Biomedical Engineering Reference
In-Depth Information
when enamel proteins are used, large amounts
of cementum are formed, and it seems logical
to conclude that this is needed, since the peri-
odontal ligament fi bers attach to both cemen-
tum and bone.
Bone graft materials have been used to fi ll
the void in the bone around the tooth created
by periodontal disease. Many different types
of materials have been employed, but demin-
eralized freeze-dried bone allograft (DFDBA)
is the best documented for stimulating
periodontal regeneration [
better than some other commercially available
graft materials [
].
Many materials have been combined to
stimulate periodontal regeneration. In larger
periodontal defects, some type of bone graft
material is required to prevent the gingiva from
collapsing into the bone defect, an event that
severely limits periodontal regeneration. It is
generally thought that a combination of mate-
rials will be synergistic and facilitate regenera-
tion. An osteoconductive scaffold combined
with factors that stimulate cellular activity is
likely to bring about more effective periodontal
regeneration [
38
]. This material
(considered by many to be osteoconductive)
contains bone morphogenetic and other pro-
teins, but their specifi c role in stimulating
bone formation is not known. For many
years it was assumed that all components of
DFDBA had an equal role in stimulating
periodontal tissue formation. However, we
were able to show that commercial DFDBA
varies in its osteoinductive activity, whether
derived from the same or from different tissue
banks [
42
]. Commercially available
enamel matrix proteins have therefore been
combined with bone graft material [
57
]. In one
such study with baboons, periodontal defects
treated with autogenous bone grafts combined
with enamel proteins were compared with
untreated periodontal defects [
5
]. Signifi cant
new amounts of cementum and bone were
formed, particularly in the narrower lesions
(Fig.
22
]. Osteoinductive activity was also
greater when the tissue came from younger
donors, with gender making no difference [
58
). Regeneration occurred by formation
of new cementum, periodontal ligament, and of
bone that took place beyond a mark that had
been placed at the apical (lower) aspect of the
original periodontal defect.
The above discussion makes it evident that
current therapeutic efforts to treat periodontal
disease are aimed at regenerating the lost peri-
odontal tissues, including bone, the periodon-
tal ligament, and cementum.
9
.
3
].
Furthermore, the addition of exogenous bone
morphogenetic protein (BMP) enhanced the
osteoinductive activity of the DFDBA prepara-
tions. Whether or not variance in osteoinduc-
tive activity is of clinical signifi cance, the
principal value of this material is to stimulate
periodontal regeneration, which it does far
59
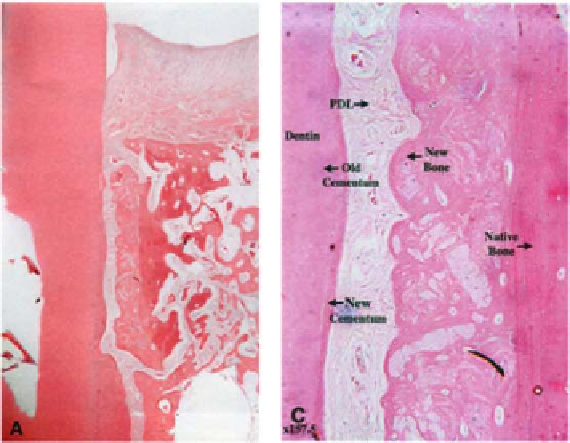
Figure 9.3.
Histologic view of peri-
odontal regeneration in response to
enamel matrix proteins. These slides
demonstrate the reformation of sup-
porting bone, periodontal ligament
(PDL), and new cementum along the
root surface representative of periodon-
tal regeneration in a narrow bony
defect.