin reduces the frequency of coronary artery abnormalities.15
Pseudoxanthoma elasticum
Pseudoxanthoma elasticum (PXE) is an autosomal recessively inherited disorder of elastic tissue caused by mutations in the ABCC6 transporter protein.16 PXE is associated with a wide array of systemic manifestations. Angioid streaks, the ocular hallmark of PXE, are breaks in the Bruch membrane. Retinal bleeding and vision loss commonly occur. Calcification of the internal elastic laminae of arteries can result in bleeding or occlusion of these vessels. As a result, patients develop intermittent claudication on walking and occlusive coronary artery disease at an early age. Cardiac valvular abnonnalities have also been described.17 Skin lesions consist of yellow xanthomalike macules, papules, or redundant folds of skin in flexural areas, particularly the neck and axillae [see Figure 3]. Some patients may have systemic manifestations of PXE without clinically apparent skin lesions.18 Diagnosis is established by biopsy of scar or normal-appearing flexural skin.10 There is no therapy for the skin lesions associated with PXE.
Rheumatic fever
The two cutaneous manifestations of rheumatic fever are erythema marginatum and subcutaneous nodules. Erythema mar-ginatum is a transient faint annular erythematous rash that often develops over joints [see Figure 4]. The subcutaneous nodules that appear with rheumatic fever are nontender, freely movable nodules measuring approximately 1 cm in diameter; they occur on the extensor surfaces of elbows, hands, or feet.
Yellow nail syndrome
Yellow nail syndrome is caused by an abnormality of lymphatics [see Figure 5]. Affected patients develop lymphedema, usually of the legs, and pleural effusions. Pulmonary symptoms such as recurrent bronchitis are also common. Diagnosis is made by finding evidence of abnormal lymphatic function associated with yellow nails without other causes of nail pathology. Increased microvascular permeability with leakage of proteins may play a role in the development of the yellow nail syndrome.20
Endocrinologic Diseases
Diabetes mellitus
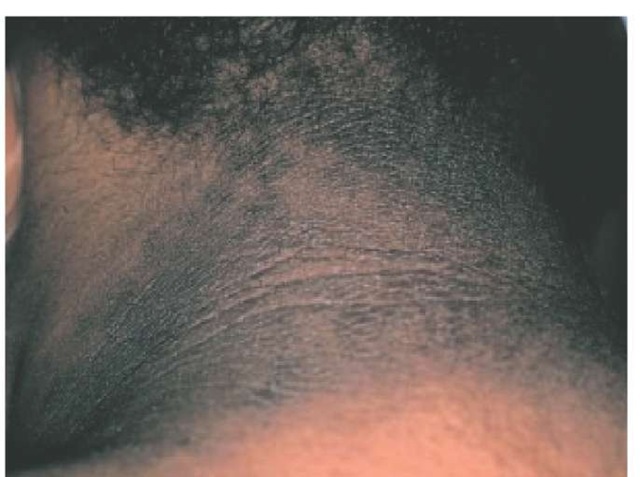
There are numerous cutaneous manifestations of diabetes mellitus [see 9:VI Diabetes Mellitus]. Acanthosis nigricans can occur in patients with diabetes and other endocrinopathies, such as Cushing syndrome, acromegaly, polycystic ovary syndrome, and thyroid disease. Insulin resistance is an underlying factor in several of the aforementioned endocrinopathies; it also may play a role in the development of acanthosis nigricans. Skin lesions consist of brown velvety patches in intertriginous areas, especially the neck and axillae [see Figure 6], and occur more commonly in obese patients with diabetes.21 Acanthosis nigricans has also been associated with internal malignancies, particularly gastric adenocarcinoma or other gastrointestinal adenocarcinomas.
Necrobiosis lipoidica is a specific cutaneous manifestation of diabetes. Lesions consist of chronic atrophic patches with enlarging erythematous borders. The legs are most commonly affected. The centers of the lesions appear yellow because of subcutaneous fat that is visible through the atrophic dermis and epidermis. Occasionally, the lesions ulcerate. Necrobiosis lipoidica is often associated with diabetic nephropathy or retinopathy.22
Scleredema, another manifestation of diabetes, consists of induration of the skin of the back and posterior neck in obese patients with type 2 (non-insulin-dependent) diabetes.
Figure 3 Xanthomalike papules are characteristic of pseudoxanthoma elasticum. The neck and axillae are the most common sites of involvement.
Figure 4 Transient annular erythematous rashes (erythema marginatum) typically occur in patients with rheumatic fever.
Figure 5 Yellow nails are a sign of underlying disease of the lymphatics in patients with yellow nail syndrome.
Figure 6 Acanthosis nigricans, a dark velvety acanthosis that can occur in patients with diabetes mellitus and other endocrine disorders, often appears on the neck.
Scleredema may improve if diabetes is controlled.23 Less commonly, sclere-dema occurs in nondiabetic patients after streptococcal pharyngitis; in such patients, the disease is self-limited, resolving within 2 years of onset. High-dose corticosteroids,24 radiation,25 and ultraviolet-A1 irradiation (UVA1)26 have all been used to treat scleredema.
Diabetic bullae, neuropathic ulcers, and so-called waxy skin and stiff joints occur in patients with diabetes. In the last condition mentioned, scleroderma-like induration of the skin over the dorsal aspect of the hands prevents full flexion or extension of the proximal interphalangeal joints.
Diabetic patients are prone to a number of infections, including erythrasma, a corynebacterial infection resulting in asymptomatic reddish-brown patches in intertriginous sites, especially the groin and axillae. Patients are also prone to staphylococcal infections and frequently develop furuncles and carbuncles. Candidal infections are another risk, particularly when blood glucose levels are poorly controlled.
Graves disease
Graves disease consists of a triad of exophthalmos, hyperthyroidism, and pretibial myxedema [see 3:I Thyroid]. Pretibial myxedema presents as skin-colored nodules and plaques that extend from the pretibial area down to the dorsa of the feet. Lesions often develop after treatment of hyperthyroidism, although they can occur at any stage in the evolution of Graves disease.
Onycholysis, the separation of the nail plate from the nail bed, occurs in many patients with hyperthyroidism. Other autoimmune skin diseases, such as vitiligo and alopecia areata, are increased in patients with Graves disease. Manifestations of thyroid disease include the stigmata of hypothyroidism. Patients can develop alopecia; specifically, they can lose the lateral third of the eyebrows. Edematous thickening of the lips, tongue, and nose occur as well.