TIMI Risk Score
All-Cause Mortality, New or Recurrent Ml, or Severe Recurrent Ischemia Requiring Urgent Revascularization Through 14 d After Randomization. % scheme that enables a clinician to categorize a patient’s risk of risk of death and ischemic events at the critical initial evaluation. A promising clinical application of this score is identification of a patient for whom new antithrombotic therapies would be especially effective.
|
TIMI Risk Score |
All-Cause Mortality, New or Recurrent Ml, or Severe Recurrent Ischemia Requiring Urgent Revascularization Through 14 d After Randomization. % |
|
0-1 |
4.7 |
|
2 |
8.3 |
|
3 |
13.2 |
|
4 |
19.9 |
|
5 |
26.2 |
|
6-7 |
40.9 |
Table 2. TIMI Risk Score for Unstable Angina/Non-ST Elevation MI
The TIMI risk score is determined by the sum of the presence of 7 variables at admission; i point is given for each of the following variables:
■ age 65 y or older;
■ at least 3 risk factors for CAD;
■ prior coronary stenosis of 50% or more;
■ ST-segment deviation on ECG presentation;
■ at least 2 anginal events in pror 24 h;
■ use of aspirin in prior 7 d;
■ elevated serum cardiac biomarkers.
Prior coronary stenosis of 50% or more remained relatively insensitive to missing information and remained a significant predictor of events.
While ECG manifestations are an important component of diagnosis, one should be aware of the pitfalls of the ECG. Tables 3, 4 and 5 describe the ECG manifestations of ischemic disease.
|
STelevation |
![tmpD-4_thumb[4] tmpD-4_thumb[4]](http://what-when-how.com/wp-content/uploads/2012/04/tmpD4_thumb4_thumb.jpg) |
|
ST depression and T-wave changes |
![tmpD-5_thumb[4] tmpD-5_thumb[4]](http://what-when-how.com/wp-content/uploads/2012/04/tmpD5_thumb4_thumb.jpg) |
Table 3. ECG manifestations of acute myocardial ischemia (in absence of LVH and LBBB)
![tmpD-6_thumb[4] tmpD-6_thumb[4]](http://what-when-how.com/wp-content/uploads/2012/04/tmpD6_thumb4_thumb.jpg) |
![tmpD-7_thumb[4] tmpD-7_thumb[4]](http://what-when-how.com/wp-content/uploads/2012/04/tmpD7_thumb4_thumb.jpg) |
![tmpD-8_thumb[4] tmpD-8_thumb[4]](http://what-when-how.com/wp-content/uploads/2012/04/tmpD8_thumb4_thumb.jpg) |
Table 4. ECG changes associated with prior myocardial infarction
|
False positives |
|
Benign early repolarization |
|
LBBB |
|
Pre-excitation |
|
Brugada syndrome |
|
Peri- /myocarditis |
|
Pulmonary embolism |
|
Subarachnoid haemorrhage |
|
Metabolic disturbances such as hyperkaLaemia |
|
Failure to recognize normal limits for J-point displacement |
|
Lead transposition or use of modified Mason-Likar configuration1A |
|
Cholecystitis |
|
False negatives |
|
Prior myocardial infarction with Q-waves and/or persistent ST elevation |
|
Paced rhythm |
|
LBBB |
Table 5. Common ECG pitfalls in diagnosing myocardial infarction
Management
Patients with an initial ECG reading that reveals new or presumably new ST segment depression and/or T wave inversion, although not considered candidates for fibrinolytic therapy, should be treated as though they are suffering from MI without ST elevation or unstable angina (a distinction to be made subsequently after scrutiny of serial ECGs and serum cardiac marker measurements). In patients with a clinical history suggestive of STEMI and an initial nondiagnostic ECG reading (i.e., no ST segment deviation or T wave inversion), serial tracings should be obtained while the patients are being evaluated in the emergency department.
Emergency department staff can be alerted to the sudden development of ST segment elevation by periodic visual inspection of the bedside ECG monitor, by continuous ST segment recording, or by auditory alarms when the ST segment deviation exceeds programmed limits. Decision aids such as computer-based diagnostic algorithms, identification of high-risk clinical indicators, rapid determination of cardiac serum markers, two-dimensional echocardiographic screening for regional wall motion abnormalities, and myocardial perfusion imaging have greatest clinical utility when the ECG reading is nondiagnostic. In an effort to improve the cost-effectiveness of care of patients with a chest pain syndrome, nondiagnostic ECG reading, and low suspicion of MI but in whom the diagnosis has not been entirely excluded, many medical centers have developed critical pathways that involve a coronary observation unit with a goal of ruling out MI in less than 12 hours.
Once the diagnosis of coronary artery disease is made, the management depends upon the severity of the underlying severity of the disease. The treating physician has to diagnose the clinical scenario appropriately as the treatment largely depends of the initial diagnosis. Stable coronary artery disease could be managed conservatively whereas acute coronary syndrome has to be managed very aggressively. Select patients have to be considered for early invasive strategy too.
The prehospital care of patients with suspected STEMI is a crucial element bearing directly on the likelihood of survival. Most deaths associated with STEMI occur within the first hour of its onset and are usually caused by ventricular fibrillation. Accordingly, the importance of the immediate implementation of definitive resuscitative efforts and of rapidly transporting the patient to a hospital cannot be overemphasized.
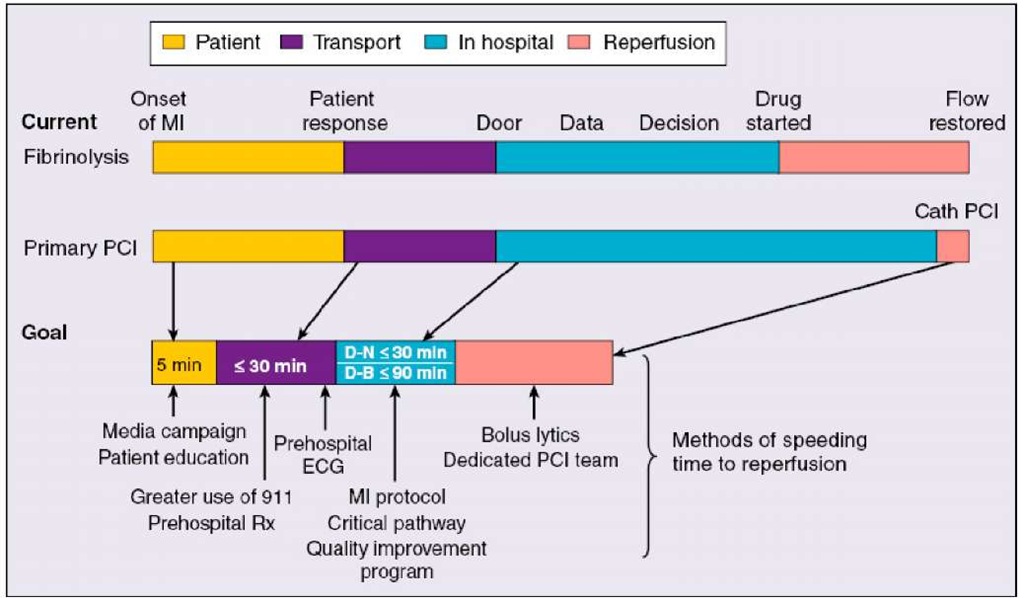
Major components of the delay from the onset of symptoms consistent with acute myocardial infarction (MI) to reperfusion include the following: (1) the time for the patient to recognize the seriousness of the problem and seek medical attention; (2) prehospital evaluation, treatment, and transportation; (3) the time for diagnostic measures and initiation of treatment in the hospital (e.g., "door-to-needle" time for patients receiving a thrombolytic agent and "door-to-balloon" time for patients undergoing a catheter-based reperfusion strategy); and (4) the time from initiation of treatment to restoration of flow (Figure 4). Thrombolytic therapy is vital for early reperfusion and this has been discussed in other topics.
Fig. 4. Adjunctive medical therapy is a critical component of therapy for STEMI and confers benefit in addition to that gained by reperfusion therapies, regardless of method of reperfusion.
Ancillary therapy can be used to facilitate and enhance coronary reperfusion or to limit the consequences of myocardial ischemia. Early, aggressive use of antiplatelet therapies, such as aspirin, and clopidogrel, confers significant additional mortality benefit when given as adjuncts to thrombolysis or PCI. Beta-blockers, angiotensin-converting enzyme inhibitors in appropriately selected patients, and 3-hydroxy-3-methylglutaryl CoA reductase inhibitors (statins) have all been shown to reduce the risk of cardiovascular events and mortality in patients who have STEMI. Therapies such as nitroglycerin and morphine have no mortality benefit but may improve symptoms and reduce ischemic burden. Calcium-channel blockers and prophylactic anti-arrhythmic drug therapy (lidocaine) may increase mortality. The suggested benefit of metabolic modulation at the myocyte level with electrolytes, glucose, and insulin seen in small, early trials has not been reproduced in larger, randomized studies.
Table 6.
Abbreviations: ACS, acute coronary syndrome; BP, blood pressure; CHF, congestive heart failure; CV, cardiovascular; CVA, cerebrovascular accident; HR. heart rate; IV, intravenous; LV, left ventricular: MI, myocardial infarction; NSTE, non-ST-segment elevation; PCI, percutaneous coronary intervention.
Conclusion
Although improvements in the management of patients who have STEMI have led to a decline in acute and long-term fatality rates, reperfusion and ancillary therapies remain underused. Several initiatives (eg. Get With the Guidelines in USA) are designed to improve adherence to guidelines and access to appropriate reperfusion therapies. To date, clinical advancement is judged on achieving and maintaining epicardial artery patency. New fibrinolytics and combination therapies will continue to evolve. There will be technological advances and improvement in operator skills for PCI. The ultimate goal for the management of STEMI remains unchanged: to open occluded arteries quickly in carefully screened patients and in a cost-effective manner.