Biomedical Engineering Reference
In-Depth Information
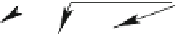
shear
ATn2
PoG
I
RTK
GPCR
NOx
Ca
EC
Rho
PI3K
Cam
PKC
ERK
stretch
NO
Csk
Cam/CamK
ET
Cam/PP2B
NFAT
stretch
TNF
α
TGF β
ATn2
PDGF
I
GCase
RTK
GPCR
NOx
SMC
DAG
Ca
IP3
PI3K
Rho
MMP
PKC
(VD)
(VC)
Ca
Csk
MAPK
Csk
PKB
growth
Fig. 9.12
Artery wall adaptation to hemodynamic stresses. The artery bore is locally controlled
by mechanotransduction experienced by both endothelial and smooth muscle cells as well as
hormones and growth factors. Angiotensin-2 acts on endothelial cells via NO to cause vasodilation
that reduces vasoconstriction generated by direct angiotensin-2 effect on smooth myocytes. In
other words, angiotensin-2 receptors have opposite effects according to cell type. Their number on
endothelial cells is smaller than that on smooth myocytes (I: integrin; PoG: proteoglycan; NOx:
reduced form of nicotine adenine dinucleotide phosphate (NAD(P)H) oxidase; NFAT: nuclear
factor of activated T cells).
A fundamental couple at the microscopic scale is composed of an endothelial
and a smooth muscle cell (Fig.
9.13
). At the nanoscopic scale, numerous agents
contribute to the local control of the vasomotor tone (Table
9.34
). Yet, let us
consider a fundamental couple at the nanoscopic scale: nitric oxide and endothelin
that cause vasodilation and -constriction, respectively. The major regulators of the
vasomotor tone are thus assumed to carry out the entire chemical control. Even
using this assumption, reality remains complex. Endothelin-1 indeed targets 2 types
of cognate receptors — ET
A
and ET
B
— that have opposite effects (Table
9.35
).
The simplified model of mechanotransduction takes into account these 2 types of
endothelin receptors to be representative enough (Fig.
9.14
).












































































Search WWH ::

Custom Search