Management of Cytologic Abnormalities
Atypical squamous cells
Each year, an estimated two to three million women are diagnosed as having cervical cytology containing ASC.37,38 The majority of women with ASC do not have a clinically significant lesion. However, 5% to 17% of patients with atypical ASC cytology have CIN 2,3 confirmed by biopsy.30,39,40 A large, prospective study of routinely screened women reported that 39% of cases of high-grade squamous lesions were detected in women with ASC cytology.41
Increased age and a history of treatment of CIN have been reported to increase the risk of CIN in patients with ASC cytol-ogy.42 High viral levels of HPV types known to be associated with cervical cancer have been found to be strongly predictive of high-grade CIN in patients with ASC Pap smears.43 ASC findings suggestive of neoplastic processes carry a greater risk of high-grade lesions and carcinoma than ASC findings suggestive of reactive processes.
Management Options
The evaluation and management of women with ASC-US cytology is a topic of considerable controversy. The best approach to the management of abnormal cervical cytology is to use the fewest number of tests to resolve the clinical question posed by the presence of ASC. Management options include (1) repeat cytology at a designated interval, (2) high-risk HPV DNA testing, (3) immediate colposcopy, (4) a combination of repeat cervical cytology and HPV DNA testing, (5) direct visual inspection in combination with conventional cytology, (6) referral for col-poscopy, and (7) a combination of these strategies.
Repeat cervical cytology A repeat cervical cytology obtained at a later date appeals to many health care providers, because most histologic abnormalities found with ASC-US will be low-grade cervical neoplasia that is likely to regress without definitive therapy. The repeat Pap smear should be obtained 4 to 6 months after the index cytology [see Figure 1]. This is considered the optimal interval; a repeat cytology obtained after less than 4 months is thought to be associated with decreased sensitivity,40 and after 6 months, 7% of patients with ASC-US smears will have CIN 2,3.44
High-risk HPV DNA testing HPV DNA is associated with virtually all cervical cancers and high-grade precursor lesions; the identification of these types of HPV that are associated with a high risk of oncogenesis is useful in identifying patients with ASC-US who are at increased risk for neoplasia.45
The probability of HPV expression is influenced by several factors, including age, menstrual cycling, use of exogenous hormones, and immunocompetence.10,46 The addition of HPV DNA testing to cervical cytologic screening for women with ASC-US may be most effective in women 30 to 35 years of age, who are past the peak of incidence of acute infections [see Table 2].46 In women whose cytology was classified as ASC-US, those who were 30 years of age or older had a lower prevalence of HPV positivity and a lower referral to colposcopy than younger women (30% versus 65%); this improvement in specificity was not accompanied by a decrement in sensitivity. Establishing age-and population-specific analytic cutoff points for the detection of HPV may further enhance the specificity of HPV DNA testing. Other strategies for improving specificity without compromising sensitivity may include the use of serial HPV DNA testing or lengthening the interval between the index ASC-US cytology and HPV DNA testing.
Of the commercial HPV DNA detection kits, Hybrid Capture 2 (HC2) (Digene Diagnostics, Silver Spring, Maryland) has a higher sensitivity (94.8% versus 84.4% for high-grade precursor lesions) and detects a broader range of high-risk HPV types than other methods.47 HC2 is a nonradioactive, rapid assay that can detect 18 HPV DNA types,48 13 of which convey high risk of oncogenesis. A retrospective study of 398 women showed the HC2 assay to be as sensitive and specific as a single repeat cyto-logic smear for the detection of CIN.40 However, it has been argued by some that its use identifies large numbers of low-grade lesions (CIN 1) and transient HPV infections and may lead to overevaluation and overtreatment because of its low positive predictive value.47
Figure 1 A Pap smear showing atypical squamous cells of undetermined significance (ASC-US).
Immediate colposcopy Colposcopy would be expected to detect almost all of the cases of high-grade CIN, but it has drawbacks, including expense and the risk of overevaluation and overtreatment in women who do not have CIN. Immediate col-poscopy, however, may be indicated for women with a history of CIN, for poorly compliant women, and for women for whom waiting creates undue anxiety.
Studies of the natural history of HPV infection have demonstrated that most HPV infections produce only minor, transient infections.10,11 A positive HPV DNA test in combination with an ASC-US cervical cytologic finding does not indicate high-grade disease or the presence of cancer, but it does indicate some increased risk of cancer now or in the future. Because of imperfect sensitivity, the initial colposcopy and directed biopsy will not detect about 10% of those women who will have histologically confirmed CIN 2,3 within 2 years of follow-up.49
Repeat cytology and direct visualization To compensate for the low sensitivity of a single repeat cervical cytology in women with atypical squamous cells, it has been suggested that repeat cytology be combined with a visual screening method. Direct visual screening methods include cervicoscopy (direct visual inspection of the cervix after an acetic acid wash), specu-loscopy (direct visualization of the cervix under low magnification after application of an acetic acid wash), and cervicography (visual inspection of the cervix in which a static photographic image is used to document cervical abnormalities after an acetic acid wash).50 Several studies that evaluated the combined use of cervicography and repeat cytology reported that this screening approach had a high sensitivity for the detection of CIN 2,3.51,52 Because the data are limited, more studies are needed before recommending repeat cytology and direct visualization as a screening approach in patients with ASC-US.
Repeat cytology and HPV DNA testing Several studies have reported that the combination of HPV DNA testing and a repeat Pap smear has a sensitivity similar to that of colposcopy for the detection of high-grade CIN.43,53-55 The negative predictive value of DNA testing for high-risk types of HPV is generally reported to be 98% or greater.40,56 However, other investigators question the cost-effectiveness of this combined screening strategy in women with ASC-US.57,58 Use of liquid-based cytology permits the residual transport fluid to be used to test for HPV DNA (a technique referred to as reflex HPV DNA testing).39 In a large study, Manos and colleagues evaluated HPV DNA testing of residual material from liquid-based cervical cytology using the HC2 assay. An overall sensitivity of 96.9% (95% confidence interval [CI], 88.3% to 99.5%) was achieved when colposcopy of HPV DNA-positive women was performed immediately after the reflex HPV DNA test. The authors concluded that reflex HPV DNA testing of cervical cytology aids in identifying those women at risk for high-grade lesions.44
The initial report of the ASC-US/LSIL Triage Study (ALTS) found that reflex HPV DNA testing was more sensitive than a single repeat cytologic smear in detecting CIN 3 in women with ASC-US cytology.40 The sensitivity of HPV DNA testing for the detection of CIN of grade 3 or higher was 96.3% (95% CI, 91.6% to 98.8%); 56.1% (95% CI, 54.1% to 58.1%) of patients were referred for colposcopy. The sensitivity of a single repeat cytologic specimen for the detection of ASC-US or findings associated with higher risk was 85.3% (95% CI, 78.2% to 90.8%); 58.6% (95% CI, 56.5% to 60.6%) of patients were referred for colposcopy. However, the conventional clinical management strategy for cy-tologic follow-up is based on a series of repeat cytologic specimens, not on the sensitivity of a single cytologic sampling. A 2-year follow-up of the ALTS showed that a repeat cytologic specimen is as sensitive as HPV DNA testing at an ASC-US referral threshold, but this approach requires two follow-up visits and ultimately more colposcopic examinations than HPV triage (67.1% versus 53.1%).59
Reflex HPV DNA testing offers advantages over HPV DNA testing using conventional Pap smears: women do not need an additional clinical examination for specimen collection, and 40% to 60% of women with negative test results are spared a colpo-scopic examination. However, with this approach, the number of patients needing colposcopies remains high. The combination of HPV DNA testing and cervical cytology increases sensitivity at the expense of specificity, because even potentially oncogenic HPV-type infections are found in women without cervical neoplasia, particularly young, sexually active women. The positive predictive value of HPV DNA testing is similar to that of cytology (18% to 25%), but the negative predictive value is 99.8% to 100%.6062
The drawbacks of reflex HPV DNA testing lie in its tendency to produce false negative and false positive results. A screening study of cervical cytology found a substantial degree of cross-reactivity (6.4%) between the reflex HPV DNA probe and the HPV types not included on the probe; this was detected by retesting all HPV DNA-positive samples with a polymerase chain reaction (PCR) assay. The PCR retest found a significant false positive rate of 3.6% and a false negative rate of 6.1% of all samples defined by the reflex HPV DNA test.63 Thus, reflex HPV DNA testing has the potential for both overevaluation and undereval-uation of high-risk HPV infections. However, the combination of a negative reflex HPV DNA test and a negative cytology indicated the absence of CIN 3 or cancer to a certainty of 100%, with a specificity, positive predictive value, and negative predictive value of 93.8%, 8.6%, and 100%, respectively.63
Table 2 Prevalence of High-Risk HPV Infections Stratified by Age of Women at the First Examination61
|
Age |
Women (%) |
High-Risk HPV (%) |
|
< 20 |
418 (5.3) |
84 (20.1) |
|
21-30 |
1,843 (23.2) |
435 (23.6) |
|
31-40 |
2,076 (26.2) |
289 (13.9) |
|
41-50 |
1,925 (24.3) |
235 (12.2) |
|
51-60 |
1,014 (12.8) |
110 (10.8) |
|
> 60 |
656 (8.3) |
61 (9.3) |
|
Total |
7,932 |
1,214 (15.3) |
HPV—human papillomavirus
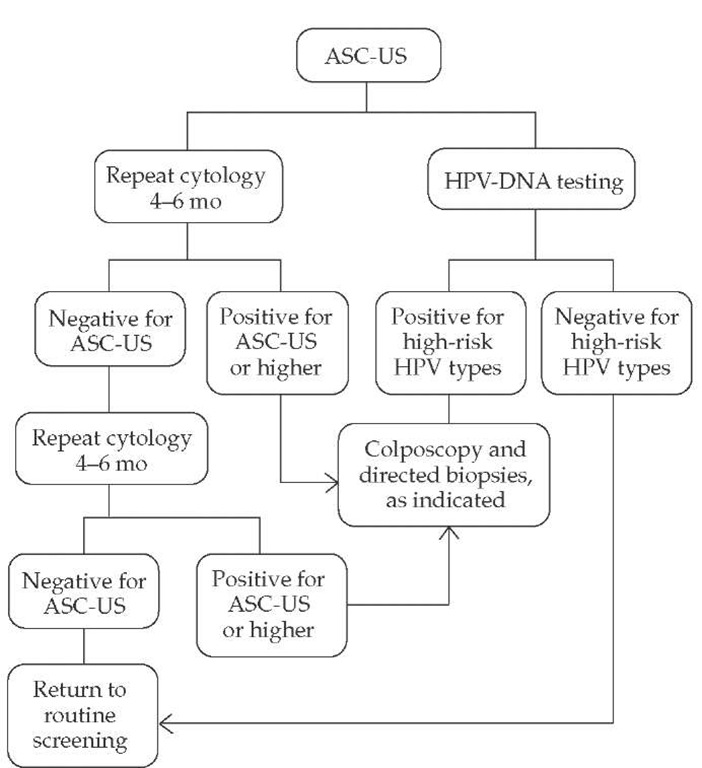
Figure 2 Management scheme for atypical squamous cells of undetermined significance (ASC-US), based on the consensus guidelines developed by American Society for Colposcopy and Cervical Pathology.64 (HPV—human papillomavirus)
Recommended Management
Different policy-making organizations vary in their recommended approaches to the management of ASC. The American Society for Colposcopy and Cervical Pathology (ASCCP) established consensus guidelines for the management of ASC in 2001. The consensus guidelines classify ASC into two groups: ASC-US and ASC-H (see above).64 For women with ASC-US cytology, a program of repeat cytologic testing, immediate colpos-copy, or DNA testing for high-risk types of HPV are acceptable management options [see Figure 2].64 When liquid-based cyto-logic is used or when cocollection for HPV DNA testing can be performed, reflex HPV DNA testing is the preferred approach. Women with ASC-US who test negative for high-risk HPV DNA should undergo repeat cytologic testing at 12 months. Women who are managed with immediate colposcopy and who are found not to have CIN should undergo repeat cytolog-ic testing at 12 months.
When a program of repeat cervical cytologic testing is used, women with ASC-US should undergo repeat cytology (either conventional or liquid-based) at 4- to 6-month intervals until two consecutive results that are negative for intraepithelial lesion or malignancy are obtained. In most instances, women with ASC-H, LSIL, HSIL, and AGC should be referred for immediate col-poscopic evaluation [see Squamous Epithelial Lesions, below].64
The National Comprehensive Cancer Network guidelines are consistent with the recommendation of the consensus guidelines.65
The Society of Obstetricians and Gynecologists of Canada (SOGC) guidelines recommend repeating the cytologic smear every 3 to 6 months until three consecutive negative smears are obtained, after which annual cytologic examinations can be resumed. If cytology continues to demonstrate ASC-US, col-poscopy should be performed.66
Management of ASC-US in Special Circumstances
Immunosuppressed women with ASC-US are at increased risk for CIN 2,3; high-risk types of HPV are frequently detected in these women. Referral for colposcopy is recommended in all immunosuppressed women who have ASC-US.64
In postmenopausal women with ASC-US, the risk of CIN 2,3 is lower than in premenopausal women. Treatment with a course of intravaginal estrogen followed by a repeat cervical cytology 1 week after therapy is an acceptable option.40 It is also acceptable to manage postmenopausal women who have ASC-US with immediate colposcopy or HPV DNA testing.
ASC-US and oncogenic hpv dna
As demonstrated by ALTS and other studies, it is now possible to identify many women with ASC-US who do not need col-poscopy. However, women who have oncogenic HPV DNA and ASC-US present a sizable management challenge. It is not known how to manage women with ASC-US who test positive for high-risk HPV DNA but who are not found to have CIN by col-poscopy and biopsy. Expert opinion and review of the literature indicate that such women are at low risk for high-grade cervical neoplasia and that repeated colposcopy should not be performed in this setting. Instead, HPV DNA testing along with repeat cytology at 6 and 12 months is recommended.27 The likelihood that these repeat tests will be negative and that patients will subsequently forgo further surveillance screening is not known.
Squamous epithelial lesions
For women with LSIL, colposcopy is the recommended man-agement.64 If the colposcopy results are negative for CIN and cancer, appropriate management entails either repeat cytology at 6 and 12 months or HPV DNA testing at 12 months; subsequent management entails (1) a repeat colposcopy if results are positive for ASC or HPV or (2) a return to routine screening if results are negative. If colposcopy reveals the presence of a lesion, the patient is managed in accordance with the guidelines recommended by the ASCCP.
For women with HSIL, colposcopy with endocervical assessment is the recommended management.64 If colposcopy reveals no lesion or only biopsy-proven CIN 1, then cytology, col-poscopy, and biopsy results should be reviewed; subsequent management depends on the final interpretation of tests. If col-poscopy indicates the presence of a lesion, the patient is managed in accordance with the guidelines recommended by the ASCCP.
Management of LSIL and HSIL may vary if the patient is pregnant, postmenopausal, or an adolescent.
Atypical glandular cells
The finding of AGC is significant because AGC is associated with a greater risk of high-grade lesions than the risk associated with ASC. On follow-up evaluation, high-grade lesions (either squamous or glandular) may be seen in 10% to 39% of patients with an AGC cytologic result35,36; in comparison, 5% to 17% of patients with atypical ASC cytology have CIN 2,3 confirmed by biopsy.
Women with atypical endometrial cells should initially be evaluated with endometrial sampling.64 If no neoplasia is identified, it is recommended that the patient undergo follow-up evaluation using a program of repeat cervical cytologic testing at 4-to 6-month intervals until four consecutive results that are negative for intraepithelial lesion or malignancy are obtained. If a result of ASC or LSIL is obtained on any of the follow-up smears, acceptable options include a repeat colposcopic examination.64 Continued follow-up evaluation is needed.