Damage through excitation and the paradoxical properties of an injured neuron
Usually, although not in every case, damage, evoked by various factors, injures cells through excessive excitation [797, 642, 742]. Necrotic neuronal damage often is a fee paid for excitation. Mild or strong excitations are at the core of injury evoked by various insults. Neuroexcitatory mechanisms are involved in ischemic neuronal injury, in damage due to neurotoxin injections, in mechanical damage, in damage as a consequence of oxygen or glucose deprivation, etc. [331, 337, 799, 832, 1389]. Mediators of the processes related to neuronal damage are excitatory amino acids, especially glutamate, retrograde transmitters, free radicals, intracellular Ca2+, impairment of energy metabolism, intracellular acidification, etc. Intensive influx within the cell of positive ions, Ca2+ and Na+, depolarizes the cell and hurts it. On the other hand, strong depolarization is characterized by a disturbance of homeostasis of intracellular Ca2+ and Na+-influx [437]. Although suppression of Na+-channels exerts neuroprotection [627], Na+ ensures immediate neuronal reactions and does not control long-term cellular homeostasis. However, Na+ metabolism is closely connected with the maintenance of excitability and may serve by a satisfactory indicator of a neuron’s conditions on the scale of damage-protection.
Not only excitation causes damage, but also damage produces changes of excitability. Excitability of neurons decreases during apoptotic degeneration, but membrane potential and AP amplitude remain stable [546]. During necrotic damage, excitability changes in a rather complex way. Nerve fibers develop anomalous excitability at or near the spot of nerve injury. The mechanisms include unusual distributions of Na+ channels, and an increase in intracellular Na+ as well as a deficit in central inhibitory mechanisms following nerve injury [416, 1195, 1439]. Particularly, peripheral axotomy induces long-term hyperexcitability of centrally located neuron soma in diverse species including the Aplysia that serves as the main object for investigation of behavioral plasticity. Long-term hyperexcitability of soma is selectively expressed in the sensory neurons of Aplysia having axons in cut or crushed nerves rather than nearby, uninjured nerves [453]. Hyperexcitablity of axotomized dorsal root ganglion neurons also depends on up-regulation of tetrodotoxin-sensitive sodium channels, which are a basic instrument of excitability [327, 626]. After spinal cord injury, an increase in excitability of neurons may be connected with the shift of the expression of Na+ channels from a high-threshold tetrodotoxin-resistant type to a low-threshold tetrodotoxin-sensitive type [1382]. Sodium up-regulation is usually observed in such cases.
Damage distorts membrane properties. Both injury and excitation evoke depolarization and the growth of excitability in neurons. In dying neurons, a phase of enhanced excitability before death is inevitably transformed to an unexcitable state. Such a property of neural tissue, to be activated under the influence of a harmful impact before death, condemns an injured neuron to display paradoxical properties. An injurious agent (asphyxia, etc.) usually evokes short-term depolarization and excitation, which, after a few minutes, is replaced by a slow compensatory hyperpolarization. This is followed by a persistent depolarization until the membrane potential reaches zero and excitability decreases, even if the injurious agent is removed [81, 797, 1213]. In such cases neurons inevitably die. In certain circumstances, any one of these phases may be absent. For instance, vulnerable neostriatal neurons respond to ischemia with a membrane depolarization and resistant neurons with a hyperpolarization [221].
The same succession of phases may be observed for behavior. For example, morphine injection induces short-term hypophagia, which is followed by a period of hyperphagia and then by persistent hypophagia [144]. The noci-ceptive responses to the formalin test also may be divided in three distinct phases: acute pain, inhibitory (interphase: pain decreases) and tonic pain [454]. Similarly, the ventilatory response to acute hypoxia in mammalian species is biphasic, an initial hyperventilatory response is followed by a reduction in ventilation within 23 minutes below the peak level [558].
During necrotic damage, properties of excitable membrane undergo reorganization because of disturbed ionic equilibrium. Enhanced survival may be sharply, but in a rather complex way, related to membrane potential [405]. Correspondence between excitability of an injured cell and characteristics of its membrane also becomes paradoxical. Spontaneous discharge may be inhibited, when input resistance and the level of membrane potential are not affected [836]. Sometimes, when there are no changes in membrane potential of neurons, input resistance and action potential amplitude of certain identified neurons are increased [13]. Many pharmacological substances affecting the state of neuronal damage-protection also do not alter membrane potential but change the threshold of AP generation or refractoriness [1200, 502]. Damage may selectively affect K +, Ca?+ or Na+ currents [836, 433] and may depend, or not on NO production [551]. These paradoxical properties may be easily explained by non-monotonous changes of excitability during dying.
The process of cell recovery from damage disturbs the coordination between membrane potential and excitability so that a change in excitability after damage is not the direct consequence of a shift in the membrane potential [1213, 1423, 81, 604]. The relationship between threshold and other membrane factors is distorted when measured during ischemia and after its release. During ischemia, there is disproportionately greater refractoriness and, after release of ischemia, supernormality develops and excitability increases. The former could be due to interference with the recovery from inactivation of Na+ channels evoked by some intracellular metabolic disturbance created by ischemia. After recovery, the properties of excitable membrane return to the norm. Processes of neuronal damage and death are illustrated in Fig. 2.1.
Normally hyperpolarization removes the membrane potential from the threshold level of AP and decreases excitability, while depolarization increases it. Specifically, when the membrane potential in a healthy neuron to some extent transitorily decreases, AP height, EPSP amplitude and the threshold of AP generation decline, whereas excitability, refractoriness, AP duration and spontaneous activity enlarge. However, when membrane depolarization is large enough or dragged out, the neuronal state worsens and the above-mentioned correspondences are disturbed. After the occurrence of persistent depolarization when cells are near death, excitability decreases, the AP threshold increases and the Na+-dependent AP decreases and disappears (see Fig. 2.1,bottom). These disturbances are typical not only, because of excessive excitation, but are observed after any harmful impact, although particular details may differ. Mild damage usually increases excitability, while severe damage decreases it and thresholds may increase during depolarization evoked by injury. Paradoxical properties of electrical activity of injured neurons are illustrated in Fig. 2.2.
Fig. 2.1. Metabolic disturbance changes electrical activity in an inspiratory neuron in the brainstem-spinal cord preparation of rat. The glycolytic blocker iodoacetate irreversibly abolishes respiratory rhythm and elicits a hyperpolarization, followed by a prominent depolarization. The alterations depend on Ca2+ entry, K+ -channels, Na+ /Ca2+ exchanger functioning, etc. Dotted line indicates zero level of membrane potential, when the cell is near the death. Spike amplitude decrease irreversibly. Calibration in the figure. The Fig.2.1 was redrawn in accordance with the data [81]
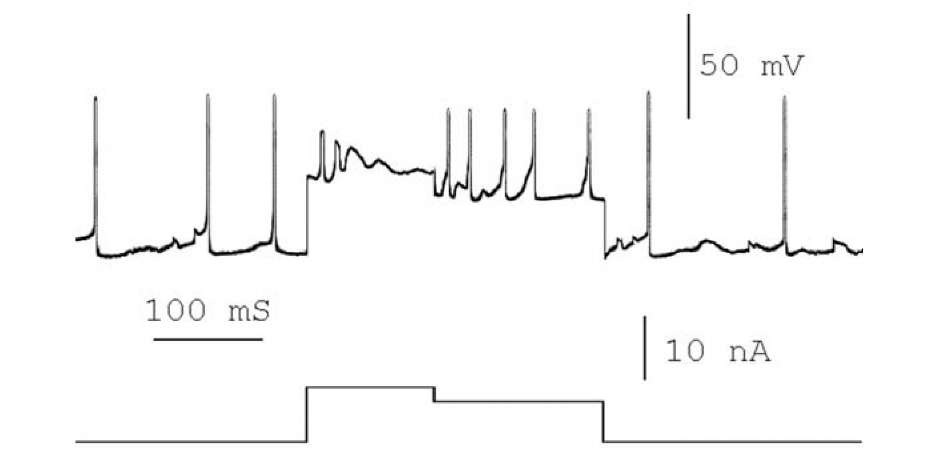
Strong depolarization increased activity and then evoked inactivation, excitability declined and the neuron failed to generate APs. Short-term decrease in the depolarizing current diminished inactivation and AP generation recovered. This phenomenon was discovered by N.E. Vvedensky, more than hundred yeas ago [1311]. Injury of neuromuscular junction leads to development paradoxical state of the tissue. While responses of tissue to stimulus after injury decrease, the higher irritation the smaller becomes the response. Thus, small damage excites, whereas large damage inhibits and when damage is large, responses increase, if strength of stimulus decreases.
Fig. 2.2. Paradoxical effect of decrease in excitatory current to intracellular activity of neuron of the parietal ganglion of Helix. The neuron was hyperdepolarized by the direct excitatory current and failed to generate spikes. Decrease the degree of the hyperdepolarization improved neuron’s state and recovered its possibility to generate spikes. At the top, spontaneous neuronal activity and response to the direct current injection; at the bottom, value of depolarizing current. Calibrations in the figure.
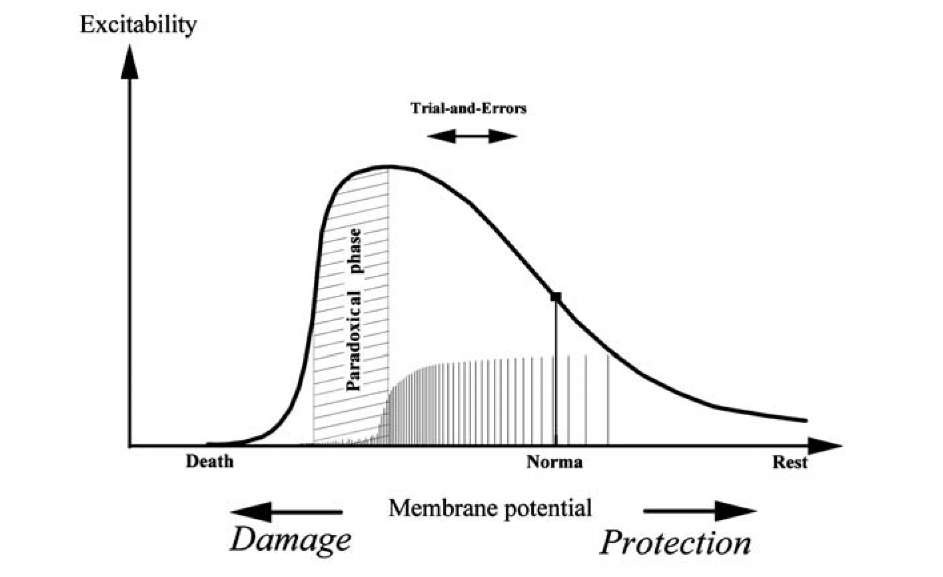
In Fig. 2.3 is schematically presented some changes in neuronal excitability at the scale of damage-protection. An increase in depolarization brings a membrane potential closer to its threshold so that the neuron generates spontaneous spikes and coupling, as we already pointed out, increases. We will demonstrate further that such enhanced activity may serve as the basis of trial-and-error when the brain searches for a way to avoid excitotoxic damage. Additional depolarization, nevertheless, evokes excitotoxic damage and decreases of excitability. Frequency of spike generation increases, while each spike becomes smaller, smaller and eventually is totally blocked. That is, further depolarization injures neurons and leads to a paradoxical phase, in which decreasing the excitation results in an increase in excitability. In such cases, hyperpolarization protects neurons and paradoxically recovers excitability. Thus, compensational recovery of membrane potential leads to generation of action. Compensatory hyperpolarization is in many cases connected with the activation of K+ current. As an example, infusion of K + channel blocker in the hippocampus induces release of glutamate from nerve endings that results in neurodegeneration. Under these conditions, GABA^- mediated transmission may paradoxically increase (!) neuronal excitation [956]. This is explained by the property of GABA receptors to protect cells, not only to inhibit them. Similarly, anoxia (2-5 min) hyperpolarized dopamine-containing neurons through K + current and inhibited spontaneous AP. Block of potassium current lead to anoxia-induced hyperdepolarization and AP inhibition, but neuronal activity recovered after decrease in the hyperdepolarization (one minute after end of anoxia) [836].
Fig. 2.3. A schematic illustration of the dependence of neuronal excitability on excitotoxic influences. Abscissa the shift to damage or protection ( or in the first approximation a membrane potential). Ordinate the change in excitability. A paradoxical phase borders the interval in which hyperpolarization or decrease in the level of damage leads to reaction augmentation. The changes in amplitude and frequency of spikes are shown along the abscissa axe.
Protective hyperpolarization may be also connected with the outflow of K + from a cell. Two-pore-domain K+ channels are a diverse and highly regulated superfamily of channels that are thought to provide baseline regulation of membrane excitability. Moreover, opening of these channels protects neurons against both ischemic and epileptic insults [407]. Another reason for compensatory hyperpolarization may be an augmentation of the electrogenic Na+, K+ pump, such as following release of ischemia. Heightened activity of the electrogenic Na+,K+ pump leads to hyperpolarization [502]. As we already have pointed out, excitatory amino acids are the main mediators of cell damage. Activation of glutamate receptors depolarizes neural cells, ensures enhancement of intracellular Ca2+, and activates G proteins that reorganize cellular metabolism. Besides excitatory amino acids, many other neurotrans-mitters also affect cell damage and, in the first turn, these are the inhibitory amino acids GABA [295, 593] and taurine [573, 697, 1085, 1090, 1387], which are the most abundant inhibitory neurotransmitters in the brain and they act against damage and protect neurons. Some GABA^-agonists provide complete histological protection against hypoxic-ischemic injury [470]. In addition to its direct inhibitory action through the ionotropic GABA^ receptor, GABA exerts a variety of modulatory actions through the metabotropic GABA_g type of receptor by means of G proteins [1024].
GABAergic interneurons in the hippocampus and neocortex contain the calcium-binding proteins parvalbumin and calbindin, preventing damage of these interneurons, when most other neurons eventually cease to live as a result of ischemia [409, 465] or excessive excitation [588]. Excitatory and inhibitory spinal pathways showed different susceptibility to ischemia. Interneu-rons of excitatory segmental pathways are less sensitive to ischemia than mo-toneurons and motoneurons were less sensitive to ischemia than interneurons of inhibitory pathways [655]. This may be determined by the presence of calcium binding proteins. In parvalbumin knockout mice, paired-pulse depression in synapses between interneurons and Purkinje cells of cerebellum converts to paired-pulse facilitation [199], that is, sensitivity to excessive excitation is higher in the absence of calcium-binding proteins. Nevertheless, during regular functioning, GABAergic interneurons undergo intensive damage and death, since they receive strong excitatory input from pyramidal cells and they are intensively replaced by newborn neurons. Pyramidal cells, receiving inhibitory influence from these interneurons are thus protected and more stable. One must recall also that inhibitory GABAergic interneurons are frequently electrically coupled by means of gap junctions.
A cell uses many synaptic pathways for chemical control of damage, not only glutamatergic and GABAergic synapses. Non-amino-acid neurotransmit-ters also influence cell damage-protection. Acetylcholine can induce neuronal damage [929] and, on the other hand, damage leads to a reduction in acetyl-choline receptors, while anticholinergic actions produce protection, evoked by toxicity [210], infection [1204], ischemia [12] and extensive intracellular Ca2+ following some insults [994]. Dopamine [789, 1107] protects cells against damage; dopamine-containing neurons are very stable [803, 1380] and dopamine-receptors are connected with the inhibitory Gj protein [1422]. Serotonin ameliorates cellular damage [1370, 1107], plays a pivotal role in the homeostasis of neural tissue [69] and stimulates cell proliferation. Peptide neurotransmitter substance P also protects neurons [866, 364]. Motivationally relevant substances, neuropeptides and neurohormones also affect the processes of neu-ronal damage, when they act on behavior1. On the other hand, damage increases expression of neuropeptides.
Besides numerous neurotransmitters, neuropeptides and neurohormones, various second and retrograde messengers, also interact with cell damage and protection. Let us consider the roles of these substances in neuronal function, damage, and behavior. However, keep in mind that any (or almost any) factor affecting neuronal behavior, affects neuronal survival, too.
![Metabolic disturbance changes electrical activity in an inspiratory neuron in the brainstem-spinal cord preparation of rat. The glycolytic blocker iodoacetate irreversibly abolishes respiratory rhythm and elicits a hyperpolarization, followed by a prominent depolarization. The alterations depend on Ca2+ entry, K+ -channels, Na+ /Ca2+ exchanger functioning, etc. Dotted line indicates zero level of membrane potential, when the cell is near the death. Spike amplitude decrease irreversibly. Calibration in the figure. The Fig.2.1 was redrawn in accordance with the data [81] Metabolic disturbance changes electrical activity in an inspiratory neuron in the brainstem-spinal cord preparation of rat. The glycolytic blocker iodoacetate irreversibly abolishes respiratory rhythm and elicits a hyperpolarization, followed by a prominent depolarization. The alterations depend on Ca2+ entry, K+ -channels, Na+ /Ca2+ exchanger functioning, etc. Dotted line indicates zero level of membrane potential, when the cell is near the death. Spike amplitude decrease irreversibly. Calibration in the figure. The Fig.2.1 was redrawn in accordance with the data [81]](http://what-when-how.com/wp-content/uploads/2011/06/tmp2339_thumb_thumb.jpg)