Biomedical Engineering Reference
In-Depth Information
healing, the tooth and surrounding tissue were
removed by block section and examined histo-
logically. The results of this multicenter clini-
cal trial (unpublished) showed that the rhBMP-
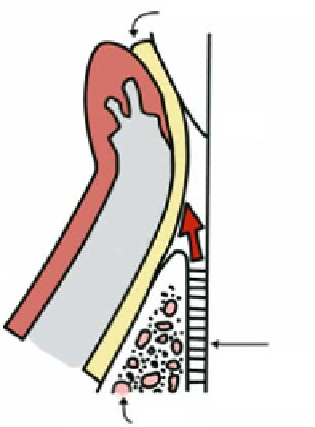
Barrier Membrane
2
and collagen sponge did not stimulate peri-
odontal regeneration, even though studies in
dogs had demonstrated a partial effect on bone
growth [
Tooth
]. In the dog study, however, areas of
ankylosis and root resorption had been
observed; this was not the case when the PDGF/
IGF combination was used.
The newest approved protein stimulant of
periodontal regeneration is a heterogeneous
mixture of proteins extracted from enamel
harvested from developing tooth buds in
pigs [
71
Gingiva
]. The predominant component in
this mixture is amelogenin; however, other
proteins in this mixture have also been shown
to contribute stimulating activities. Extracel-
lular matrix (ECM) proteins stimulate peri-
odontal regeneration to the same extent as
GTR procedures that utilize membrane barri-
ers [
18
Periodontal
Ligament
Bone
Figure 9.2.
Schematic cross-sectional representation of the
placement of a barrier membrane subgingivally as done for
guided tissue regeneration (GTR). This is thought to allow for
repopulation of the wound space with cells derived from the
bone, periodontal ligament, and cementum.
]. The advantage of the enamel proteins
is that they are less technique-sensitive and
affect proliferation and differentiation in
epithelium, periodontal ligament cells, and
bone cells [
62
, on the other hand,
acts only as a differentiation agent for bone
cells. The enamel proteins stimulate prolifera-
tion of less differentiated bone cells and
differentiation of mature bone cells. These
proteins also inhibit the growth of epithelial
cells and stimulate periodontal ligament fi bro-
blasts. Also of signifi cance is the fact that the
enamel proteins enhance the attachment and
growth of bone cells and periodontal ligament
cells [
60
]. rhBMP-
2
was needed to remove the membrane, led to the
development of several types of resorbable
membranes that exclude the gingiva and epi-
thelium. Most of these are made from polylac-
tic and/or polyglycolic acids or collagen.
Collagen membranes favor tissue ingrowth and
become exposed. However, all membrane bar-
riers are technique-sensitive and require time
to shape and place.
In more recent efforts to stimulate GTR,
various proteins were added to stimulate
growth of the periodontal structures. Early
efforts focused on factors that enhance cellular
competence and progression through the cell
cycle. Because a combination of platelet-derived
growth factor (PDGF) and insulin-like growth
factor (IGF) stimulated skin wound healing in
animals, this combination was used to success-
fully stimulate periodontal regeneration in
dogs and monkeys [
]. The mechanism for attachment
does not appear to involve integrin binding
(RGD) sequences, but it does require divalent
cations. Other studies have demonstrated that
the enamel proteins can inhibit anaerobic but
not gram-positive growth [
31
]. Although all
factors stimulate periodontal regeneration, the
importance of each individual attribute is not
presently known.
For many years, clinicians have fi lled the
osseous defects around teeth with some type of
bone-replacement graft material in the hope of
causing bone tissue to form around the tooth.
Even though bone typically is the largest com-
ponent of the missing periodontal structure, it
is not known whether stimulation of cementum
or the periodontal ligament is also required to
achieve optimal regeneration. For example,
66
]. However, this combi-
nation has not yet been commercially devel-
oped. Another approach has used recombinant
human bone morphogenetic protein
29
2
(rhBMP-
2
) to stimulate periodontal regeneration in
humans. In a pilot trial, rhBMP-
was placed in
a collagen sponge around teeth with periodon-
tal disease that were to be extracted. After
2