Experimental models help researchers understand the developmental and function of a biological process. A model system in biological research refers to anything that scientists use to recreate aspects of a disease or any biological process.
The study of a biological process has made intensive use of experimental models, as performing such work in human is difficult for experimental, practical, and ethical reasons. A model can be a cell living in a dish. Or it can be used the animal models that have long played an important role in biology are both invertebrates (e.g., Drosophila, Aplysia) and vertebrates (e.g., Zebrafish, rodents, non-human primates), as well as mutant and transgenic animals that have revolutionized scientists’ ability to characterize normal, abnormal, and restorative development.
Stem cells can be clinically beneficial through a range of mechanism-encapsulated in the idea of therapeutic plasticity. The field of stem cell biology and regenerative medicine is rapidly moving toward translation to clinical practice, and in doing so has become even more dependent on animal donors and hosts for generating cellular reagents and assaying their potential therapeutic efficacy in models of human disease. Advances in cell culture technologies have revealed a remarkable plasticity of stem cells from embryonic and adult tissues, and transplantation models are now needed to test the ability of these cells to protect at-risk cells and replace cells lost to injury or disease. Stem cells can be applied to two basic experimental models. First, preliminary experiments are performed using cultured stem cells grown in dishes. These cells come from human tissue samples or from model organisms such as mice or rats. Second, refined potential stem cell therapies are tested in animal models, such as mice, rats, and non-human primates, before being used in clinical trials.
The process of developing a potential therapy starts out as a testable idea based on initial research findings. This idea must be followed up with rigorous research and testing in the lab using different experimental models, which can take years of works. Even if the therapy looks great in lab experiments, it will become a viable treatment only after it is proven safe and effective in human clinical trials.
The first step is to establish an experimental model- a laboratory-based scenario that stimulates that way a stem cell therapy might work in humans. To be useful, an experimental model must possess these features: (1) it must accurately reflect the biology of human stem cells; (2) it must be reproducible, allowing experiments to be credibly repeated; and (3) it must be time effective, allowing experiments to be completed, analyzed and repeated within a reasonable time period.
Several issues need to be considered to establish the best experimental model using stem cells for understanding developmental and function of a biological process: (1) To discover the best stem or progenitor cell in vitro protocols for isolating, expanding, and priming these cells to facilitate their massive propagation into just the right type of stem cells, and (2) To establish the best animal models of human disease and injury, using both small and large animals, for testing new regenerative medicine therapeutics.
APPLICATIONS OF STEM CELLS AS FOR EXPERIMENTAL DISEASE MODELS IN VITRO
Although many common diseases can be modeled in rodents, in many cases there animal models do not faithfully reproduce the human syndrome at either the molecular or anatomical levels. Species differences between rodents and humans might be one reason for clinical failures—rodent cells are differentially vulnerable to human transgenes and toxins compared with human cells. Human stem cells represent a renewable source of tissue that can generate target tissues. Therefore, these cells are a valuable tool of experimental disease models in vitro.
Recent remarkable advances allow us to control growth and differentiation of human stem cells that are derived from embryos, fetal, or the adult tissue. Human stem cells can be induced to differentiate into physiologically active and presumably functional cells, which occur through well-defined stages that involve waves of proliferation and maturation that are coordinated through temporal patterning in the developing tissues. These cells can be held in culture for many weeks or months for further maturation if required. Furthermore, the generation of human stem cell lines that carry mutations conferring predisposition to certain diseases will supply valuable research tools for studying by which processes the disease arise and potentially lead to the development of new therapeutic strategies.
STRATEGIES FOR DISEASE MODELING IN STEM CELLS
Several strategies can be used to introduce the gene of interest into stem cells and their progeny – the introduction of mutations by viral infections, homologous recombination, nucleus transfer from the affected patients own cells, or by prenatal diagnostics. These cells could then be differentiated into the afflicted cell type and used to study the onset and progression of the disease, screen for new drugs, and test new therapies. For example, generation of pancreatic beta cells from human embryonic stem cells that carry particular maturity-onset diabetes of the young mutation could help towards a better understanding of the development of the disease and facilitate discovery of a cure. In neurodegenerative diseases, the ability to generate large number of defined neural derivatives raises the prospect of developing in vitro disease models as reported in recent studies of human embryonic stem cells-derived neurons examining toxicity in Parkinson’s disease, Amyotrophic lateral sclerosis (ALS), Huntington’s disease, and multiple sclerosis.
Most of stem cells including human embryonic and fetal stem cells can be transduced with viral vectors that carry specific mutations in a disease-causing gene of interest. Adeno-associated virus (AAV), and lenti- and retroviral vectors can be used for this purpose. Adeno-associated virus and lentiviral vectors infect dividing and non-dividing cells, whereas retroviral vectors infect only dividing cells. Cultures of infected cells that express the gene of interest can then be expanded. The transgene can be expressed through differentiation, allowing the examination of the effects of the mutant proteins in post-mitotic cells. Stable trans-gene expression can be achieved through transgene incorporation into the genome. The culture can also be enriched for the infected cells suing selection markers such as antibiotic resistance. However, the viral transduction to deliver mutant genes to cells has limitations. For example, the rates of infection are heterogenous and insertion into the genome is random.
Homologous recombination allows site specific insertion of a gene and has been used to generate transgenic lines from mouse embryonic stem cells. This technique has recently been show to work in human embryonic stem cells, although the recombination rates are low. The power of this technique is clear, as target genes can be inserted into know parts of the human genome without the risk of disrupting areas that are crucial for normal cell function. As technology advances, it might be also possible to use homologous recombination in fetal and adult stem cells.
In addition to genetic manipulation of normal stem cell cultures, it might be also useful to isolate stem or progenitor cells from embryos or postmortem fetal tissue that carries mutations linked to specific diseases. The advantage of this approach is that the insertion site and copy number of the mutation is identical to the normal situation in humans. Although this tissue is rare and appropriate clinical screening is required for its identification, large number of cells can be obtained following in vitro expansion from a single tissue source. One limitation of this approach is that if the mutation is very severe, it might not be possible to passage the cells that carry it and the cell lines might not be fully renewable.
At present, most embryonic stem cell lines have been derived from excess embryos that are collected from couples who undergo in vitro fertilization but that are no longer required. Therefore, it is impossible to ignore the associated ethical and political issues even if we use stem cells only for experimental models. Furthermore, most of what the research community knows about the nature and behaviors of stem cells comes from in vitro studies of these cells, subjecting them to growth factor and other morphogenetic or toxic molecule concoctions that attempt to mimic as possible growth condition in vivo. But many of events that investigations observe and attempt to characterize in a dish are not perfect as they occur in life because the cells are exposed to nonphysiological amounts of potent growth factors, cytokines, and morphogens that have profound effects on their choices to divide or differentiate along a particular line. Even so, recent studies using human stem cells achieve a rather impressive level of recapitulating many of the differentiation cascades that lead to the generation of normal cell lineage diversity as it evolves in vivo.
EXPERIMENTAL MODELS TO UNDERSTAND THE BIOLOGY OF STEM CELLS
After the refinement of the in vitro models of different stem cell populations to generate cells that are homogenous as possible, it is feasible to use the results of in vitro studies for in vivo experimental models for transplantation. Stem cell therapies involve more than simply transplanting cells into the body and waiting for them to go to work. A successful stem cell therapy requires an understanding of how transplanted cells work, combined with a reliable experiment model to enduring that the stem cells perform the desired action in the body. Whether stem cells survive, and whether they can still be transplanted after manipulation will have to be tested in experimental models. Regardless of the mechanism of action of any putative intervention (cellular or pharmacological), there is a need to demonstrate pathological and functional recovery in appropriate experimental models.
Several important issues remain to be resolved before delivery of functional cell population in vivo can be accomplished, including the type and number of cells to be delivered, site of engraft-ment, prevention of abnormal tissue formation (e.g. teratoma) due to contamination of the graft with remaining undifferentiated cells, and donor/ recipient compatibility and graft rejection. Allo-geneic transplantation of stem cell-derived cells will require immunosuppression in order to avoid graft-versus-host disease.
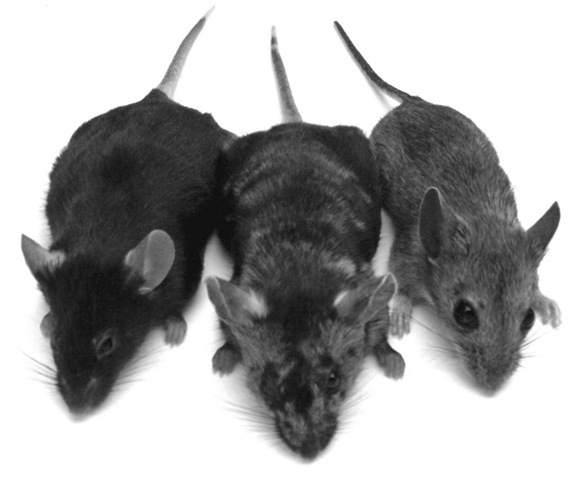
From left: Mus musculus (house mouse); chimera, a genetic fusion of a house and wood mouse; and Apodemus sylvaticus (wood mouse). Both small and large animals are used for testing new regenerative medicine therapeutics.
On a final note, recent advances suggest that patient-derived inducible pluripotent stem (iPS) cells may use as different strategies of avoiding this problem in the near future. The major advantage of using tissue-specific stem cells and iPS cells is that the patient’s own cells can be expanded in culture and then re-introduced into the patient without immune rejection.