A stem cell is defined as a cell that can renew itself for the lifetime of the organism (self-renewal) while also producing cell progeny that mature into more specialized, organ-specific cells (committed progenitors). The balance between populations of stem cells and differentiating cells is critical for embryonic development and for long-term maintenance and regeneration of adult tissues. Understanding stem cell self-renewal holds great promise for therapeutic applications in regenerative medicine.
mechanisms of self-renewal
In steady-state conditions, the main molecular mechanism through which stem cells can achieve self-renewal is asymmetric division, which entails the division of a stem cell to give rise to two cells with different fates: one stem cell and one committed progenitor. This mechanism ensures that the stem cell pool (number of stem cells) remains constant during the lifetime of an organism. Self-renewal must be tightly regulated, requiring the coordination of both intracellular and extracellular factors. Intracellular asymmetry is achieved during cell division through the segregation of specific cellular components such as proteins and RNA to only one daughter cell and not to the other. Although still somewhat controversial, recent evidence suggests that the DNA itself can be distributed asymmetrically. Upon cell division, the original DNA strands are retained in the daughter stem cell, and the newly synthesized DNA is partitioned to the committed progenitor. This mechanism is thought to protect stem cells from the accumulation of mutations resulting from DNA synthesis and guarantees stem cells the exact same genome forever (immortal DNA). As a result, together with DNA, the epigenetic signature of a stem cell is inherited, including modifications to the DNA itself, as well as associated proteins (chromatin factors). This ensures that stem cell gene expression and function will be maintained over future cell generations. Extracellular asymmetry is provided by the microenvironment surrounding the stem cells (stem cell niche). The distribution of extracellular matrix components, secreted proteins, and other cells in the vicinity of the stem cells is critical to controlling the stem cell pool. For example, in the Drosophila ovary, the orientation of stem cell division is dictated by the niche. The mitotic spindle is perpendicular to the niche, so that after division, one cell remains in close contact with the niche and maintains stem cell function, and the other loses this contact and begins to differentiate into more committed progeny. Thus, the polarity of both intracellular and extracellular signals plays a crucial role in self-renewal.
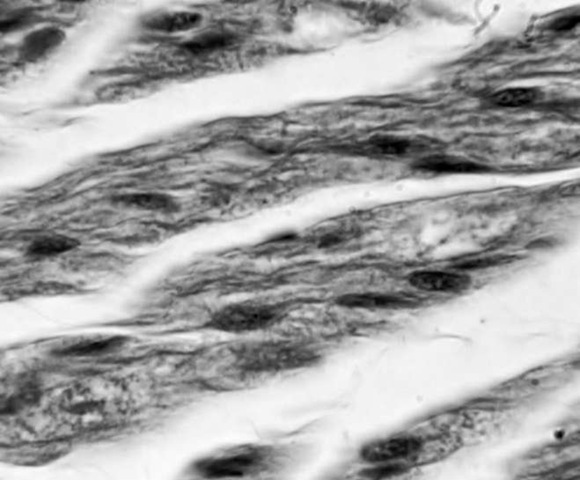
Muscle stem cells lie beneath a thin basement membrane on top of a single contractile, multinucleated muscle fiber.
Although asymmetric division occurs in homeo-static conditions and is necessary to maintain a constant stem cell pool, symmetric division is required during embryonic development and to meet the demands of tissue stress and injury. This mechanism ensures that when an acute damage severely impairs tissue function, stem cells can start dividing very rapidly to give rise to committed progenitors to guarantee the restoration of tissue function in a relatively short period of time. This leads to exhaustion of the stem cell pool (depletion). Conversely, stem cells can also divide symmetrically to give rise to more stem cells, thus expanding the stem cell pool (expansion). A third mechanism has been recently observed in mouse spermato-genesis—reversion—in which a stem cell initially divides, giving rise to two committed daughter cells (transient amplifying cells) and then, subsequently, these transient amplifying cells, when again in contact with the niche, revert to a stem cell state, thus expanding the stem cell pool. These studies underscore the importance of the niche in regulating cell fate and demonstrate the critical role of extrinsic factors in instructing cell function.
SELF-RENEWAL AND THE MICROENVIRONMENT
Removal of stem cells from their native microenvironment, for example, through isolation and cul-turing in the laboratory, results in the rapid loss of stem cells, as they lose their ability to self-renew. Both embryonic and adult stem cells reside within a highly organized microenvironment that is composed of both cellular and noncellular components. For example, the mammary stem cell micro-environment consists of contractile myoepithelial and luminal epithelial cells directly adjacent to the stationary stem cells, with proteinaceous components of the thin basement membrane encapsulating the mammary duct structures; for example, collagen, laminin, proteoglycans, and syndecans.
In addition, endothelial cells, fat cells, and the collagen they produce make up the surrounding stromal compartment. Muscle stem cells, known as satellite cells, reside beneath a thin basement membrane on top of a single contractile, multi-nucleated muscle fiber. In contrast, hematopoietic stem cells (HSCs) of the bone marrow exist as a suspension surrounded by bone cells, blood vessel cells, and differentiated blood cells, as well as growth factors, collagen, and other extracellular matrix components produced by these cells.
Proteins secreted by cells within the microenvironment (biochemical cues), as well as the rigidity or fluidity of the microenvironment (biophysical cues), can positively and negatively regulate the ability of stem cells to self-renew. During development, aging, injury, and disease, the microenviron-ment incurs numerous changes in its cellular and noncellular composition and structure that affect its potential to instruct stem cells to self-renew. Precise regulation of stem cell self-renewal is critical to allowing production of the terminally differentiated cells necessary to repair tissues while reestablishing the stem cell pool to levels permitting tissue homeostasis.
SELF-RENEWAL IN VITRO AND IN VIVO
The study of stem cell self-renewal mechanisms and regulation is dependent on the availability of stringent in vitro and in vivo experimental assays. Self-renewal assays must be able to demonstrate that a single stem cell can both differentiate into multiple cell types and be able to self-renew. Clo-nogenic assays are a common method for assaying stem cell function in vitro. In this assay, single stem cells are embedded within methylcellulose (which is similar in consistency to gelatin) and tested for their ability to differentiate and self-renew. However, stem cell behavior can change significantly on in vitro culture following loss of contact with the microenvironment, making in vivo self-renewal assays more readily accepted. The gold standard in vivo stem cell assay for HSCs is to rescue the life of a host mouse lacking HSCs by injecting it with a single purified HSC. If the single cell is a true stem cell, it will be able to replenish all the blood and immune cells of the host mouse, and it should be possible to reisolate stem cells from this host for serial transplantation into a third mouse lacking HSCs. Serial transplantation (two transplants in succession) is currently the only accepted method to assess stem cell self-renewal. Development of in vitro assays that recapitulate the in vivo microenvironment and allow for time-effective analysis of stem cell function would greatly enhance our ability to further purify stem cell populations and elucidate the molecular mechanisms regulating stem cells.
self-renewal and cancer
Cancer results from the deregulation of normal developmental processes. At present, there is debate as to whether malignant tumors are initiated and maintained by a population of tumor cells that share similar biologic properties to normal adult stem cells (cancer stem cells). Scientists demonstrated that transplantation of a small number of cells that were enriched for cancer stem cells into a host mouse without prior malignancy is sufficient to initiate cancer. These cancer stem cells are competent to self-renew because cancer stem cells can be reisolated and serially transplanted into a third healthy mouse, resulting in tumor formation. It follows that stem cells, which are critical to normal development because of their exclusive ability to differentiate into multiple cell types and to self-renew indefinitely, are considered a prime candidate as the cell type from which the cancer stem cell derives. In this scenario, a stem cell experiences certain genetic or epigenetic alterations, resulting in a cell that can still differentiate into multiple cell types and self-renew but that overrides normal intrinsic and extrinsic levels of regulation, thus becoming autonomous. Alternatively, a cancer stem cell may derive from transient amplifying cells or even terminally differentiated cells that acquire stem cell characteristics, notably, by hijacking the capacity to self-renew and thereby creating a cancer cell that renews indefinitely. Evidence suggests both scenarios can occur in a tissue- and cancer-dependent manner.
CURRENT SELF-RENEWAL RESEARCH CHALLENGES
The study of mechanisms regulating stem cell self-renewal holds many clinical advantages. Understanding the minimal signals and molecules leading to stem cell self-renewal divisions could ultimately result in the ability to culture and produce additional stem cells for therapeutic use. For example, cord blood is being stored at birth as a potential source of autologous, or immunologically matched, hematopoietic stem cells. Yet the number of cells that is appropriate and useful in a newborn does not suffice for an adult, highlighting the need for methods to increase the numbers of stem cells in culture. In addition, an understanding of the mechanisms of self-renewal may reveal novel ways to identify and specifically target cancer stem cells, facilitating destruction of solid tumors and blood malignancies at their root.
At present, self-renewal studies are hindered by two main issues. To study self-renewal of stem cells, it is imperative that researchers perform studies on a pure starting population of stem cells. This requires the availability of reliable markers that distinguish stem cells from committed progenitor cells within the same tissue. Few stem cell markers are currently available, and identification of additional markers is hindered by the lack of reliable in vitro and in vivo assays for assessing stem cell function. High-throughput culture assays would greatly aid in the identification of stem cell specific markers, which would, in turn, allow the advancement of self-renewal research, increase our understanding of stem cell biology, and enable harnessing of self-renewal mechanisms for use in the clinic.