Environmental Engineering Reference
In-Depth Information
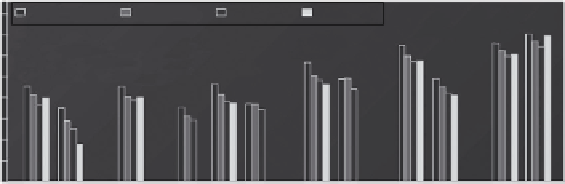
S
ã
o Paulo
100,000,000
Mexico City
Santiago
New York
Restricted
activities
Acute
morbidity
10,000,000
1,000,000
100,000
10,000
1,000
100
10
1
Other
medical visits
Hospital
admissions
Chronic
morbidity
Mortality
FIGURE 13.5
Estimated potential human health beneits from reductions in air pollution associated with
implementing GHG mitigation measures in four cities (2001-2020). (From Cifuentes, L. et al.,
Science
,
293(5533), 1257, 2001b.)
assessments of GHG mitigation policies on public health have been produced for Canada (Last et al.,
1988) and selected energy sectors in China (Wang and Smith, 1999; Cao et al., 2008), under dif-
fering baseline assumptions. A synthesis of research on co-beneits and climate change policies in
China concluded that China's Clean Development Mechanism potentially could save 3,000-40,000
lives annually through co-beneits of improved air pollution (Vennemo et al., 2006). Several studies
investigated the links between regional air pollution and climate policy in Europe (Working Group
on Public Health and Fossil Fuel Combustion, 1997; Alcamo, 2002; van Harmelen et al., 2002).
13.5.3 M
onetary
v
aluations
oF
M
itigation
c
o
-b
eneFits
To help decision makers assess policies with a wide array of health consequences, outcomes are often
converted into comparable formats. One approach is to convert health outcomes into economic terms
to allow direct comparison of costs and beneits. There are several common approaches for eco-
nomic valuation of averted health consequences (step 3 of Figure 13.4): cost of illness (COI); human
capital; willingness to pay (WTP) methods; and quality-adjusted life year (QALY) approaches. The
COI method totals medical and other out-of-pocket expenditures and has been used for acute and
chronic health endpoints. For instance, separate models of cancer progression and respiratory disease
were used to estimate medical costs from these diseases over one's lifetime (Hartunian et al., 1981).
However, early attempts to value mortality risk reductions applied the human capital approach, which
estimates the “value of life” as lost productivity. This method is generally recognized as problematic
and not based on modern welfare economics, where preferences for reducing death risks are not cap-
tured. Another limitation is incorporation of racial- or gender-based discrimination in wages. This
method assigns value based solely on income, without regard to social value, so unpaid positions such
as homemaker and lower-paid positions such as social worker receive lower values. Because data are
often available for superior alternatives, this approach is rarely used in health beneit studies. WTP
generates estimates of preferences for improved health that meet the theoretical requirements of neo-
classical welfare economics, by aiming to measure the monetary amount persons would willingly
sacriice to avoid negative health outcomes. Complications arise in analysis and interpretation because
changes in environmental quality or health often will themselves change the real income (utility)
distribution of society. A valuation procedure that sums individual WTP does not capture individual
preferences about changes in income distribution. Another complication is that the value of avoided
health risk may differ by type of health event and age. The QALY approach attempts to account for the
quality of life lost by adjusting for time “lost” from disease or death, but these estimates may be very
insensitive to different severities and types of acute morbidity (Miller, 2006).
Search WWH ::

Custom Search