Biomedical Engineering Reference
In-Depth Information
vaporization. It has been suggested that this is related to the
high tensile strength of collagen fi bers. A large induced pres-
sure is necessary to disrupt the tissue (92). The Er laser vapor-
izes tissue more explosively than with CO
2
LSR, so that at
fl uences of only 5-10 J/cm
2
, there is violent ablation, and par-
ticles are ejected at supersonic velocities. There is recoil at the
tissue surface—the skin actually appears to be “pushed down”
in real time. Momentum transfer produces stress waves, which
combined with the small level of RTD may contribute to the
tendency for bleeding after Er:YAG LSR. In general, in any
laser resurfacing procedure, by confi ning energy both spatially
and temporally, more effi cient vaporization occurs with less
thermal decomposition of proteins and less chance of char-
ring. Nonablative skin remodeling has also been used with
water as a chromophore (1320, 1450, and 1540 nm) and is
intended to heat a subsurface “slab” of tissue (without epider-
mal damage). Both wrinkles and scars have improved with
these approaches, but results are normally modest compared
with properly applied ablative approaches. PDLs and other
VIS light modalities have proved effective in scars (67,93-96).
Although there is an indirect effect of VIS light technologies
on wrinkles in some cases, no VIS light modality has achieved
the same improvement in fi ne wrinkling as ablative modalities
with traditional fl uences. Fractional lasers have expanded
greatly since the last edition of this topic. Both ablative and
nonablative approaches have played an ever-increasing role in
wrinkle reduction (97-99).
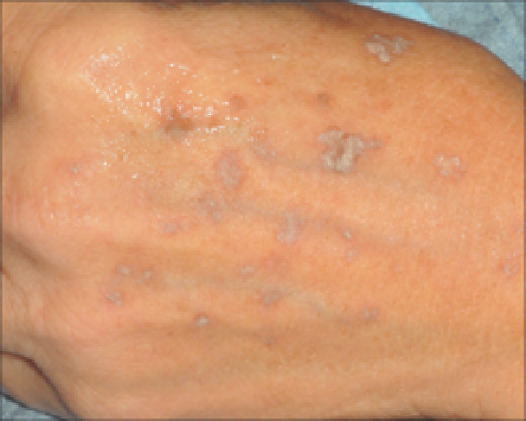
Figure 1.30
Note whitening response of lentigo on hand after Q-switched
alexandrite laser.
treat. In most cases, the most complete removal (with only one
treatment session) is achieved via Q-switched technologies.
On the other hand, the least invasive and gentlest removal is via
long pulse (milliseconds) technologies in the VIS light spec-
trum, such as IPL devices as well as KTP lasers. Long-pulse
alexandrite lasers have also been employed as well as long-
pulsed diode lasers to gently heat epidermal static pigmented
lesions. “Dermal” static pigmented lesions such as nevus of
Ota respond best to Q-switched lasers (103). This is consistent
with the theory of SPT. With longer pulses (millisecond-
domain), the dermal melanocytes, which are of relatively low
concentration (compared with melanocytic nests in com-
pound nevi or highly pigmented basal cell layers in lentigos),
simply do not become hot enough to achieve pigment reduc-
tion (8). For light lentigos, the contrast between the skin's
background color and the lesions may become too small for
effective reduction by long-pulsed GY sources. In these cases,
the shorter pulses of Q-switched lasers are required for selec-
tive heating of pigmented lesions. Melasma is a challenging
condition to treat via lasers, most likely due to its dynamic and
infl ammatory nature (compared with the static nature of len-
tigos) (104). Ablative lasers can sometimes result in improve-
ment; however, the ablation normally has to be carried out
deeply, or postinfl ammatory hyperpigmentation may out-
weigh any achievement gains. Q-switched lasers typically result
in only temporary improvement (followed by PIPA that wors-
ens the appearance!) (104). On the other hand, longer pulsed
VIS light laser technologies can sometimes achieve gradual
improvement in melasma so long as the settings are not too
high (105,106).
Acne
There are many EMR-based approaches to acne treatment,
which are limited only by our understanding of the patho-
physiology of acne. Mechanisms for improving acne include
suppression of
P. acnes
(PDT with endogenous and exogenous
PS), normalization of the keratinization process through
infundibular heating (some MIR lasers), and possible seba-
ceous gland damage through deep heating with IR lamp, deep
MIR, and RF technologies (100). Of all the techniques, the
only one that shows long-term acne reduction with
micro-
scopic
evidence of marked sebaceous gland damage is
red light
ALA-PDT
. This histologic picture has only been observed with
long ALA incubation times (>4 hours) coupled with low
power density light sources (101). A new system undergoing
studies uses gold nanoshells that are targeted by 755- and
810-nm lasers to disrupt and damage the infundibulum and
sebaceous glands. Delivery of the shells to the target relies on
a transfolllicular route (102).
Pigmented Lesions
Melanosome heating conforms well with the basic theory of
SPT (19). With very short pulses (nanoseconds), one observes
immediate frost whitening at the surface (Fig. 1.30) added.
Although the exact cause is unknown, it is most certainly
related to the formation of gas bubbles that intensely scatter
light (19). Over several minutes, these bubbles dissolve, caus-
ing the skin color to return to nearly normal. As the pulse
duration increases, melanosome heating becomes more gentle,
and there tends to be focal DE junction heating but with con-
siderable diffusion outside the melanosome. Pigmented lesions
can be divided into superfi cial and deep. Static epidermal pig-
mented lesions such as lentigos tend to be straightforward to
Vascular Lesions
Selective microvascular injury can be achieved well into the
penetrating red visible wavelengths. The absorption coeffi cient
of bloodless dermis is only 0.1-0.3 cm
−1
throughout the red
wavelength region, and Hb absorption exceeds bloodless der-
mis throughout the red and NIR spectrum. It follows that even
lasers with relatively poor Hb absorption, such as the ruby
laser, have been used for PWS treatment. Despite competition