Learning Objectives
1. Differentiate between internal and external respiration.
2. Describe the anatomic relationships between the larynx, trachea, and esophagus.
3. Name and describe the ways in which the respiratory system is protected.
4. Diagram the path of air flow in and out of the lungs, identifying the structures involved and their functions.
5. Explain how the mechanisms of inspiration and expiration occur.
6. Describe the pleura and its function.
7. Describe two regulators of breathing and how they function.
8. Describe how the exchange of gases takes place in the alveoli of the lungs.
9. Describe effects of aging on the respiratory system and their nursing implications.
|
IMPORTANT TERMINOLOGY |
||
|
alveolar duct |
inspiration |
pleura |
|
alveolar sac |
intercostal muscles |
pleural cavity |
|
bronchi |
internal respiration |
pleural space |
|
bronchiole |
laryngopharynx |
respiration |
|
cellular respiration |
larynx |
sinus |
|
cilia |
lung |
surfactant |
|
diaphragm |
mediastinum |
trachea |
|
dyspnea |
nares |
ventilation |
|
epiglottis |
nasopharynx |
visceral pleura |
|
eupnea |
oropharynx |
vocal cord |
|
expiration |
parietal pleura |
|
|
external respiration |
pharynx |
|
|
Acronyms |
|
|
ERV |
TLC |
|
FRC |
TV |
|
IC |
URI |
|
IRV |
VC |
|
RV |
Vt |
The respiratory system is responsible for drawing air (containing oxygen) into the lungs, exchanging oxygen for carbon dioxide, and removing carbon dioxide and other gaseous wastes. The lungs depend on the cardiovascular system to contribute actively to the process of gas exchange and to deliver oxygen at the cellular level.
Respiration is the exchange of gases between a person’s external environment and the body’s internal cells. Respiration refers to three processes: ventilation (breathing), gas exchange (in the alveoli of the lungs and in the cells of the body), and oxygen and carbon dioxide transportation (for metabolism, body processes, and waste removal). The air a person takes in through the respiratory system contains approximately 21% oxygen and 0.4% carbon dioxide, and under normal circumstances, this provides an ample oxygen supply for a person’s needs. The air that a person exhales still contains approximately 16% oxygen, but has an increased amount of carbon dioxide (approximately 4.5%).
Structure and Function
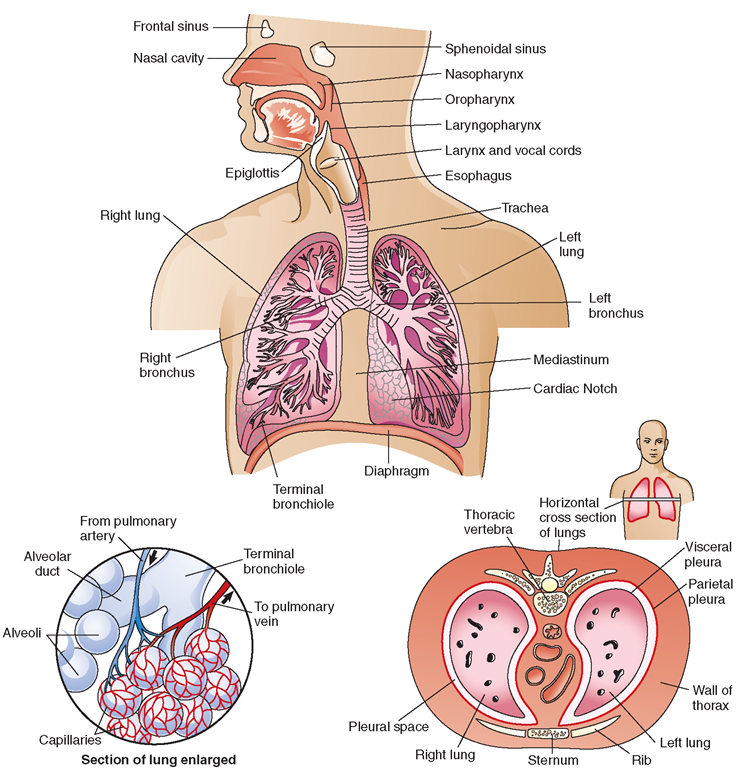
The functions of the respiratory system (Box 25-1) include taking oxygen from the atmosphere, exchanging it for carbon dioxide from the body, and assisting with the regulation of the body’s pH. The respiratory system depends on the circulatory system to transport gases and on the nervous system to receive chemical and nervous stimuli at the brain’s respiratory centers to initiate and control respirations. Figure 25-1 illustrates the respiratory system.
BOX 25-1.
Functions of the Respiratory System
Oxygen-Carbon Dioxide Exchange
♦ Takes in oxygen from outside air
♦ Exchanges carbon dioxide for oxygen in lungs
♦ Exchanges oxygen for carbon dioxide at the cellular level
♦ Eliminates carbon dioxide from body
Acid-Base Balance
♦ Assists in regulating body’s pH
♦ Eliminates some water
Protection
♦ Warms and moistens air before it enters lungs
♦ Mucus in nose traps foreign particles
♦ Coughing and sneezing dislodge foreign particles
♦ Yawning and swallowing help equalize pressures between inner ear and atmosphere
Speech Production
♦ Air passes over vocal cords to produce sound
NCLEX Alert The respiratory system involves the life-sustaining priorities of Airway and Breathing. Be alert to the terminology of normal and abnormal respiratory functioning.
UPPER RESPIRATORY TRACT
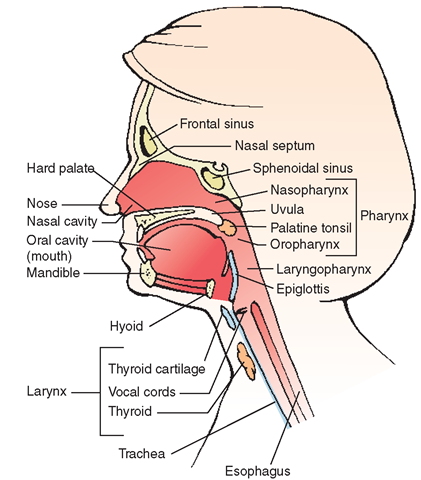
The upper respiratory tract consists of the nose, sinuses, pharynx, larynx, and trachea. Figure 25-2 illustrates the upper respiratory tract. These structures serve as pathways for air to enter and exit the lungs, where exchange of gases takes place. The upper respiratory tract is the entrance to the “conducting area” of the respiratory system.
Nose
Air enters the body through the right and left external nares or nostrils. If for some reason the nares become occluded (e.g., packing of the nose, a foreign object, or swelling), a person can breathe air through the mouth. The nasal septum, a structure consisting of bone and cartilage, divides the internal nose into two sides or cavities. The nerve endings in the septum and in the nasal passages are responsible for the sense of smell. The olfactory nerve (cranial nerve I) carries these nerve impulses to the brain.
FIGURE 25-1 · The respiratory system. Top, upper respiratory structures and the structures of the thorax. Bottom (left), an enlarged section of the lung showing the alveoli and capillary exchange and (right) a horizontal cross section of both lungs indicating the visceral and parietal pleurae and surrounding bones.
FIGURE 25-2 · Anatomy of the upper respiratory tract.
Mucous membrane, richly supplied with blood vessels, lines the nasal cavity. The blood vessels aid in warming and moistening air before it reaches the lungs. Sticky mucus traps dust particles, dirt, and microorganisms from the air. Hairs at the entrance of the nostrils and cilia (tiny hair-like projections) on the membranes serve as filters to remove some foreign particles that otherwise might be carried to the lungs. The cilia all beat in one direction, channeling mucus from the upper respiratory tract into the throat. (Most secreted mucus is swallowed into the digestive system, where hydrochloric acid from the stomach destroys many pathogens.)
Three small bones, the turbinates or conchae, project into the nasal cavity to increase the surface area of the mucous membrane. This increased surface area helps in the warming and filtering of room air. The nasolacrimal ducts, or tear ducts from the eyes, open into the upper nasal cavities, adding lubrication and also causing the “runny nose” that often accompanies crying. (Cartilage is present in the system from the nose to the small bronchi.)
Sinuses
Four cavities called sinuses are found on each side of the nasal area (a total of eight). Mucosa that is continuous with the nasal mucosa lines these sinuses. Sinuses lighten the skull and provide resonance for the voice.
The names of the sinuses correspond with the facial bones in which they are situated. The two largest sinuses are the frontal sinuses (one on each side above the eye socket) and the maxillary sinuses (one on each side of the nose, in conjunction with the maxillary bone). The ethmoidal sinuses lie between the eyes, and the sphenoidal sinuses lie on each side of the nasal cavity in the area of the orbit (eye socket). Figures 25-1 and 25-2 show several sinus cavities.
Nursing Alert The sinuses drain directly into the nasal cavities, which drain into the throat. Because of the direct connection between the sinus cavities and the nasal mucosa, infection in one area can easily spread to the other Excess sinus secretions are often present in a head cold.
Pharynx
Air travels from the nose to the pharynx, a tube-shaped passage for air and food. Consult Figures 25-1 and 25-2 as you read the following descriptions.
Nasopharynx
The section of the pharynx that extends from the nares to the uvula is called the nasopharynx. It is a passageway for air only. In childhood, it contains the adenoids (pharyngeal tonsils) (not shown in the adult pictured). The adenoids are located in the posterior wall of the nasopharynx and, along with the tonsils, assist the body in its immune response to foreign invaders.Enlargement of the adenoids can cause snoring or obstruction of the upper airway. Only rarely does an adult have adenoids; when an individual approaches adulthood, the adenoids usually atrophy (waste away). During the act of swallowing, the soft palate and uvula elevate to block the nasal cavity, preventing food from entering the respiratory system. The auditory (eustachian) tubes connect the nasopharynx with the middle ear (see Fig. 21-3). These eustachian tubes permit air to enter or to leave the middle ear cavities, permitting proper functioning of the tympanic membranes (eardrums) and equalizing pressures between the external environment and the middle ear.
Oropharynx
The oropharynx is the part of the pharynx extending from the uvula to the epiglottis. Commonly called the “throat,” the oropharynx carries food to the esophagus and air to the trachea. Two sets of tonsils are in the oropharynx: the two palatine tonsils are located posteriorly, on each side of the oral cavity, and the lingual tonsils are located at the base of the tongue. The palatine tonsils are the ones commonly removed during a tonsillectomy (see Fig. 25-2). These two sets of tonsils encircle the throat and have a role in the immune system (in addition to the adenoids). Their function is to destroy foreign substances that are inhaled or ingested.
Laryngopharynx
The laryngopharynx is the lowest portion of the pharynx. It extends from the epiglottis to its division into two separate passageways, the larynx (for air) and the esophagus (for food).
Larynx (Voice Box)
From the pharynx, air passes into the larynx, a box-like structure made of cartilages held together by ligaments. The function of the cartilages in the larynx is to keep the airway open at all times. (The largest and most prominent cartilage, particularly in males, is the thyroid cartilage or laryngeal prominence, commonly known as the “Adam’s apple.”) The larynx is located in the midline of the neck.
Nursing Alert In the event of a blocked air way a tracheotomy may be needed. This is an artificial opening, either temporary or permanent, into the trachea.
The larynx serves as an air passageway between the pharynx and the trachea. Although the pharynx acts as a dual passageway for air and food, only air is allowed to pass into the larynx. A lid or cover of cartilage called the epiglottis (“trap door cartilage”) guards the entrance to the larynx. The epiglottis automatically closes when swallowing, preventing food from entering the lower respiratory passage. The glottis is the vocal structure of the larynx, consisting of the true vocal cords and their related openings.
Nursing Alert If a portion of food accidentally becomes lodged in the larynx, coughing can usually dislodge it. If not, the air passage may be blocked; such a blockage can be fatal unless proper emergency treatment is given. (Nurses are most often trained in treating obstructed airway and cardiopulmonary resuscitation.)
Vocal Cords
Within the larynx are the vocal cords (vocal folds), two thin, triangle-shaped reed-like folds (see Fig. 25-2). One end of each cord is attached to the front wall of the trachea; the other end is attached to a tiny cartilage near the back wall of the trachea. These cartilages can move to produce many sounds or can be spread apart to allow silent breathing. As air leaves the lungs and passes over the vocal cords when they are close together, the cords vibrate, and the vibration produces sound, in much the same manner as that of a reed organ. The size of the vocal cords and the larynx varies, accounting for the difference in people’s voices. A man usually has a larger larynx—and therefore a deeper voice—than most women. A voice becomes louder and stronger when a lot of air is forced out rapidly.
Trachea (Windpipe)
Air passes from the larynx into the trachea, a tube approximately 4.5 inches (11 cm) long and 1 inch in diameter in adults. It consists of C-shaped hyaline cartilage and connective tissue and extends from the lower end of the larynx into the chest cavity behind the heart. Here, smooth muscles begin to assist in the passage of air. Immediately posterior to the larynx and the trachea is the tube called the esophagus,which transports food from the pharynx to the stomach.The trachea’s horseshoe-shaped cartilaginous rings provide sufficient rigidity to keep it open at all times for air to pass through. The rings are flexible enough, however, to permit bending of the neck. At the bottom of the trachea, the single tubular system begins to branch (see Fig. 25-1). By the time the tubes reach the alveoli in the lungs, they have branched 20-23 times. Ciliated mucous membrane lines the trachea. As in the nose, mucus in the trachea traps inhaled foreign particles, which waves of cilia carry out of the respiratory tract through the pharynx.
Key Concept The respiratory tract is a common site of infections. Upper respiratory infections (URI) are among the most common infections in the world.