Knowing your blood lipid (fat) levels—the various forms of cholesterol and triglycerides—is important. But what these numbers mean can be confusing, and how the different types of cholesterol—not to mention other blood fats—relate to coronary artery (heart and blood vessel) disease also can be a puzzle.
Coronary artery disease is the number one killer of Americans. Studies point to certain abnormalities in cholesterol and triglyceride levels as a major contributor to this problem. There is plenty of good news to suggest that public awareness of heart disease and its risk factors is making a difference. Deaths from cardiovascular disease continue to decrease. Much credit for this encouraging trend goes to improved treatments and modification of the risk factors for heart disease, including lowering cholesterol levels. Despite these substantial improvements, the American Heart Association reports that cardiovascular disease still kills almost 1 million Americans each year. This is more than all cancer deaths combined. More than 6 million Americans experience symptoms due to coronary artery disease. As many as 1.5 million Americans will have a heart attack every year, and about half a million of them will die.
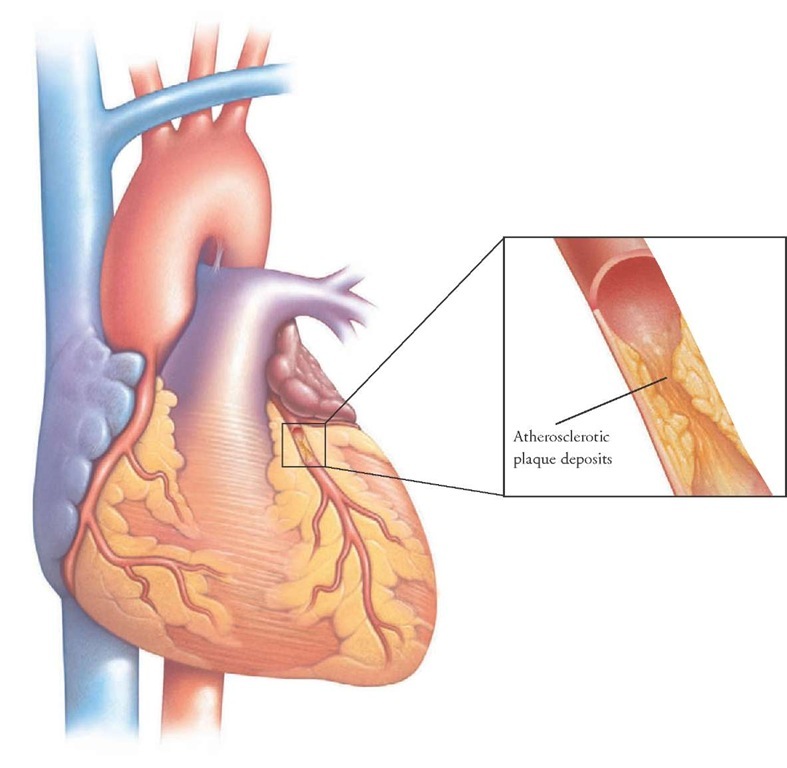
Blockage of the coronary arteries supplying the heart muscle (which can lead to heart attack) causes more deaths, disability, and economic loss than any other type of heart disease.
Atherosclerosis
The coronary arteries are the heart’s own circulatory system. They supply the heart with blood, oxygen, and nutrients. The heart uses this blood supply for energy to perform its continuous task of pumping. Coronary artery disease can take many different forms, but each has essentially the same effect: the heart muscle does not get enough blood and oxygen through the coronary arteries. Consequently, its own demands for oxygen and nutrients are not met. This condition can be either temporary or permanent.
Most coronary artery disease is caused by atherosclerosis (also known as "hardening of the arteries"). The term "atherosclerosis" comes from the Greek ather (meaning "porridge") and sklerosis (meaning "hardening"). Healthy arteries are flexible, strong, and elastic. The inner layer of arteries is smooth, enabling blood to flow freely.
Atherosclerosis can be a silent, painless process in which cholesterol-containing fatty deposits accumulate in the walls of the arteries. These accumulations occur as lumps called plaques. As plaque deposits enlarge, the interior of the artery narrows, and the flow of blood is then reduced (see the illustration below). If reduced flow occurs in the coronary (heart) arteries, it can lead to a type of chest pain called angina pectoris.
As a plaque enlarges, the inner lining of the artery becomes rough. A tear or rupture in the plaque may cause a blood clot to form. Such a clot can block the flow of blood or break free and plug another artery. If the flow of blood to a part of the heart is stopped, a heart attack results. If the blood flow to a part of the brain stops, a stroke occurs.
A Closer Look at Blood Lipids
Many factors influence the clogging of arteries, but cholesterol is a primary one. Cholesterol is a waxy, fat-like substance (a lipid). Although it is often discussed in negative terms, it is an essential component of the body’s cell membranes. It also serves to insulate nerves and is a building block in the formation of certain hormones. The liver uses it to make bile acids, which help digest food.
Confusion about cholesterol is due in great part to the all-purpose use of the term. Cholesterol has two sources: the foods we eat (about 20%) and the cholesterol that is made by the body (about 80%). Dietary cholesterol is found only in animal products, such as meat and dairy products, or foods made with animal products. Examples include all meats, fish, and poultry, eggs, and milk products. In addition, both the amount and the type of fat eaten influence the blood cholesterol level. Both saturated (primarily from animals) and trans-saturated (oils that have been processed to make them more solid) fats increase the amount of cholesterol made by the liver.
In atherosclerosis, plaque deposits gradually accumulate in the lining of the arteries. As the deposits enlarge, blood circulation is impaired. This increases the risk for heart attack, stroke, and other vascular problems.
Mini-Glossary of Lipid-Related Terms
• Apolipoprotein—Proteins that combine with lipids to make them dissolve in the blood.
• Cholesterol—A soft, waxy substance in the blood and in all your body’s cells. It is used to form cell membranes, some hormones, and other needed tissues. Dietary cholesterol is found only in food derived from animal sources.
• HDL cholesterol—About 20 to 30 percent of blood cholesterol is carried by high-density lipoproteins (HDL). HDL carries cholesterol away from the arteries and back to the liver, where it is removed from the body. HDL seems to protect against heart attack. This is why HDL cholesterol is referred to as the "good" cholesterol.
• LDL cholesterol—Low-density lipoprotein (LDL) cholesterol is the main cholesterol carrier in the blood.
When there is too much LDL cholesterol circulating in the blood, it can slowly build up in the walls of the arteries that feed the heart and brain. This is why LDL cholesterol is often called the "bad" cholesterol.
• Lipoproteins—Lipids combined with apoproteins.
• Triglycerides—Triglycerides are derived from fats eaten in foods or made in the body from other sources such as carbohydrates. Calories ingested in a meal and not needed immediately by tissues are converted to triglycerides and transported to fat cells to be stored. Hormones regulate the release of triglycerides from fat tissue to meet the daily need for energy between meals.
• VLDL cholesterol—In the fasting state, very low-density lipoproteins (VLDL) contain 15 to 20 percent of the total blood cholesterol, along with most of the triglycerides.
Unique Roles: LDL and HDL Cholesterol and Triglycerides
Cholesterol and triglycerides are fats and are insoluble in the blood. However, when they combine with protein they become lipoproteins and are able to dissolve in and be carried by blood throughout the body. (See sidebar: Mini-Glossary of Lipid-Related Terms, above.)
Low-density lipoprotein (LDL) cholesterol is the main cholesterol carrier in the blood. There is a direct relationship between the level of LDL cholesterol (or total cholesterol) and the rate of coronary artery disease. When there is too much LDL cholesterol circulating in the blood, it can slowly build up in the walls of the arteries that feed the heart and brain. For this reason, LDL is often referred to as the "bad" cholesterol.
If there are too many LDL particles in the blood, or the liver (the normal site of metabolism) does not remove LDL quickly enough from the blood, it builds, particularly in blood vessels. It is the role of high-density lipoprotein (HDL) to counteract this effect.
About a third to a fourth of blood cholesterol is carried by HDL. HDL carries cholesterol away from the arteries and back to the liver, where it is removed from the blood. It is therefore often referred to as the "good" cholesterol. A high level of HDL seems to protect against atherosclerosis and heart attack. The opposite is also true: a low HDL level indicates an increased risk of atherosclerosis. Thus, the goal is to have a high HDL cholesterol level and a low LDL cholesterol level.
Triglycerides in the blood are derived from fats eaten in foods or produced when the body converts excess calories, alcohol, or sugar into fat. Most triglycerides are transported through the bloodstream as very low-density lipoprotein (VLDL). Some cholesterol is also present in VLDL.
A certain amount of triglycerides in the blood is normal. Hormones regulate the release of triglycerides from fat tissue to meet the body’s needs for energy between meals. However, at high levels, triglycerides may contribute to the development of atherosclerosis. Increased triglyceride levels also may be a consequence of other diseases, such as untreated diabetes mellitus.
Calories ingested at a meal and not used immediately by tissues are converted to triglycerides and transported to fat cells to be stored.
Blood Testing
The only way to determine whether cholesterol and other blood lipids are in a desirable range is to have them measured by a blood test. The National Cholesterol Education Program guidelines recommend that total cholesterol, HDL cholesterol, and triglycerides be measured at least once every 5 years in all adults age 20 or older. However, your physician also may recommend that the screening include LDL cholesterol and triglycerides.
Triglycerides must be measured after an overnight fast because eating can have a marked effect on blood triglyc-eride levels. Therefore, fast for at least 12 hours before blood is drawn. Do not drink alcohol for 24 hours before the test. If you have a risk factor(s) for heart disease, consult your physician regarding the optimal frequency of testing. (See sidebar: Risk Factors for Coronary Artery Disease Other Than LDL Cholesterol, below.)
In a sense, it is incorrect to think of a cholesterol (or triglyceride) level as being strictly abnormal or normal. Although ranges of cholesterol levels have been identified which are considered "too high," there is no "magic number" that separates risky levels from safe levels. Actually, the ranges for adults are based on a consensus of experts. They have identified lipid levels in the blood above which the risk for development of coronary complications is high enough to warrant medications or lifestyle changes.
People with cholesterol or triglyceride levels in the higher-risk zones are said to be hypercholesterolemic or hypertriglyceridemic (hyper means "high," and emic means "in the blood"). But, as with all risk factors, being in the "high" range does not guarantee that coronary artery disease will develop, nor does being in the "low" range guarantee avoiding it.
Blood test numbers are only guidelines. If the numbers stray from the desirable range, a physician can provide advice on what to do. Remember that each number takes on greater meaning in light of the other lipid results and in the presence of other cardiovascular disease risk factors (see sidebar: Your Blood Lipid Test Results—What Do Those Numbers Mean? page 65).
Risk Factors for Coronary Artery Disease Other Than LDL Cholesterol
• Age: males 45 years or older and females age 55 years or older, or females who have had premature menopause without estrogen replacement
• Family history of early coronary artery disease
• Current cigarette smoking
• High blood pressure
• Low HDL cholesterol (less than 40 mg/dL)
• Diabetes mellitus
The Reasons for High Blood Lipid Levels
Why do some people have high cholesterol and triglycerides? High levels may result from genetic makeup or lifestyle choices or both. Heredity may endow people with cells that do not remove LDL or VLDL cholesterol from the blood efficiently, or with a liver that produces too much cholesterol as VLDL particles or too few HDL particles. Lifestyle factors such as a high-fat diet, obesity, smoking, and physical inactivity also can cause or contribute to high cholesterol levels, increasing an individual’s risk for atherosclerosis.
For a more complete picture of cardiovascular health, other risk factors—beyond cholesterol and triglycerides— must be considered. The more risk factors an individual has in combination with undesirable lipid levels, the greater the chances for development of cardiovascular disease.
The risk factors for cardiovascular disease are divided into those that can be changed and those that cannot.
Risk Factors That Can Be Changed or Treated
Smoking cigarettes damages the walls of the blood vessels, making them more receptive to the accumulation of fatty deposits. Smoking also may lower the HDL by as much as 15 percent. Quitting smoking may return the HDL to a higher level.
High blood pressure damages the walls of the arteries, thus accelerating the development of atherosclerosis. Some medications for high blood pressure increase LDL and triglyceride levels and decrease HDL levels. Others do not. Blood pressure that is properly managed decreases the progression and risk for cardiovascular disease.
Sedentary lifestyle is associated with a decrease in HDL. Aerobic exercise is one way to increase HDL. Aerobic activity is any exercise that requires continuous movement of the arms and legs and increases the rate of breathing. Even 30 to 45 minutes of brisk walking every other day helps protect the cardiovascular system.
Obesity is a risk to cardiovascular health. Excess body fat increases total cholesterol, LDL cholesterol, and triglyc-eride levels. It also lowers the HDL cholesterol level. Obesity increases blood pressure and the risk for diabetes, which can increase the chances of heart disease developing. Losing just 10 percent of excess body weight can improve triglyceride and cholesterol levels.
Diabetes can increase the triglyceride level and decrease the HDL cholesterol level. Good control of blood sugar helps reduce increased triglyceride levels.
Your Blood Lipid Test Results—What Do Those Numbers Mean?
Use this table as a general guide. The importance of each number varies according to your sex, health status, and family history. For example, if you already have heart disease, you will want to lower your LDL cholesterol level to less than 100 mg/dL. Your health care provider can help clarify your specific risk.
|
|
|
Level (in mg/dL) |
|
|
Test |
Optimal |
Borderline |
Undesirable |
|
Total cholesterol |
Less than 200 |
200-240 |
More than 240 |
|
HDL cholesterol Considered "good"—the higher, the better |
60 or more |
- |
Less than 40 |
|
LDL cholesterol* Considered "bad"—the lower, the better |
Less than 100 |
130-160 |
More than 160 |
|
Cholesterol/HDL ratio |
Less than 4.5 |
4.5-5.5 |
More than 5.5 |
|
LDL/HDL ratio |
Less than 3 |
3-5 |
More than 5 |
|
Triglycerides |
Less than 150 |
150-200 |
More than 200 |
LDL may be measured directly or may be estimated from the other numbers if your triglyceride level is lower than 400 mg/dL. You can estimate LDL yourself by using this equation: LDL = Total Cholesterol – HDL + triglyceride level divided by 5.
Estrogen deficiency and menopause increase the risk of heart disease. Conversely, estrogen replacement lowers the risk in certain groups of estrogen-deficient women.
Risk Factors That Cannot Be Changed
Aging—Aging usually increases the level of LDL cholesterol, although the reasons are not understood. It could be the aging process itself that causes this, or an increase in body fat with advancing age.
Sex—Cardiovascular disease is not only a man’s disease, as once thought. It is the number one killer of women, claiming the lives of 500,000 women every year. Cardiovascular disease occurs in women almost as often as it does in men. It just happens later in life. Before menopause, a woman’s risk of coronary artery disease is lower than that of a man. Menopause results in an increase in LDL cholesterol and a decrease in the protective HDL cholesterol. After menopause, a woman’s risk of heart disease is the same as that of a man. Treatment with estrogen helps to return the risk to premenopausal levels.
Family history—A family history of abnormal lipid levels or early heart disease increases the risk of heart attack and stroke.
Lifestyle Changes to Reduce Risk
There is significant opportunity to reduce the risk of getting cardiovascular disease. Changes in nutrition along with increased physical activity and learning to decrease stress can improve blood cholesterol and triglyceride levels. Making dietary changes to improve blood cholesterol and triglyceride levels involves these steps:
Maintain a desirable weight—A diet that is high in fat also can be unnecessarily high in calories and contribute to an unhealthy weight. Decrease the total amount of fat eaten. Limit fat—saturated, polyunsaturated, and monoun-saturated—to less than 30 percent of your total daily calories.Some individuals may need to restrict fats even more. Because all foods with fats contain a combination of these fats, it is important to reduce total fat.
Reduce saturated fat—The major dietary culprit in an increased blood cholesterol level and increased risk for coronary artery disease, saturated fat is typically solid or waxy at room temperature. Minimize your intake of saturated fat. Foods high in saturated fat include red meats and dairy products as well as coconut, palm, and other tropical oils (check the ingredient portion of the food label).
Replace saturated fat with unsaturated fat— Polyunsaturated and monounsaturated fats should make up the remaining fat allowance. In the recommended amounts, polyunsaturated fats reduce LDL cholesterol, but at the expense of the protective HDL cholesterol, whose levels also may decrease. Polyunsaturated fats are usually liquid at room temperature and in the refrigerator. Vegetable oils such as safflower, corn, sunflower, soy, and cottonseed oil are high in polyunsaturated fat. Monounsaturated fats tend to have the same effects on LDL cholesterol without lowering HDL cholesterol. Monounsaturated fats are liquid at room temperature but may start to solidify in the refrigerator. Olive, canola, and nut oils are sources of monounsaturated fats.
Limit trans fat—This fat is also called partially hydrogenated vegetable oil. This type of fat may be as harmful to your health as saturated fat because it increases blood cholesterol levels, among other effects. Major sources are hardened vegetable fat, such as margarine or shortening, and products made from these fats, such as cereals, cookies, and crackers.
Cholesterol-Lowering Margarine?
Who would have thought a person could consume margarine and possibly lower cholesterol? This functional food was approved for use in the United States and was introduced to the grocery shelves in 1999. Two types are available: Benecol and Take Control. Benecol is made with a refined form of plant sterol called stanol ester, which is derived from wood pulp. Take Control contains sterol esters, which are made from vegetable oils, soybean, and corn. These new margarines may help lower LDL cholesterol when used as directed by a physician. The margarines may lower LDL cholesterol 7 to 10 percent. Therefore, it is important that they be used in conjunction with a healthful diet full of whole grains, fruits, and vegetables and one that is low in total fat, saturated fat, and cholesterol.
Reduce dietary cholesterol—The daily limit for dietary cholesterol is 300 milligrams. Dietary cholesterol is found only in foods made from or containing animal products. A good way to lower dietary cholesterol is to limit the amount of meat and dairy products. Organ meats and egg yolks are also high in cholesterol.
Eat a plant-based diet—A diet that has generous amounts of grains, vegetables, and fruits is naturally lower in fat and has good sources of soluble fiber and antioxidants, which may protect blood vessels from damage and plaque buildup.
Fruits and vegetables and whole-grain products are also natural sources for folate—a B vitamin that controls the amount of homocysteine in the blood. Homocysteine is an amino acid (a building block of protein) normally found in your body. Your body needs homocysteine to manufacture protein to build and maintain tissue.
Problems arise when there is too much homocysteine, which can cause the tissues lining the arteries to thicken and scar. Cholesterol builds up in the scarred arteries, leading to clogged vessels and blood clots. Adequate intake of this vitamin can help normalize homocysteine levels and may reduce the risk for cardiovascular disease (see sidebar: Folate and Heart Disease, page 67). There is also accumulating evidence that vitamin E may reduce the risk of heart attack.
Cardiovascular Disease and Physical Activity
Unfortunately, most of the population of the United States is sedentary. Sedentary people have nearly twice the risk of having a fatal heart attack as active people of the same age when other factors—such as smoking and high cholesterol—are equal. Consult a physician before embarking on an exercise program. Then, follow these tips for maximal results:
• Choose an aerobic activity. It can be something like
walking, jogging, bicycling, or swimming.
• Gradually increase the time and frequency of the exercise.
Work up to exercising for 30 minutes daily.
When Are Medications Necessary?
If changes in lifestyle have not brought lipid values into the goal range, medication may be necessary. Before recommending a medication, your physician will use careful judgment and weigh many variables—sex, age, current health, family history of early heart disease or abnormal lipids, and the side effects of medication.
Folate and Heart Disease
Homocysteine is an amino acid that is made from dietary protein. Too much homocysteine can damage arterial walls, allowing fatty plaque deposits to clog arteries and promote blood clotting.
|
Food |
Serving |
Folate Amount |
% Daily Value |
|
|
|
Size |
(micrograms) |
(based on 400 |
|
|
|
(cup) |
|
micrograms) |
|
|
Breakfast cereals |
1/2 to 1 |
100-400* |
25-100 |
Folate can decrease homocysteine |
|
|
|
(check label) |
|
levels. About 400 micrograms a |
|
Lentils (cooked) |
1/2 |
180 |
45 |
day is enough to lower your blood |
|
Chickpeas |
1/2 |
140 |
35 |
concentration of homocysteine. To |
|
Asparagus |
1/2 |
130 |
33 |
get more folate, eat plenty of beans, |
|
Spinach |
1/2 |
130 |
33 |
fruits, and vegetables—preferably |
|
Black beans |
1/2 |
130 |
33 |
raw or lightly cooked. Half the folate |
|
Kidney beans |
1/2 |
115 |
29 |
in foods can be lost in cooking. |
*Manufacturers of grain-based foods now fortify their products with folic acid—a synthetic form of the vitamin.