Biomedical Engineering Reference
In-Depth Information
Ca
++
Cryoprecipitate:
fibrinogen
factor XIII
fibronectin
aprotonin
Prothrombin
Thrombin
Factor XIII
Fibrinogen
Fibrin gel
Ca
++
Thrombin
Ca
++
Aprotinin
Factor XIIIa
Plasmin
Cross-linked fibrin clot
Aprotinin
Fibronectin
Cross-linked fibronectin
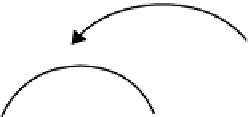
FIGURE 20.2
Schematic illustration of fi brin glue delivery and the chemical reactions that result in the
production of cross-linked fi brin.
(and calcium ions) also activates factor XIII to XIIIa (also termed transglutamidase), which cross-
links fi brin polymers solidifying the clot. The addition of aprotinin inhibits serine proteases, such
as plasmin, which breakdown the fi brin clot via the process of fi brinolysis. Fibronectin present in
the starting solution is also cross-linked by factor XIIIa. To prepare autologous fi brin, the patient
donates approximately 400 ml of blood 3 weeks prior to surgery. The whole blood is centrifuged to
separate the plasma, which is collected and stored at
40°C. The plasma is thawed at 4°C for 24 h,
and the freeze-thaw process is repeated twice. The plasma is then centrifuged, and the autologous
cryoprecipitate is collected, stored at
−
40°C, and thawed just prior to surgery [18]. The thawed
cryoprecipitate is drawn into a syringe and connected via a Y-connector to a second syringe con-
taining thrombin (1000 units/mL), calcium chloride, and aprotinin (Figure 20.2). Simultaneous
delivery of the cryoprecipitate and thrombin via the Y-connector into the fi stula tract creates the
fi brin glue [18,19]. As the fi brin clots, it seals the fi stula tract and thus provides a provisional matrix
for the infi ltration of fi broblasts and endothelial cells from the surrounding tissue, initiating tissue
healing. Plasmin released from the surrounding tissue eventually causes lysis of the fi brin glue after
7-14 days. The rapid degradation of fi brin after a relatively short period of time may occur before
complete tissue healing has taken place and possibly accounts for the disappointing published suc-
cess rates, ranging from 10% to 85%, for fi brin glue injection of perianal fi stulas [20]. Because of
this low success rate a number of alternative materials that do not possess these inherent problems
are being developed for use as fi ller materials that are likely to achieve higher success rates com-
pared with the materials currently available. These alternative materials include collagen-based
materials, such as Permacol (Tissue Science Laboratories Plc., Aldershot, Hampshire, U.K.) [21],
and microspheres consisting of alginate/bioactive glass composites [22].
For any biomaterial developed for fi stula repair, particular consideration should be given to
countering bacterial infections, a problem frequently associated with medical implants that can
require removal of the implant. This may be of particular signifi cance in perianal fi stulas since,
unless thoroughly cleansed, the tracks that communicate with the gastrointestinal tract are likely to
be colonized by gut bacteria [15].
−
20.4 BULKING BIOMATERIALS
20.4.1 F
ECAL
I
NCONTINENCE
Fecal incontinence affects about 2% of the population and may be caused by defects or weakness
of the internal anal sphincter [23]. Current treatment options include antidiarrheal drugs or sacral
nerve stimulation, but these strategies are limited by expense and their short-term effi cacy. Surgical
reconstruction of the internal anal sphincter is usually unsuccessful in the majority of patients.