Fibromyalgia is a commonly encountered disorder characterized by chronic widespread musculoskeletal pain, stiffness, paresthesia, disturbed sleep, and easy fatigability along with multiple painful tender points, which are widely and symmetrically distributed. Fibromyalgia affects predominantly women in a ratio of 9:1 compared to men. This disorder is found in most countries, in most ethnic groups, and in all types of climates. The prevalence of fibromyalgia in the general population of a community in the United States using the 1990 American College of Rheumatology (ACR) classification criteria (see below) was reported to be 3.4% in women and 0.5% in men. Contrary to some previous reports, fibromyalgia was not found to be present mainly in young women but, rather, to be most prevalent in women >50 years. The prevalence increased with age, being 7.4% in women between the ages of 70 and 79. Although not common, fibromyalgia also occurs in children. The reported prevalence of fibromyalgia in some rheumatology clinics has been as high as 20%. Most patients present with fibromyalgia between the ages of 30-50 years.
Pathogenesis
Several causative mechanisms for fibromyalgia have been postulated to explain abnormal pain perception. Several abnormalities of the central nervous system have been suggested. Disturbed sleep has been implicated as a factor in the pathogenesis. Nonrestorative sleep or awakening unrefreshed has been observed in most patients with fibromyalgia. Sleep electroencephalographic studies in patients with fibromyalgia have shown disruption of normal stage 4 sleep [non-rapid eye movement (NREM) sleep] by many repeated α-wave intrusions. The idea that stage 4 sleep deprivation has a role in causing this disorder was supported by the observation that symptoms of fibromyalgia developed in normal subjects whose stage 4 sleep was disrupted artificially by induced α-wave intrusions. This sleep disturbance, however, has been demonstrated in healthy individuals; in emotionally distressed individuals; and in patients with sleep apnea, fever, osteoarthritis, or rheumatoid arthritis. Low levels of serotonin metabolites have been reported in the cerebrospinal fluid (CSF) of patients with fibromyalgia, suggesting that a deficiency of serotonin, a neurotransmitter that regulates pain and NREM sleep, might also be involved in the pathogenesis of fibromyalgia. Fibromyalgia patients as a group have been reported by some investigators to have reduced levels of growth hormone, which is important for muscle repair and strength. Growth hormone is secreted normally during stage 4 sleep, which is disturbed in patients with fibromyalgia. The reduction of growth hormone may explain the extended periods of muscle pain following exertion in these patients. The level of the neurotransmitter substance P has been reported to be increased in the CSF of fibromyalgia patients and may play a role in spreading muscle pain. Patients with fibromyalgia have a decreased cortisol response to stress. Low urinary free cortisol and a diminished cortisol response to corticotropin-releasing hormone suggest an abnormal hypothalamic-pituitary-adrenal axis. Autonomic dysfunction has also been suggested to play a role in the pathogenesis of fibromyalgia. Some patients experience orthostatic hypotension on tilt-table testing and may have increased resting supine heart rates. Disturbances of the autonomic and peripheral nervous system may also account for the dry eyes and mouth and the cold sensitivity and Raynaud’s-like symptoms seen in patients with fibromyalgia. Single photon emission computed tomography (SPECT) imaging has demonstrated reduced blood flow to the thalamus, caudate nucleus, and pontine tectum, which are areas in the brain involved in the signaling, integration, and modulation of pain. Patients with fibromyalgia have been shown to perceive stimuli such as heat or pressure as painful with less degree of stimulation than normal individuals. The actual threshold for detecting stimuli appears to be similar in both patients and normal subjects. Studies have also suggested that patients with fibromyalgia may have psychophysiologic abnormalities in their ability to inhibit irrelevant somatosensory stimulation.
Many patients with fibromyalgia have psychological abnormalities; there has been disagreement as to whether some of these abnormalities represent reactions to the chronic pain or whether the symptoms of fibromyalgia are a reflection of psychiatric disturbance. Approximately 30% of patients fit a psychiatric diagnosis, the most common being depression, anxiety, somatization, and hypochondriasis. Studies have also shown a high prevalence of sexual and physical abuse and eating disorders. However, fibromyalgia also occurs in patients without significant psychiatric problems.
Since patients experience pain from muscle and musculotendinous sites, many studies have been done to examine muscle, both structurally and physiologically. Inflammation or diagnostic muscle abnormalities have not been found. Evidence indicates deconditioning of muscles, and patients experience a greater degree of postexertional pain than do unaffected persons. A better understanding of fibromyalgia awaits further studies.
Clinical Manifestations
Symptoms are generalized musculoskeletal aching and stiffness and fatigue. Patients may complain of low back pain, which may radiate into the buttocks and legs. Others complain of pain and tightness in the neck and across the upper posterior shoulders. Patients complain of muscle pain after even mild exertion, and some degree of pain is always present. The pain has been described as a burning or gnawing pain or as soreness, stiffness, or aching. Pain may begin in one region, such as the shoulders, neck, or lower back (Chap. 22) before it eventually becomes widespread. Patients may complain of joint pain and perceive that their joints are swollen; however, joint examination yields normal findings. Stiffness is generally present on arising in the morning; usually it improves during the day, but in some patients it lasts all day. Patients may complain of numbness of their hands and feet. They may also feel colder overall than others in the home, and some may experience Raynaud’s-like phenomena or actual Raynaud’s phenomenon. Patients complain of feeling fatigued and exhausted and wake up tired. They also awaken frequently at night and have trouble falling back to sleep. Patients may experience cognitive impairment with difficulty thinking and loss of short-term memory. Headaches, including migraine type, are also common symptoms. Others experience episodes of light-headedness, dizziness, anxiety, or depression. Symptoms are made worse by stress or anxiety; cold, damp weather; and overexertion. Patients often feel better during warmer weather and vacations.
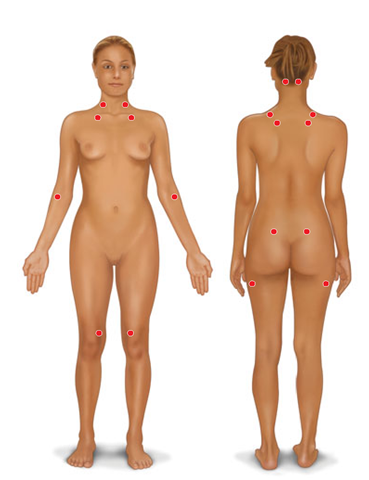
The characteristic feature on physical examination is the demonstration of specific sites or points, which are more tender or painful than the same sites in normal individuals. The ACR Criteria for Fibromyalgia defines 18 tender points (Fig. 21-1).These points of tenderness are remarkably constant in location. A moderate and consistent degree of pressure should be used in digital palpation of these tender points.
FIGURE 21-1
Tender points in fibromyalgia. Suboccipital muscle insertion at base of skull; anterior aspect of intertransverse process spaces at C5-7; midpoint of upper border of trapezius muscle; above scapular spine near medial border of scapula; second costochondral junction; lateral epicondyle; upper outer quadrant of buttocks; posterior aspect of trochanteric prominence; medial fat pad of knee (all bilateral). (From the brochure "Fibromyalgia,” Arthritis Information, Advice and Guidance, Disease Series. Used by permission of the Arthritis Foundation.)
As a guideline to reduce variability in the interpretation of point tenderness, the amount of force applied should be 4 kg (~9 lb), which is the degree of force required to just blanch the examiner’s thumbnail. This amount of pressure does not produce significant tenderness or pain in normal subjects. Some workers recommend that the tender site be palpated using a rolling motion, which may be more effective in eliciting the tenderness. The tender sites can also be examined using a dolorimeter, which is a spring-loaded pressure gauge; however, digital palpation appears to be as effective and accurate. Some investigators have quantitated the degree of tenderness or pain, but the number of tender point sites is more diagnostic. Some patients are tender all over, although still more tender or painful at the specific tender point sites.
Skinfold tenderness may be present, particularly over the upper scapular region. Subcutaneous nodules may be felt at sites of tenderness. Nodules in similar locations are present in normal persons but are not tender.
Fibromyalgia may be triggered by emotional stress, infections and other medical illness, surgery, hypothyroidism, and trauma. It has appeared in some patients with hepatitis C infection, HIV infection, parvovirus B19 infection, or Lyme disease. In the latter situation, fibromyalgia may persist despite adequate antibiotic treatment for Lyme disease, and especially anxious patients may believe that they still have Lyme disease. Disorders commonly associated with fibromyalgia include irritable bowel syndrome, irritable bladder, headaches (including migraine headaches), dysmenorrhea, premenstrual syndrome, restless legs syndrome, temporomandibular joint pain, noncardiac chest pain, Raynaud’s phenomenon, and sicca syndrome.
The course of fibromyalgia is variable. Symptoms wax and wane in some patients, while in others pain and fatigue are persistent regardless of therapy. Studies from tertiary medical centers indicate a poor prognosis for most patients. The prognosis may be better in community-treated patients. In a community-based study reported after 2 years of treatment, 24% of patients were in remission, and 47% no longer fulfilled the ACR criteria for fibromyalgia.
Diagnosis
Fibromyalgia is diagnosed by a history of widespread musculoskeletal pain present for at least 3 months and the demonstration of significant tenderness or pain in at least 11 of the 18 tender point sites on digital palpation (Fig. 21-1). The ACR criteria are useful for standardizing the diagnosis; however, not all patients with fibromyalgia meet these criteria (Table 21-1). Some patients have fewer tender sites and more regional pain and may be considered to have fibromyalgia.
The musculoskeletal and neurologic examinations are normal in fibromyalgia patients, and there are no laboratory abnormalities.
TABLE 21-1
|
THE AMERICAN COLLEGE OF RHEUMATOLOGY 1990 CRITERIA FOR THE CLASSIFICATION OF FIBROMYALGIAa |
|
1. History of widespread pain. Pain is considered widespread when all of the following are present: |
|
a. Pain in the left side of the body |
|
b. Pain in the right side of the body |
|
c. Pain above the waist |
|
d. Pain below the waist |
|
e. Axial skeletal pain (cervical spine or anterior chest or thoracic spine or low back) |
|
2. Pain on digital palpation in at least 11 of the following 18 tender point sites (see Fig. 20-1): |
|
a. Occiput: bilateral, at the suboccipital muscle insertion |
|
b. Low cervical: bilateral, at the anterior aspect of the intertransverse spaces at C5-7 |
|
c. Trapezius: bilateral, at the midpoint of the upper border |
|
d. Supraspinatus: bilateral, at the origin, above the scapular spine near the medial border |
|
e. Second rib: bilateral, at the second costochondral junction, just lateral to the junction on the upper surface |
|
f. Lateral epicondyle: bilateral, 2 cm distal to the epicondyle |
|
g. Gluteal: bilateral, in the upper outer quadrant of the buttock |
|
h. Greater trochanter: bilateral, posterior to the trochanteric prominence |
|
i. Knee: bilateral, at the medial fat pad proximal to the joint line |
|
Digital palpation should be performed with a moderate degree of pressure. For a tender point to be considered positive, the subject must state that the palpation was painful. “Tender” is not to be considered painful. |
aFor purposes of classification, patients will be said to have fibromyalgia if both criteria are satisfied. Widespread pain must have been present for at least 3 months. The presence of a second clinical disorder does not exclude the diagnosis of fibromyalgia.
Fibromyalgia may occur in patients with rheumatoid arthritis, systemic lupus erythematosus (SLE), other connective tissue diseases, or other medical illness. A distinction is no longer made between primary and secondary fibromyalgia (concomitant with other disease), as the signs and symptoms are similar. Fibromyalgia and chronic fatigue syndrome have many similarities. Both are associated with fatigue, abnormal sleep, musculoskeletal pain, impaired memory and concentration, and psychiatric conditions such as less severe forms of depression and anxiety. Patients with chronic fatigue syndrome, however, are more likely to have symptoms suggesting a viral illness. These include mild fever, sore throat, and pain in the axillary and anterior and posterior cervical lymph nodes. The onset of chronic fatigue syndrome is usually sudden; patients are usually able to date the onset. While many patients with chronic fatigue syndrome have tender or painful points, the diagnosis does not require their presence. Patients with fibromyalgia may be misdiagnosed with SLE or Sjögren’s syndrome as these disorders have in common symptoms of musculoskeletal pain, dry eyes, cold hands, and fatigue. The antinuclear antibody (ANA) test may also be positive. The frequency of a positive ANA test in fibromyalgia patients, however, is the same as sex-and aged-matched normal controls. The predictive value of a positive ANA test in patients without characteristic symptoms and objective features of a connective tissue disease is quite low. Discretion is advised before ordering an ANA test. Patients with fibromyalgia may complain of muscle weakness, but on muscle strength testing, they have “giveaway” weakness secondary to pain. Proximal muscle weakness and elevated muscle enzymes distinguish patients with polymyositis. Polymyalgia rheumatica is distinguished from fibromyalgia in an elderly patient by the presence of more proximal muscle stiffness and pain and an elevated erythrocyte sedimentation rate. Patients should be evaluated for hypothyroidism, which may have symptoms similar to fibromyalgia or may accompany fibromyalgia. Disturbed sleep, musculoskeletal pain, and fatigue occur in patients with sleep apnea and restless legs syndrome. A distinguishing feature of sleep apnea is the presence of significant daytime somnolence. These patients should be referred to a sleep laboratory for evaluation and treatment. Myofascial pain syndrome, which involves an area such as the shoulder or neck, may represent a localized form of fibromyalgia (Chap. 22). Some patients with this syndrome progress to fibromyalgia.
The diagnosis of fibromyalgia has taken on a more complex significance in regard to labor and industry issues. This has become a significant issue since it has been reported that 10-25% of patients are not able to work in any capacity, while others require modification of their work. Disability evaluation in fibromyalgia is controversial. The diagnosis of fibromyalgia is not accepted by all. It is hard to evaluate patients’ perceptions of their inability to function. The determination of tender points can also be subjective, on the part of both the physician and the patient, particularly when issues of compensation are pending. Patients also encounter difficulty in having their illness recognized as a disability. Physicians have been placed in the inappropriate role of assessing the patient’s disability. Physicians are not in a position to quantitate disability at the workplace; that is better done by a work evaluation specialist. Better instruments are clearly needed for measuring disability, particularly in patients with fibromyalgia.
Treatment:
Fibromyalgia
Patients should be informed that they have a condition that is not crippling, deforming, or degenerative, and that treatment is available.Pregabalin,a calcium channel alpha2-delta-subunit ligand with analgesic, anxiolytic, and antiepileptic activity, has had demonstrated efficacy for reducing symptoms of pain, disturbed sleep, and fatigue in patients with fibromyalgia. Duloxetine, a serotonin/norepinephrine reuptake inhibitor, has shown benefit for the management of symptoms associated with fibromyalgia in patients with or without major depressive disorder. Milnacipran, a dual norepinephrine and serotonin reuptake inhibitor, was also recently approved by the Food and Drug Administration for the treatment of fibromyalgia.
The use of tricyclics such as amitriptyline (10-50 mg), nortriptyline (10-75 mg), and doxepin (10-25 mg) or a pharmacologically similar drug, cyclobenzaprine (10-40 mg), 1-2 h before bedtime will give the patient restorative sleep (stage 4 sleep), resulting in clinical improvement. Patients should be started on a low dose, which is increased gradually as needed. Side effects of these tricyclics and cyclobenzaprine limit their use;these include constipation, dry mouth, weight gain, drowsiness, and difficulty thinking.Trazodone or zolpidem also improves sleep quality. In patients with restless legs syndrome, clonazepam may be effective. Depression and anxiety should next be treated with appropriate drugs and,when indicated,with psychiatric counseling.
Fluoxetine, sertraline, paroxetine, citalopram, or other newer selective serotonin reuptake inhibitors can be used as antidepressants. Other useful antidepressants are trazodone and venlafaxine.Alprazolam and lorazepam are effective for anxiety. Patients may also benefit by regular aerobic exercises, which are started after patients begin to have improved sleep and less pain and fatigue. Exercise should be of a low-impact type and begun at a low level. Eventually the patient should be exercising 20-30 min, 3-4 days a week. Regular stretching exercises are also very important. Salicylates or other nonsteroidal anti-inflammatory drugs (NSAIDs) only partially improve symptoms. Glucocorticoids have been of little benefit and should not be used in these patients.Opiate analgesics should be avoided. For pain, acetaminophen or tramadol may be useful. Also, gabapentin (300-1200 mg/d in divided doses) may reduce pain. Local measures such as heat, massage, injection of tender sites with steroids or lidocaine, and acupuncture provide only temporary relief of symp-toms.Other therapies that may help to varying degrees include biofeedback, behavioral modification, hypnotherapy, and stress management and relaxation response training. Life stresses should be identified and discussed with the patient, and the patient should be provided with help on how to cope with these stresses. Patients may benefit from a multidisciplinary team approach involving a mental health professional, a physical therapist,and a physical medicine and rehabilitation specialist. Group therapy may be beneficial.
Patients should be well educated about their disorder and taught the importance of self-help. There are patient support groups in many communities. While treatment of fibromyalgia is effective in some patients, others continue to have chronic disease, which is relieved only partially if at all.