Introduction
Prion diseases are fatal neurodegenerative disorders of humans and animals, which result from the conformational conversion of a normal, cell surface glycoprotein (PrPC) into a pathogenic isoform (PrPSc) that is the main component of infectious prions (1,2). Familial prion diseases, which include 10% of the cases of Creutzfeldt-Jakob disease and all cases of Gerstmann-Straussler syndrome and fatal familial insomnia, are linked in an autosomal dominant fashion to point and insertional mutations in the PrP gene on chromosome 20 (3,4). These mutations are presumed to favor spontaneous conversion of PrP to the PrPSc state. One way to experimentally model familial prion diseases is to express PrP molecules carrying disease-associated mutations in either cultured mammalian cells or transgenic mice. The authors review their own work using these two kinds of model systems, which have provided complementary information about the PrPC^PrPSc conversion process, and about the pathogenic effects of mutant PrP.
Cultured Cells Convert Mutant PrPs to a PrPSc-Like State
We have created stably transfected lines of Chinese hamster ovary (CHO) cells that express mouse PrP (moPrP) molecules carrying mutations homologous to seven different pathogenic mutations of humans. As a negative control, cells have also been analyzed that express moPrP with a substitution of valine for methionine at codon 128, homologous to a nonpathogenic polymorphism at codon 129 in human PrP.
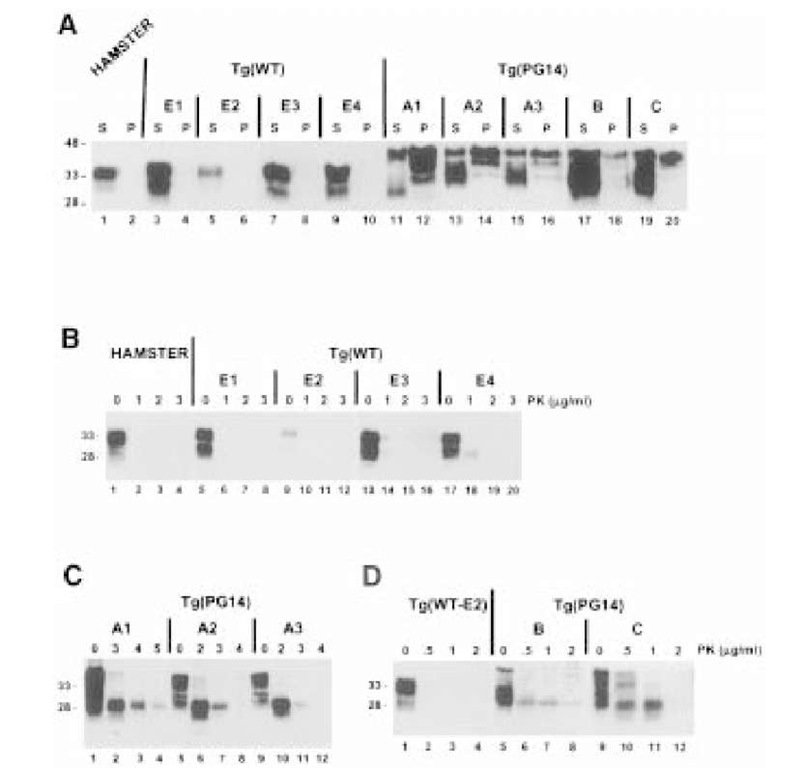
The authors find that moPrPs carrying pathogenic mutations acquire all of the biochemical hallmarks of PrPSc (5-7). PrPSc can be distinguished operationally from PrPC by several biochemical properties. One commonly used property is insolubility in nondenaturing detergents, which can be assayed by subjecting detergent lysates to ultracentrifugation. Although most of the wild-type PrP remained in the supernatant under these conditions, the majority of each of the PrPs carrying a pathogenic mutation was found in the pellet (Fig. 1A). As expected, M128V moPrP behaved like the wild-type protein. A second characteristic of PrPSc is resistance to proteolysis, which is manifested by production of protease-resistant core fragment (PrP 27-30) upon treatment with protein-ase K. Treatment of the mutant PrPs with 3.3 ^g/mL proteinase K for 10 min resulted in production of a PrP27-30 fragment; under the same conditions wild-type and M128V moPrPs were completely digested (Fig. 1B). Immunoblotting with sequence-specific antibodies demonstrated that the PrP27-30, fragment is cleaved just after the octapeptide repeats, which is the same region where authentic PrPSc is cleaved.
Analysis of transfected CHO cells expressing mutant PrPs has provided several important insights into the cell biology of PrPSc, as described below.
Membrance Topology of Mutant PrPSc
PrPC is attached to cell membranes by a C-terminal glycosylphosphatidyli-nositol (GPI) anchor, and can be released by cleavage of the anchor using bacterial phosphatidylinositol-specific phospholipase C (PIPLC). The nature of the membrane attachment of PrPSc, however, has been a matter of uncertainty. Chemical analysis of the purified protein demonstrates that PrPSc possesses a C-terminal GPI anchor (8). Unlike PrPC, however, PrPSc is not releasable by PIPLC from brain membranes or from the surface of scrapie-infected N2A cells (5,9-11).
Fig. 1. PrPs carrying disease-related mutations are detergent-insoluble and protease-resistant when expressed in cultured CHO cells. (A) CHO cells expressing wild-type and mutant mouse PrPs were labeled with [35S]methionine for 20 minutes and then chased for 3 hours. Detergent lysates of the cells were centrifuged first at 16,000 g for 5 min, and then at 265,000g for 40 min. PrP in the supernatants and pellets from the second centrifugation was immunoprecipitated and analyzed by SDS-PAGE. PrP-specific bands were quantitated using a Phosphor-Imager, and the percentage of PrP in the pellet was calculated. Each bar represents the mean ±SD of values from three experiments. Values that are significantly different from wild type PrP by t-test (p < 0.001) are indicated by an asterisk. PrPs carrying disease-related mutations sediment (are detergent-insoluble), while wild type and M128V PrPs remain largely in the supernatant. Human homologues of the mutant PrPs analyzed here are associated with the following phenotypes: PG14 (9-octapeptide insertion), CJD-vari-ant; P101L, GSS; M128V, normal; D177N/Met128, FFI; D177N/Val128, CJD; F197S/ Val128, GSS; E199K, CJD. (B) CHO cells expressing each PrP were labeled for 3 h with [35S]methionine, and chased for 4 hours. Proteins in cell lysates were either digested at 37°C for 10 minutes with 3.3 ^g/ml of proteinase K (+ lanes), or were untreated (- lanes), prior to recovery of PrP by immunoprecipitation. Five times as many cell-equivalents were loaded in the + lanes as in the – lanes. Molecular weight markers are in kilodaltons.
Our analysis of mutant PrPs in cultured CHO cells has shed new light on the issue of the membrane attachment of PrPSc. Mutant PrPs, like PrPSc from infected brain, are not released from membranes by treatment with PIPLC (12). This property does not result from absence of a GPI anchor structure, because the mutant PrPs metabolically incorporate the anchor precursors [3H]ethanolamine, [3H]palmitate, and [3H]stearate. Although the authors originally postulated that mutant PrPs possessed a secondary mechanism of membrane attachment, in addition to their GPI anchors (12), more recent evidence suggests that the mutant molecules are resistant to PIPLC release, because their GPI anchors become physically inaccessible to the phospholipase as part of their conversion to the PrPSc state (13). This conclusion is based on failure of PIPLC to quantitatively remove [3H]palmitate label from the proteins, or to render them hydrophilic by Triton X-114 phase partitioning. Resistance to cleavage is observed when PIPLC is applied to intact cells, as well as when treatment is carried out after lysis in nondenaturing buffers. However, denatur-ation in sodium dodecyl sulfate renders the GPI anchor of the mutant PrPs susceptible to cleavage, suggesting that PIPLC-resistance depends on the native structure of the protein. We now view PIPLC resistance as being an operational property analogous to protease-resistance, and postulate that it reflects an alteration in the structure of PrP attendant on conversion to the PrPSc state.
Although most PrPC molecules are attached to the cell membrane exclusively by a GPI anchor, it has been reported that there exists a subpopulation that displays a transmembrane orientation. Two transmembrane species of PrP have been identified, each with the same membrane-spanning segment (residues 112-135), but with opposite orientations of the polypeptide chain (14,15). It has recently been suggested (16) that one of these species (CtmPrP, which has its C-terminus in the endoplasmic reticulun [ER] lumen) is the primary effector of neurodegeneration in both inherited and infectious cases of prion diseases, since mice carrying certain mutations in the transmembrane region, as well as those infected with scrapie, showed increased amounts of CtmPrP (16). In contrast, our own results suggest that CtmPrP is unlikely to be part of a general pathogenic pathway, because disease-associated mutations outside of the transmembrane domain do not increase the amount of this form (17).
Kinetics and Subcellular Localization of Mutant PrPSc Synthesis
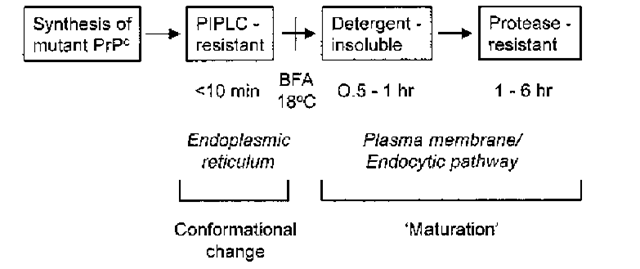
We have used transfected CHO cells to identify intermediate biochemical steps in the conversion of mutant PrPs to the PrPSc state (18). The strategy was to measure the kinetics with which three PrPSc-related properties (PIPLC resistance, detergent insolubility, and protease resistance) develop in pulse-chase labeling experiments. This has allowed definition of three steps in the conversion process (Fig. 2). The earliest biochemical change that could be detected in mutant PrP, one that was observable within minutes of pulse-labeling cells, was the acquisition of PIPLC resistance, a property that was revealed by partitioning of the phospholipase-treated protein into the detergent phase of Triton X-114 lysates, or by its binding to phenyl-Sepharose. The second step is acquisition of detergent insolubility, which is not maximal until 1 h of chase (6), suggesting that it occurs after the acquisition of PIPLC-resistance.
Fig. 2. A scheme for transformation of mutant PrPs to a PrPSc state. Mutant PrPs are initially synthesized in the PrPC state, and acquire PrPSc properties in a stepwise fashion as they traverse different cellular compartments. PIPLC-resistance, which develops in the ER, reflects folding of the polypeptide chain into the PrPSc conformation. Detergent-insolubility and protease-resistance, which develop upon arrival at the plasma membrane or along an endocytic pathway, result from intermolecular aggregation (“maturation”). The times given underneath the boxes indicate when after pulse-labeling the corresponding property is detected. Addition of brefeldin A (BFA) to cells or incubation at 18°C, treatments which block movement of proteins beyond the Golgi apparatus, inhibit acquisition of detergent-insolubility and protease-resistance but not PIPLC-resistance.
Detergent insolubility presumably reflects aggregation of PrP molecules, and by sucrose gradient fractionation aggregates were detected ranging in size from 4S (monomeric) to over 20S (>30 PrP molecules). The third step is acquisition of protease-resistance, which is not maximal until several hours after labeling (6). We have hypothesized that the fundamental conformational change that underlies conversion of mutant PrPC into PrPScis reflected in the acquisition of PIPLC resistance, with detergent insolubility and protease resistance being secondary properties that develop sometime after the initial molecular conversion.
Our kinetic studies suggest that individual steps in the formation of PrPSc may take place in at least two different cellular locations (Fig. 2). Because mutant PrPs become PIPLC-resistant within minutes of synthesis in pulse-labeling experiments, this early step must take place in the ER. Consistent with this conclusion, acquisition of PIPLC resistance is not affected by treatment of cells with brefeldin A, or by incubation at 18°C, which are manipulations that block exit of proteins beyond the Golgi (18). In contrast, detergent insolubility and protease resistance, which do not develop until later times of chase, and are reduced by brefeldin A and 18°C incubation, are likely to be acquired after arrival of the protein at the cell surface, either on the plasma membrane itself or in endocytic compartments. The idea that the generation of PrPSc from mutant PrPs may begin in the ER is theoretically appealing, because of the well known role of this organelle in protein folding. It is also reasonable to suggest that ER chaperones are good candidates for the hypothetical cellular co-factors that are widely thought to play an important regulatory role in prion synthesis (19).
Generation of Tg Mice Expressing a Mutant PrP
To extend the cell culture work, and to investigate the properties of mutant PrP in an in vivo setting, we constructed mice bearing a moPrP transgene that contains a nine-octapeptide insertional mutation (20,21). The human homolog of this mutation, which is the largest insertion thus far described in the PrP gene, has been found in two patients (one British and one German) who were afflicted with an illness characterized by progressive dementia and ataxia, and, in the one autopsied case, by the presence of PrP-containing amyloid plaques in the cerebellum and basal ganglia (22-24). The transgenic mice model key clinical and neuropathological features of human familial prion diseases, and unlike other mice harboring PrP transgenes (14,25-28), they spontaneously accumulate PrPSc in their brains. Analysis of these mice has provided important insights into the natural history and pathogenesis of familial prion diseases.
Neurological Symptoms of Tg(PG14) Mice
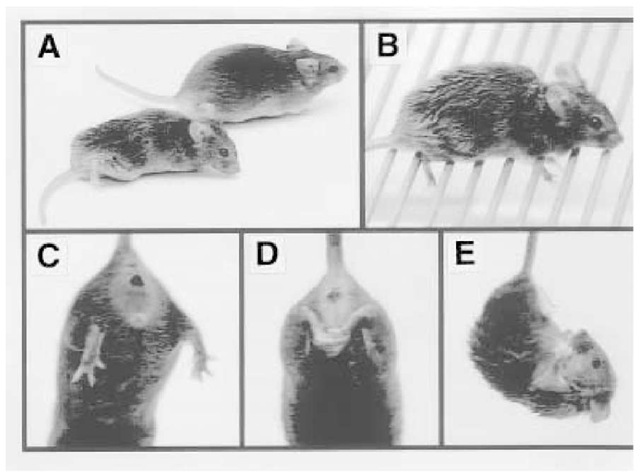
Tg(PG14) mice from the A2 and A3 lines (both of which express mutant PrP at levels similar to that of endogenous PrP) develop a progressive and ultimately fatal neurological disorder characterized by ataxia, kyphosis, foot-clasp reflex, waddling gait, difficulty righting, and weight loss (Fig. 3; 20,21). Similar symptoms were also observed in a founder (A1) that did not breed, and that expressed PG14 PrP at 4x the level of endogenous PrP. In contrast, Tg(WT) mice which express wild-type PrP at even higher levels (3-4x endogenous PrP), remain healthy. We observed that breeding the transgene array to homozygos-ity dramatically accelerated the onset of disease (from 235 ± 10 to 68 ± 9 d of age), and shortened its duration (from 154 ± 14 to 49 ± 11 d). This effect is probably attributable to the twofold higher expression of PG14 PrP in homozy-gous, compared to heterozygous, mice. This explanation is consistent with our finding that the Tg(PG14) B and C lines, which express low levels of the mutant protein (15% of the endogenous PrP level), do not develop a neurological disorder within the lifespan of the animals. Taken together, these results indicate that overexpression of wild-type PrP does not produce neurological dysfunction, and that development of the disease in Tg(PG14) mice is related to the expression level of the mutant protein.
Neuropathological Abnormalities in Tg(PG14) Mice
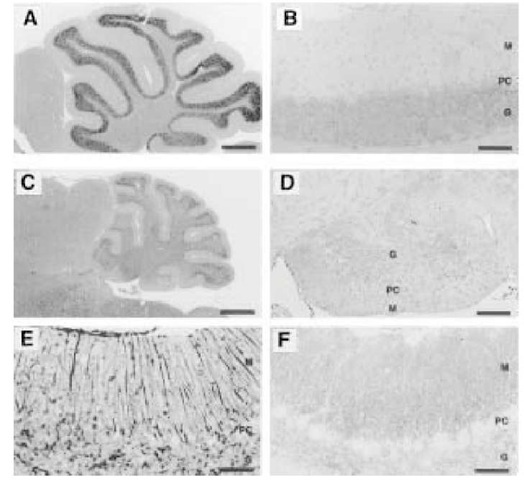
Several pathological changes were observed in the A2 and A3 lines of T(PG14) mice, and in the A1 founder (20,21). The most obvious was a massive degeneration of cerebellar granule cells, which begins by 30 d of age in Tg(PG14+’+) mice, and eventually results in severe atrophy of the cerebellum (Fig. 4A-D).
Figure 3. (A) Neurological symptoms in Tg(PG14) mice. (A) Tg(PG14-A3)/Prn-p0/0 mouse at 84 days of age (left), and Tg(WT-E1)/Prn-p0/0 mouse at 89 days of age. Note the ataxic posture of the PG14 mouse with hind limbs extended, the hunchback orientation of the body, and the ruffled appearance of the coat. (B) The Tg(PG14-A1) founder at 319 days of age is completely incapable of ambulating on a metal grill. Normal mice walk easily on the grill and rarely let their feet slip through the bars. (C) When suspended by its tail, a Tg(WT) mouse, like a nontransgenic mouse, splays its hind limbs apart. (D) In contrast, the Tg(PG14-A3) founder at 324 days of age tightly clasps its hind limbs together. (E) At 84 days of age, a Tg(PG14-A3)/Prn-p0/0 mouse suspended by its tail assumes a flexed posture, attempting to clasp all four limbs together.
Several features indicate that, in Tg(PG14) mice, degeneration of granule cells occurs by an apoptotic mechanism, these including the presence of numerous pyknotic and fragmented granule cell nuclei, positive staining of degenerating neurons, both by in situ end-labeling of DNA and by an antibody to activated caspase-3, and the presence in cerebellar DNA preparations of a 200-bp ladder indicative of internucleosomal cleavage. Tg(PG14) mice thus provide a particularly clear-cut demonstration of the role of apoptosis in a prion disease.
Figure 4. Neuropathological findings in the cerebella of Tg(PG14) mice. (A) Cerebellum of a healthy Tg(WT-E1)/Prn-p0/0 mouse at 184 days of age appears normal after staining with hematoxylin and eosin. (B) Cerebellar cortex of the same mouse shown in panel A, stained with antibody 3F4, shows no deposits of PrP, and normal appearance of the molecular (M), Purkinje cell (PC) and granule cell (G) layers. (C) Cerebellum of a terminally ill Tg(PG14-A3+/+)/Prn-p0/0 mouse at 183 days of age after staining with hematoxylin and eosin. There is marked atrophy of cerebellum, with reduction in the thickness of the granule cell and molecular layers. (D) Cerebellar cortex of the same mouse shown in panel C, stained with antibody 3F4. There is a dramatic reduction in the density of granule cells, and relatively weak staining for PrP. (E) Cerebellar cortex of the symptomatic Tg(PG14-A1) founder at 319 days of age, stained for GFAP. There is marked hypertrophy of Bergmann glial fibers in the molecular layer, and increased numbers of astrocytes in the granule cell layer. (F) Cerebellar cortex of a moderately symptomatic Tg(PG14-A3+/+)/Prn-p0/0 mouse at 71 days of age, stained with antibody 3F4. There is heavy PrP deposition in a synaptic-like pattern in the molecular layer, and less prominent staining in the granule cell layer. Purkinje cells are unstained, since the transgenic vector does not drive expression in this cell type. PrP staining is more intense in this mouse compared to the older animal shown in panel D, since the granule cell layer is more intact in this animal, and granule cells are an important source of PrP. Scale bars are 556 ^m (A and C), 97 ^m (B and D), 44 ^m (E), and 62 ^m (F).
A second abnormal feature in Tg(PG14) mice was the presence of punctate, “synaptic-like” deposits of PrP, which were most prominent in the cerebellum (Fig. 4F), hippocampal formation, and olfactory bulb, and were present to a lesser extent in the neocortex and inferior colliculus. A third finding was astro-cytic gliosis, which was observed in the cerebellar cortex (Fig. 4E), the hippocampus, and the neocortex. PrP deposition and gliosis began at 30-40 d of age in Tg(PG14+’+) mice, and increased as the illness progressed. Neither thioflavin-positive plaques, nor obvious spongiosis were observed at any time. No pathological changes were seen in Tg(WT) or non-transgenic mice. 5.3. PrPSc-Like Form of PrP in Tg(PG14) Mice PG14 PrP in the brains of Tg(PG14) mice displays the same biochemical hallmarks of PrPSc that we observed for mutant PrPs in CHO cells, including detergent insolubility (Fig. 5A), protease resistance (Fig. 5B-D), and resistance of the GPI anchor to cleavage by PIPLC (20,21). Detergent-insoluble and protease-resistant PG14 PrP is already synthesized in the brains of transgenic mice during the first week of life, well before the animals develop clinical symptoms or neuropatho-logical changes (20,21). Moreover, the amount of detergent-insoluble and pro-tease-resistant PrP increased dramatically with age, with levels in the oldest, terminally ill animals that were up to 80-fold higher than in newborn mice. PrPSc-like protein accumulated more rapidly and to higher levels in Tg(PG14+’+) mice than in Tg(PG14+/-) mice, which correlates with the accelerated disease progression in the homozygous animals. These results indicate that mutant PrP is converted continuously to the PrPSc state throughout life, but that clinical symptoms and neuropathological lesions do not ensue until the amount of PrPSc reaches a critical threshold level. If the same is true in human patients, this would explain why familial prion diseases do not manifest themselves clinically until adulthood, even though mutant PrP is probably synthesized beginning before birth (29).
To assess the neuroanatomical distribution of the PrPSc-like form of PG14 PrP, we carried out histoblots of cryostat sections of brain (30). Protease-resis-tant PrP was found throughout the brains of both preclinical and terminally ill Tg(PG14) mice, with particular concentrations in the medial caudate-putamen, septum, corpus callosum, anterior commissure, ventral thalamus, globus pallidus, and hippocampus (21). The widespread anatomical distribution of the PrPSc revealed by these methods contrasts with the more restricted distribution of punctate PrP deposits seen by immunohistochemistry (see above), raising the possibility that PrPSc may be more aggregated in certain regions, such as the cerebellum. Surprisingly, we have also found a detergent-insoluble and protease-resistant form of PG14 PrP in a number of the peripheral tissues in which PrP is normally expressed (although at lower levels than in brain), including skeletal muscle, heart, kidney, and testis (21).
Figure 5. PG14 PrP in the brains of transgenic mice is detergent-insoluble and pro-tease-resistant. (A) Detergent lysates of brain (containing 100 ^g of protein) from transgenic mice and from Syrian hamster were centrifuged at 260,000 X g for 40 min. Proteins in supernatants (S lanes) and pellets (P lanes) were then separated by SDS-PAGE and immunoblotted using antibody 3F4. One-fourth of each sample (lanes 1-16), or the whole sample (lanes 17-20) was run on the gel. (B-D) Detergent lysates of brain from transgenic mice and Syrian hamster were incubated with the indicated amounts of PK for 30 min at 37°C. Digestion was terminated by addition of PMSF, and metha-nol-precipitated proteins were separated by SDS-PAGE and immunoblotted using antibody 3F4. 200 ^g (B and C) or 800 ^g (D) of initial protein was subjected to digestion. The lanes containing undigested samples (0 ^g/ml PK) represent 50 ^g (B and C) or 200 ^g (D) of protein. Mice were of the following ages and clinical status at the time of sacrifice: E1-E4, 203 days old (all healthy); A1, 319 days old (severely symptomatic); A2, 71 days old (healthy); A3, 205 days old (mildly symptomatic); B, 169 days old (healthy); C, 226 days old (healthy).
Conclusions
We have analyzed two complementary experimental systems for expression of mutant PrP molecules carrying disease-associated mutations, one based on transfected cells in culture, and one based on transgenic mice. Both systems convert mutant PrP molecules to a PrPSc-like form, the biochemical properties of which are remarkably similar in the two systems, which suggests that structural features of the mutant PrPs themselves, perhaps in conjunction with ubiquitous cellular co-factors, are the primary determinants of the conversion reaction. It is noteworthy that the mutant PrPs from transgenic mice and CHO cells differ from authentic PrPSc in their considerably lower level of protease resistance (5,20), suggesting that they represent a biochemical intermediate along the pathway from PrPC to PrPSc. This intermediate has presumably acquired some of the biochemical features of PrPSc, but is structurally distinct, perhaps because it has only partial p-sheet character, or is less aggregated or polymerized. An important test will be to determine whether mutant PrPs from cells and Tg mice are infectious in animal bioassays, which is an experiment currently underway. Regardless of the results, however, the fact that the mutant proteins possess other PrPSc-like properties in addition to protease resistance, and the fact that they produce a neurological illness in vivo, make it likely that at least some aspects of PrPSc formation are being modeled in both CHO cells and Tg(PG14) mice. Thus, the insights gained from these systems significantly advance understanding of prion diseases on both a cell biological and patho-physiological level.
![PrPs carrying disease-related mutations are detergent-insoluble and protease-resistant when expressed in cultured CHO cells. (A) CHO cells expressing wild-type and mutant mouse PrPs were labeled with [35S]methionine for 20 minutes and then chased for 3 hours. Detergent lysates of the cells were centrifuged first at 16,000 g for 5 min, and then at 265,000g for 40 min. PrP in the supernatants and pellets from the second centrifugation was immunoprecipitated and analyzed by SDS-PAGE. PrP-specific bands were quantitated using a Phosphor-Imager, and the percentage of PrP in the pellet was calculated. Each bar represents the mean ±SD of values from three experiments. Values that are significantly different from wild type PrP by t-test (p < 0.001) are indicated by an asterisk. PrPs carrying disease-related mutations sediment (are detergent-insoluble), while wild type and M128V PrPs remain largely in the supernatant. Human homologues of the mutant PrPs analyzed here are associated with the following phenotypes: PG14 (9-octapeptide insertion), CJD-vari-ant; P101L, GSS; M128V, normal; D177N/Met128, FFI; D177N/Val128, CJD; F197S/ Val128, GSS; E199K, CJD. (B) CHO cells expressing each PrP were labeled for 3 h with [35S]methionine, and chased for 4 hours. Proteins in cell lysates were either digested at 37°C for 10 minutes with 3.3 ^g/ml of proteinase K (+ lanes), or were untreated (- lanes), prior to recovery of PrP by immunoprecipitation. Five times as many cell-equivalents were loaded in the + lanes as in the - lanes. Molecular weight markers are in kilodaltons. PrPs carrying disease-related mutations are detergent-insoluble and protease-resistant when expressed in cultured CHO cells. (A) CHO cells expressing wild-type and mutant mouse PrPs were labeled with [35S]methionine for 20 minutes and then chased for 3 hours. Detergent lysates of the cells were centrifuged first at 16,000 g for 5 min, and then at 265,000g for 40 min. PrP in the supernatants and pellets from the second centrifugation was immunoprecipitated and analyzed by SDS-PAGE. PrP-specific bands were quantitated using a Phosphor-Imager, and the percentage of PrP in the pellet was calculated. Each bar represents the mean ±SD of values from three experiments. Values that are significantly different from wild type PrP by t-test (p < 0.001) are indicated by an asterisk. PrPs carrying disease-related mutations sediment (are detergent-insoluble), while wild type and M128V PrPs remain largely in the supernatant. Human homologues of the mutant PrPs analyzed here are associated with the following phenotypes: PG14 (9-octapeptide insertion), CJD-vari-ant; P101L, GSS; M128V, normal; D177N/Met128, FFI; D177N/Val128, CJD; F197S/ Val128, GSS; E199K, CJD. (B) CHO cells expressing each PrP were labeled for 3 h with [35S]methionine, and chased for 4 hours. Proteins in cell lysates were either digested at 37°C for 10 minutes with 3.3 ^g/ml of proteinase K (+ lanes), or were untreated (- lanes), prior to recovery of PrP by immunoprecipitation. Five times as many cell-equivalents were loaded in the + lanes as in the - lanes. Molecular weight markers are in kilodaltons.](http://what-when-how.com/wp-content/uploads/2011/08/tmpD30_thumb.jpg)