Introduction
The infectious cause of the transmissible spongiform encephalopathies (TSEs), or prion diseases, is not yet clearly defined. Although minorities of researchers cling tenaciously to the virus hypothesis, the prion or protein-only hypothesis is now widely accepted by most scientists working in this field (1). When originally formulated, the protein-only hypothesis proposed that the TSE agent was an abnormal infectious form of a host-coded protein (protease-resis-tant protein, or prion protein) that could convert homologous normal forms of the protein into replicates of itself (2).
It has become clear that the infectious agent is unlikely to be this abnormal form of the prion protein acting on its own. A subsequent lack of clarity about what constitutes a prion has led to a number of different notations (PrPSc, PrP*, PrPres) being used to refer either to the infectious particle or the abnormal isoform of PrP, or to both. The principal feature most commonly used to distinguish between the disease-associated forms of PrP and the normal isoform is the relative protease resistance of the abnormal form, compared to the normal PrP isoform. This topic uses the nomenclature of Caughey and Chesebro, in which PrPres is the abnormal form of the PrP and PrPsenis the normal form (3). PrPres is not a prion, which is the word invented to describe the hypothetical agent consisting solely of protein (1,2).
None of the antibodies currently available for routine use in immunocy-tochemistry is able to reliably distinguish between PrPsen and PrPres, but it is frequently stated that pretreatment of sections with formic acid destroys PrPsen (4,5). However, this has not been unequivocally validated, and it is our experience that at least some forms of PrPsen do survive formic acid pretreatment. Because immunocytochemistry alone is unable to determine whether the PrP molecule is in an abnormal or a normal isoform, we use the term "disease-associated PrP accumulation," which is without prejudice as to the protease sensitivity of the abnormal deposits. The advantage of immunocytochemistry compared to other detection methods for PrP, is that it can detect abnormal accumulations of PrP in relation to individual cells, not only at light microscopy but also at subcellular levels.
This topic records, in particular, the ultrastructural similarities between PrP amyloid formation and that of other conventional noninfectious amyloi-doses. As the prion hypothesis has become increasingly accepted, it has become difficult to make mention of other possible causal agents and retain credibility. Nevertheless, we will also briefly comment on a poorly understood group of structures, the so-called tubulovesicular bodies, which are within the appropriate size range, and have some morphological similarity to conventional viruses, and have still not been molecularly characterized.
PrP Aggregation and Fibrillization
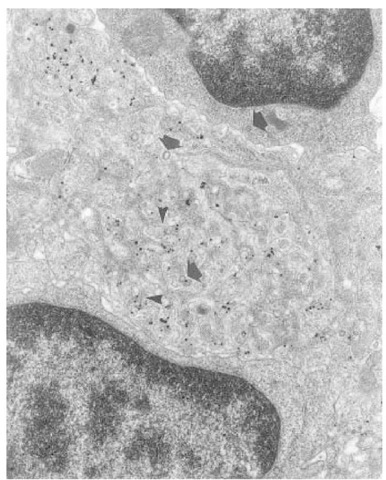
One of the hallmark features of the pathology of TSEs is the formation of amyloid plaques (6-8), which are numerous in some murine models and in some forms of the human TSEs, most notably kuru and variant Creutzfeldt-Jakob disease (vCJD). The sites and deposition, form and structure of the amyloid plaques is under host and agent control (7,9). Most plaques are formed in association with neurons, but cerebrovascular plaques, probably resulting from infection of endothelial cells (10) form in natural sheep scrapie and in the 145Y stop mutation of human Gerstmann-Straussler-Scheinker syndrome (GSS) (11), and in a murine chronic-wasting disease model. Subependymal and sub-pial plaques may be commonly found in some murine models. However, plaques are not found in some TSE diseases, such as in bovine spongiform encephalopa-thy (BSE) (12,13). Ultrastructure shows that classic plaques are composed of a stellate array of bundles of amyloid fibrils surrounded by reactive astrocytes and microglia (14-16). It is these bundles of amyloid fibrils that result in the typical staining patterns of amyloid, such as congophilia and birefringence, under polarized light. Immunogold staining has confirmed that the amyloid present in these plaques is composed mostly of disease-specific PrP (Fig 1; 14,15).
Amyloid plaques are initially formed at focal points along the length of den-drites, and possibly along axons at nodes of Ranvier. These plaques, which we call "primitive plaques," are visible as round or oval areas of immunostaining, when examined by light microscopy but they do not show conventional tinctorial staining patterns of amyloid (15,16).
Fig. 1. Electron microscope micrograph of a classic or kuru-type plaque located in the cerebral cortex of an 87 V scrapie-infected mouse. The preparation has been stained using an immunogold silver method, which reacts with PrP. The plaque shows the characteristic stellate appearance formed by radiating bundles of amyloid fibrils, which are decorated with immunogold silver reaction product, indicating that the fibrils are composed of PrP.
Multiple plaques are often formed along the length of the primary dendrite of cerebrocortical and hippocampal pyramidal neurons. Ultrastructurally, these primitive plaques show accumulation of PrP at the plasmalemma of dendrites (15). This PrP is not in a visibly aggregated form (preamyloid), and diffuses away from the point of release, spreading through the extracellular space to surround other neurites and glia of the adjacent neu-ropil (15-17).
Although the electron microscope does not allow resolution of individual molecules, or even of small multimers of PrP, soluble forms of PrP have been found in tissue culture and in the cerebrospinal fluid of CJD patients (18). It is therefore likely that the diffusable preamyloid PrP, revealed by immunogold reaction in the electron microscope is in a soluble form. In many neuroana-tomical areas, the preamyloid PrP initially released into the extracellular space does not at first result in morphological evidence of pathology, either by light or electron microscopy. It does not elicit an astroglial or microglial response, and is not found in association with neuritic pathology, neuroaxonal dystrophy, or neuronal loss. (Similarly, in spleen, PrP is initially released without evident changes in follicular dendritic cells [19]).
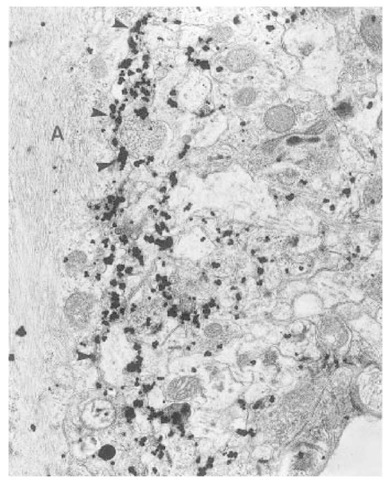
Extensive zones of diffusion around dendrites, in the absence of aggregation, suggest that the preamyloid PrP release and diffusion may occur over a long period of time. The formation of individual fibrils occurs within the extracellular space often at some distance from the releasing cell or dendrite (16,20,21) . Once fibrillar amyloid becomes visible, there appears to be a rapid acceleration of fibril formation, and single fibrils are found throughout the zone of extracellular PrP accumulation (15,16,21). The appearance of both aggregated and fibrillar PrP is associated with a increased astroglial and microglial response (21). In addition, marked fibrillization coincides with evidence of increased receptor-mediated endocytosis, as evidenced by increased coated (presumed clathrin-coated) pit activity. Immunoreaction to PrP may be seen in some of these coated pits (17,21). These features are also seen in association with fibrillization of PrP around follicular dendritic cells of the spleen (19; Fig. 2). The increased clathrin-coated activity is not seen for preamyloid PrP accumulations. These findings suggest that abnormal forms or aggregates of PrP bind to receptors at the cell surface of neurons, glia, follicular dendritic cells and lymphocytes.
Because none of the antibodies currently available for immunocytochemis-try is able to discriminate between normal host-coded PrPsen and PrPres, it is not clear whether the preamyloid forms of PrP or the fibrillar forms of aggregated PrP contain PrPres. However, it is well established that proteins that form amyloid fibrils contain a high proportion of P-pleated sheet, and it is therefore reasonable to assume that the PrP forming amyloid fibrils is abnormally configured, relative to PrPsen, and contains a high proportion of P-pleated sheet. The PrPres detected by immunoblotting are N-terminally truncated near the octarepeat segment of the normal protein (22). However, both the preamyloid forms of PrP and the PrP that forms the amyloid plaques of murine scrapie and cerebrovascular amyloid of sheep contain the N-terminus of the PrP molecule (10,23). The intensity of the immunoreaction with the N-terminal antibodies indicates that both preamyloid PrP and fibrillar PrP are composed mostly or entirely of the whole-length form of the protein.
Fig. 2. Scrapie-infected, highly reactive cytoplasmic processes (dendrites) of a folli-cular dendritic cell from the spleen of an ME7-infected mouse (immunogold silver method for PrP). The deposition of the immunogold reaction indicates that there is marked accumulation of PrP in the extracellular space around the cytoplasmic processes of the infected cell. Amyloid fibrils (arrowheads) are also present in the extracellular space, and both the dendrites of the follicular dendritic cell and adjacent lymphocytes show numerous structures morphologically identified as clathrin coated pits (arrows).
The relationship between the N-terminally truncated PrPres and immunodetected PrP is therefore unclear, but it is likely that the acquisition of protease resistance follows aggregation of the protein and that most N-terminal truncation of disease associated PrP occurs after biochemical treatment of the extracted protein. It is therefore possible that the PrP released into the extracellular space, which does not damage tissue, is in a protease sensitive form of the protein, and it is the local conditions of excess concentration of PrPsen that induce aggregation, fibrillization, and acquisition of protease resistance.
Two models have been proposed to explain the conversion of PrPsento PrPres: the heterodimer model, and seeded polymerization (see ref. 24 for review). It has previously been suggested (25) that PrPres may convert to PrPsen via a heterodimer molecule. However, previous studies (26,27) have shown that the sequential dilution of PrPres, when combined with radio-labeled PrPsen, results in a complete elimination of the converting activity. This suggests that PrPres is an ordered oligomeric seed (i.e., a particle many times larger than a monomer or a dimer).
A heterodimeric conversion of PrPsen to PrPres is not dependent on concentration of reagents, and would take place either within the cell or at the cell surface. In contrast, seeded polymerization will occur as the concentration and kinetics of PrPsen to PrPres conversion reach a critical concentration, when the amounts of disease-specific PrP reach the appropriate concentration. That is, in typical nucleation-dependent polymerization of amyloid, polymer is not observed until the monomer concentration exceeds a certain level (the critical concentration) (24). That diffusion of a preamyloid PrP is observed followed by fibril formation, then rapid generalized formation of fibrils and mature amyloid, is consistent with the seeded polymerization mechanism of classic amyloid, and inconsistent with the heterodimeric model.
In Alzheimer’s disease, amyloid also forms within the neuroparenchyma, where Ap amyloid is dependent on pH. Sedimentable aggregates of Ap 1-40, grown at pH 5.8, have different properties from aggregates grown at pH 7.4. This feature is reminiscent of the different properties of PrP obtained from different strains of scrapie (28). The situation in plaques found in GSS is different than that of scrapie, in that the PrP at the center of plaques is N-termi-nally truncated (29-31). The proteins forming plaques in GSS patients may be different from the PrP found in normal hosts, and there may therefore be differences in PrP processing in inherited and infectious forms of the TSE diseases (32,33). PrP molecules, containing mutations associated with familial TSEs, exhibit altered metabolism, and, when expressed in some uninfected tissue culture cells, may show increased aggregation and protease resistance reminiscent of PrPres (34,35). Even nonmutated hamster PrPsen shows a tendency to aggregate, when expressed as a dimer (36).
Patterns of PrP Accumulation and Cellular Tropism of Scrapie
It has long been known that different patterns of neuropil vacuolation have been found in different sheep breeds and in mice (37,38). The pattern of vacuolation (lesion profile), in highly inbred stains of mice infected with limiting-dilution, cloned agent strains, produces highly reproducible selective targeting of lesions. The lesion profile, along with incubation period (determined in groups of S7 and P7 mouse strains), has been used to characterize agent strains (39). The neuroanatomical pattern of vacuolation is mirrored by highly distinctive patterns of PrP accumulation (38,40). The nature of PrP staining seen within different neuroanatomical areas of the brain is also distinctive (16,17). PrP accumulation is most commonly found as localized, diffuse, finely punctate staining. In addition, perineuronal and intraneuronal, periglial, subpial, subependymal, and localized diffuse granular patterns of PrP staining may also be seen in sheep, cattle, cats, and mice and as discussed in Subheading 2., as plaques.
Perineuronal patterns of PrP accumulation are found in natural sheep scrapie, in BSE, in feline spongiform encephalopathy (FSE), and in some murine models. Such patterns are found in many neuroanatomical nuclei, commonly in the reticular formation, in cattle and sheep. In 87V murine scrapie, perineuronal patterns of PrP accumulation are found around neurons of the lateral hypo-thalamus. The perineuronal pattern is often not confined to the perikaryonal cytoplasm, but may extend to delineate dendrites and axons. Ultrastructurally, PrP is found around the cell, in association with the plasmalemma and adjacent extracellular space of the neuron. As described above, the cells that release PrP into the neuropil are not morphologically abnormal, but can be electrophysi-ologically normal (41).
The PrP released from scrapie-infected neurons accumulates in the surrounding neuropil, where it is found in the extracellular space around cellular processes (15,17,21). The processes include neurites, glial cells, and myelin sheaths. The PrP that accumulates is not visibly aggregated, and, in many neuroanatomical areas, does not cause tissue changes (Fig. 3). However, following some unknown stimulus, extracellular disease-associated PrP accumulations form visible electron-dense aggregates within the extracellular space. Following initial aggregation, the PrP then forms individual fibrils. Initially, these are organized haphazardly, but eventually small bundles of amyloid fibrils are seen. Once aggregation starts, fibrillization appears to follow quickly, and sites that initially had only preamyloid PrP such as the immediate perikaryonal neuropil, will form fibrils (15,21). Once aggregation within the extracellular space begins, there is a marked glial response, with increased numbers of astrocytic processes containing abundant intermediate filament bundles. Microglial activation is also prominent. Aggregated and fibrillar PrP binds other extracellular matrix compounds, such as highly sulphated gly-cosaminoglycans (42). As was also seen in plaque formation, these features suggest that aggregated and fibrillar forms of PrP are damaging to the neuropil, although the preamyloid forms of PrP are not invariably damaging.
Fig. 3. A scrapie-infected neuron (N) and adjacent neuropil from the lateral hypothalamus of an 87 V scrapie-infected mouse (immunogold silver method for PrP). There is marked PrP accumulation within the neuropil. The immunogold reaction is associated with opposing plasmalemmae of contiguous processes (mostly axon terminals and dendrites), suggesting a location to the extracellular space. (The 10 nm immunogold method provides more accurate localization of reaction product, and confirms this distribution). There is no morphologically discernible alteration to the structure of the neuropil associated with this disease-specific PrP accumulation.
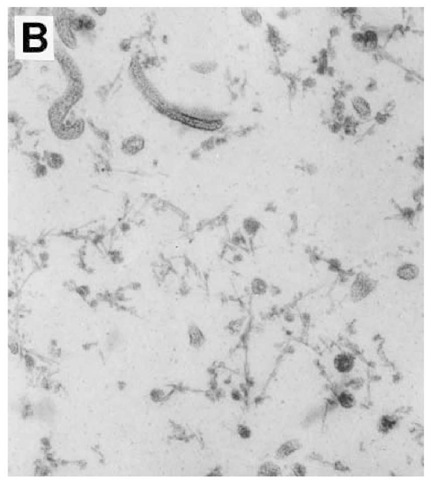
PrP accumulation, in association with other cell types in the appropriate disease model (diffuse, periglial and periependymal patterns), appears to follow a similar sequence of events, i.e., PrP accumulation begins initially as release of PrP from the plasmalemma into the extracellular space. PrP accumulates around the presumptive infected cells, only subsequently becoming aggregated and forming fibrils, which indicates that several cell types within the central nervous system, including astroglia (Fig. 4), ependymal cells, and neurons, may become infected with scrapie.
Fig. 4. Part of a reactive astrocyte perikaryon (A) adjacent to the corpus callosum of a 301V scrapie-infected mouse (immunogold silver method for PrP). The astrocyte cytoplasm has abundant intermediate filaments. Preamyloid PrP accumulation, revealed by the immunogold reaction deposit, is present at the plasmalemma of the astrocyte (arrowheads). PrP accumulation is also present in the adjacent neuropil, suggesting release and diffusion of disease-specific PrP by the infected astrocyte.
Although we have not studied the subcellular patterns of PrP accumulation for perivascular plaques, in sheep these plaques begin as endo-thelial cell infections. Subpial and perivascular patterns of PrP accumulation in sheep are a special case of astrocytic infection, as PrP accumulates in association with the glial limitans.
Fig. 5. (A) The ventricular borders of two ependymal cells from a 237K infected hamster are shown. There is a focal area of fibril accumulation (immunolabeling not shown), indicated by arrowheads, within the ventricular space. Stained with uranyl acetate and lead citrate.
Within a single infected sheep brain, areas representative of neuronal, astroglial, endothelial, and ependymal cellular infections may be detected. Although neuronal, glial, and ependymal infection may occur following transynaptic spread, or simply following bulk flow through the central nervous system, endothelial infection must be acquired by hematogenous infection.
In the case of diffuse patterns of PrP accumulation, such as occurs for example in the hippocampus of the ME7-infected mouse, all neurons within a particular neuroanatomical region appear to release PrP (21). In some brain areas, diffuse staining patterns of PrP accumulation, seen prior to terminal disease, may become dense, localized, granular patterns of PrP accumulation at terminal disease.
Fig. 5(B) The ventricular deposit shown in (A), but at higher magnification. This confirms the fibrillar nature of this ventricular deposit. Stained with uranyl acetate and lead citrate.
Granular patterns of PrP accumulation correlate ultra-structurally with widespread PrP aggregation and fibrillization within the extracellular space. This is invariably associated with marked gliosis, and sometimes with widespread neuronal loss. PrP release from ependymal cells in sheep, and in 263K infected hamster, forms amyloid fibrils within the extracellular space. Ependymal cells release PrP from their ventricular border, and subsequently form fibrils within the ventricular space (Fig. 5), which suggests that the requirement for extracellular matrix components to form fibrils may not be obligate.
Intracellular PrP is found within macrophages of lymph nodes and in astro-cytes, microglia and in Kohler cells of the choroid plexus and ventricle (15,43). All of these cells are known to have phagocytic properties, and to be involved in managing removal of degenerate or toxic products from tissue. In all of these cell types, PrP was located to lysosomes. We suggest that abnormal or excess PrP may elicit microglial and macrophage activation. These cells are then stimulated to internalize abnormal or excess PrP from the surrounding extracellular space and to initiate degradation of the disease-specific form of PrP. Evidence is emerging, from our studies of sheep lymph nodes, that the PrP present in the lysosomal compartment may express different epitopes from PrP in extracellular sites.
Disease-specific intracellular accumulations of PrP are also found in neurons but the subcellular localization of such accumulations has not yet been achieved by electron microscopy and the significance of such intracellular accumulations is unclear. However, in the ME7 model, there is some evidence that PrP may accumulate within neuronal cytoplasm at early stages of infection, but is present extracellularly and absent from the intracellular compartment at later stages of disease. Such a change in subcellular localization could be caused by altered regulation of PrP production at early stages of infection (44).