Total disc arthroplasty
Overview
Lumbar fusion has been developed for several decades and became the standard surgical treatment for symptomatic lumbar degenerative disc disease (DDD). Disc arthroplasty devices have been designed in an attempt to replace functionally the intervertebral discs, as opposed to the gold standard method (fusion) which could not achieve that (Fekete et al, 2010). Hence, a method of motion preservation would be the best alternative to spinal arthrodesis, considering that it could theoretically prevent adjacent level degeneration. However, the long-term stability, endurance and strength of the prosthesis are unknown for the majority of implants (Freeman et al, 2006).
The most important functions of the intervertebral discs are the transmission of load and the maintenance of motion and disc height. Nevertheless, none of the implants currently available can reproduce totally the kinematics of a healthy intervertebral disc (Fekete et al, 2010).
There are basically two types of disc arthroplasty devices: nucleus or total disc replacement (TDR) devices, the latter being the most frequently used.
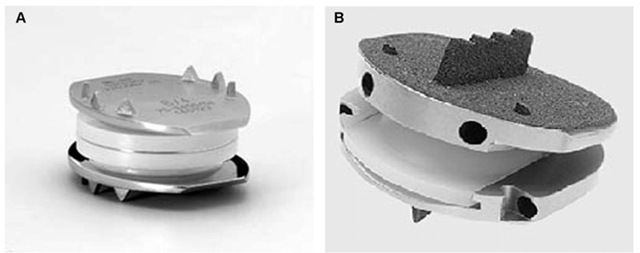
The first total disc arthroplasty implant to be widely used was the three component SB-Charite prothesis, a metal-polyethylene-metal construct, devised by Schellnack and Buttner-Janz in 1984. Since then, three different prototypes of the SB-Charite prosthesis have been developed. Of all the other types of total disc arhroplasty, the Pro-disc prosthesis, devised by Marnay, also in the 1980s, has been widely used (Zigler et al, 2004) (Figure 4).
Fig. 4. Total disc replacement in lumbar Spine: A) Sb-Charite, B) ProDisc prosthesis
Each artificial disc comprehends two or three components including two endplates and an articulating mechanism with either a metal-on-metal or metal-on-polymer surface. In order to keep the disc in place and providing stability within the host vertebral body, devices feature different designs, such as teeth-like components called spikes or fins that are driven into the vertebral bone, a porous coated surface on the endplates, promoting bony in-growth around these structures, or are secured into the recipient vertebral body with screws (Mayer et al, 2005, Jansen and Marchesi, 2008).
Arthroplasty devices can be classified based on their biomechanical properties, as (Errico et al, 2005):
1. Constrained implant: Have mechanical restrictions in motion within the physiological range, providing a fixed center of rotation.
2. Semi-constrained implant: allows motion in the physiological range
3. Non-constrained implant: allows hypermobility in comparison to the physiological range
The healthy tri-joint complex (intervertebral disc and the two facet joints) represents a semi-constrained system that allows physiological motion and prevents abnormal (excessive) motion. This motion unit in its healthy state allows for six potential motion directions: compression, distraction, flexion, extension, lateral bending, and axial rotation (McCullen et al, 2003).
Unlike spinal fusion, artificial disc replacement (ADR) is designed to preserve motion at the target spinal level. As well as possibly providing greater pain relief, this motion preservation may potentially decrease stress on and mobility of the adjacent segment structures, factors that are thought to contribute to adjacent segment disease. ADR can also restore pre-degenerative disc height and spinal
Alignment and the benefit of not depending upon a bone graft. Other theoretical advantages include maintenance of mechanical characteristics, decreased perioperative morbidity compared with fusion, and early return to function (Fritzell et al, 2001).
Indications
The leading indication for total disc arthroplasty is symptomatic, degenerative, monosegmental instability of the lumbar spine between L2 and S1. The patient must be refractory to all kinds of conservative treatment, having persistent pain (intensity greater than 5 on the visual analog scale) for at least six months. Age should range preferably between 30 and 50 years old. Furthermore, there must be a correlation between imaging studies and symptoms. MRI shows degeneration of the disc, with only mild loss of height of intervertebral space. Provocative discography reproduces the patient’s typical pain (Kraemer et al, 2009).
Contraindications to the implantation of disc prosthesis include: osteoporosis, infection, deformities, tumors, malformations, multisegmental degeneration and psychosocial disturbances (Kraemer et al, 2009).
Surgical method
Insertion of the prosthesis involves an anterior approach and is usually performed by a general surgeon and a spine surgeon. Potential problems associated with ADR may include injury to other structures (vascular, neurologic, intestinal, or urogenital), infection, loosening, polyethylene or metal wear, loss of motion over time, impact on adjacent discs and facet joints, subsidence, implant failure, heterotopic ossification, and device related endplate fracture (Geisler et al, 2004, 2008).
Clinical results
It is still uncertain, though, whether TDR is really more effective and safer than the gold standard treatment, lumbar fusion. To systematically compare the effectiveness and safety of TDR to that of arthrodesis treating lumbar DDD, Yajun and collaborators performed a meta-analysis, which has been published in 2010. The authors observed that the group of patients submitted to TDR had slightly better functioning and less back or leg pain without clinical significance, and significantly higher satisfaction status in TDR group compared with lumbar fusion group at the 2-year follow-up. Later on, at five years follow-up, these outcomes have not shown significant differences between comparing groups. The complication and reoperation rate of two groups are similar both at two and at five years.
The authors concluded that TDR does not show significant superiority for the treatment of lumbar DDD compared with fusion. The benefits of motion preservation and the long-term complications are still unable to be concluded. More high-quality RCTs with long-term follow-up are imperative to come to new conclusions.
In a systematic review of the literature, Freeman and coworkers (2006) stated that significant facet joint osteoarthritis is a contraindication to TDR, but that could be a difficult situation to identify in its early stages.
Moreover, the future of facet joints following a total disc replacement is obscure and facet joint hypertrophy, which accelerates spinal stenosis, may be a potent long-term complication that kind of implant. Not to mention that revision procedures will unquestionably be technically difficult with a great risk of vascular injury, particularly at the L4/5 level.
Therefore, that review of the literature concluded that the use of TDR may be limited to the treatment of degenerative disc disease in its early stages, with preservation of disc height. That would limit its indications, eliminating its uses in the majority of patients.
Up until now, only few studies have examined the direct effects of disc arthroplasty on adjacent levels. These studies show contradictory conclusions. While some of them support the idea of decreased adjacent-level degeneration, although lacking a clinical significance (Huang et al, 2006) others raise concerns about the high rates of index-level facet joint arthrosis and adjacent-level degeneration, despite motion preservation (van Ooij et al, 2003, Shim et al, 2007, Siepe et al, 2007) A trustworthy analysis of these results is difficult , considering the limitations in study design as well as the differences in the kinematics of the various implants examined.
Interspinous implants
Overview
With population aging, degenerative spine disorders became more common. The degenerative cascade, described by Kirkaldy-Willis and Farfan (1982) leads to disc and articular changes, with disc bulging and facet hypertrophy, causing effects in the spine, such as central and/or foramina! stenosis. Verbiest (1954) described neurogenic intermittent claudication secondary to degenerative lumbar stenosis. Thus, some kind of management has to be proposed, either conservative or surgical, in order to relieve symptoms. Weinstein (2008) suggests, in his study, that surgical procedures achieve better results, compared to conservative management.
Symptoms of spinal stenosis most often occur in patients 50 to 70 years old. These symptoms include low back pain, buttock pain, and/or trochanteric and posterior thight pain (Trautwein et al, 2010). Neurogenic claudication occurs when these symptoms exacerbs with walk, in extend position, and relieves when sitting or flexion of the spine.
A surgical treatment, for decompression and fusion of the segments, has increased operative time and blood loss, increasing complication rate in elderly patients (Carreon, et al, 2003, Deyo et al, 1993, Benz et al, 2001). To prevent complications and relief symptoms, with minimally intervention, new techniques have been developed to manage this condition.
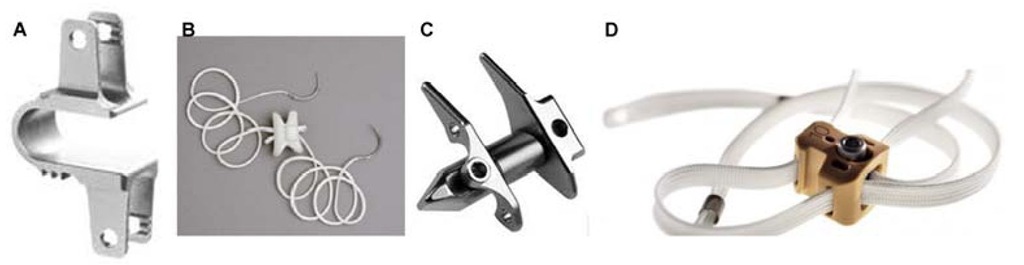
Interspinous devices were first described in 1950, by Dr Fred L Knowles (Bono et al, 2007). But, the results are poor, with high number of devices dislodged, needing to be removed. Senegas (1988) described an interspinous spacer, made of titanium, with Dacron tapes to fix the devices to spinous process. He had success in the treatment of more than 300 patients. After that, other implants have been developed (Coflex, Wallis, X-stop, Diam), with another material types (Titaniumm, peek) (Sengupta, 2004), but follow-up studies are still running to access its efficiency, and precise its indications (Figure 5).
Fig. 5. Interspinous distraction devices: A) Coflex, B) Diam, C) X-stop and D) Wallis.
Indications
The interspinous distraction devices, keep the segment in flexion. In this condition, the device reduces loading to the intervertebral disc, and also reduces spinal and foraminal stenosis (Sengupta et al, 2004). For this reason, this procedure is indicated in patients in whom the symptoms are increased in extension (Gunzburg et al, 2003). For better results, it is indicated for patients aged 50 years or older, with moderately impaired physical function related to neurogenic intermittent claudication, and may be implanted at one or two lumbar levels (Yi et al, 2010). Better results are related to pain relief in lumbar flexion, with or without low back pain, and failure of nonsurgical care (Laurysen et al, 2007). The Wallis mechanism to treat low back pain, caused by degenerative instability, is indicated for: Massive disc herniation, with substantial loss of disc material, reherniated disc with second discectomy, disc herniation in traditional level, like sacralization of L5, adjacent segment degeneration, to previous fusion, and isolated Modic I lesion, that leads to chronic low back pain. (Sengupta et al, 2004). Contraindications include: Disc degeneration grade V of Pfirrmann classification, spondilololisthesys, severe osteoporosis, spinal anatomy that would prevent implantation or cause instability, cauda equine syndrome and active systemic infection or localized infection at the site of implantation (Yi et al, 2010).
Surgical method
The X-stop device was developed to a minimally invasive approach, with short time surgery, to prevent complications in the elderly patients (Sengupta et al, 2004). For the procedure, patient must be placed in prone or lateral decubitus. They are positioned in flexed position, to keep distraction between the spinous process of the vertebral segment that will be treated. With a 4-5cm midline incision, the spinous processes are approached at the appropriate disc level, which is confirmed radiographically (Zucherman et al, 2004). The supraspinous ligament has to be maintained, to prevent kyphosis and stabilize the implant (Yi, et al, 2010, Zucherman et al, 2007). The distractor is placed through the interspinous ligament, after distraction, to maintain flexion of the segment. The spinal canal is not violated, with no need of laminectomy, laminotomy or foraminotomy.
The Wallis device must be placed with local or general anesthesia. Patient is placed in a prone position, in neutral. A neutral position of physiological lumbar lordosis is best to optimize the effect of the implant. All efforts should be made to avoid subsequent lumbar kyphosis (Senegas et al, 1988). The supraspinous ligament must be retained, to prevent kyphosis, and stabilize the segment. The procedure itself takes less than 15 minutes (Senegas et al, 2008).
Clinical results
Some studies have shown that surgical procedure, using X-stop device for chronic low back pain, substantially superior to conservative treatment, when is related to 1 or 2 level spinal stenosis, in cases where pain is relieved with flexion. These clinical results are based in a 2 years follow-up with claudication Questionnaire criteria (Zucherman, et al, 2004, 2005, Hsu et al, 2006, Anderson et al, 2006).
Comparing patients who received X-stop implants, with patients who underwent laminectomy without fusion (decompression surgery), Kondrashov et al (2007) have shown, in their study, an improvement of 15 points in the Oswestry Disability Index, defining patient success (78% of the X STOP group, versus only 33% of the laminectomy group, had successful outcomes at 4 years follow-up).
Biomechanical studies have shown beneficial effects of X-stop in kinematics of the spine (Kabir et al, 2010), with limitation in flexion/extension movement in the instrumentated level, increase in spinal canal and neural foramen, decrease in intradiscal pressure, decrease facet overload, no degenerative affection in adjacent levels, and no significant changes in biomechanics of the segment. Kutcha et al (2009) indicated, after Oswestry scores and Visual analogic scale evaluation, that X-stop implantation provides short and long term satisfactory clinical outcomes. However, some cases with severe stenosis and claudication have insatisfactory results with these implants.
Barbagallo and coworkers (2009) looked into the complications of X-STOP. Of a total of 69 patients, 8 had complications (1 interoperative and 7 postoperative). These included 4 device dislocations and 4 spinous process fractures, one of this peroperative, in a double-level implant. Of these, 7 patients (10.14%) required revision surgery. Korovessis and coworkers (2009), in a prospective controlled study, concluded that Wallis interspinous implant changed the natural history of adjacent disc degeneration incidence until up to 5 years after surgery. Senegas and coworkers (2009), in a 13 year follow up study with 107 patients, with canal stenosis or herniated disc, who underwent dymamic stabilization with Wallis, reported that the implants had to be removed in 20 patients, leading to fusion. The other 87 with Wallis had better clinical results in a retrospective evaluation, compared to fusion group. Floman and coworkers (2007), in a retrospective study with 37 patients who underwent primary lumbar disc excision and stabilization with Wallis, have shown 13% of recurrent herniations, suggesting that this implant does not reduce the incidente of recurrent herniations.
Trautwein and coworkers (2010), evaluated Coflex device (interspinous U shaped titanium alloy process), and concluded that fatigue failure of the spinal process and lamina is extremely rare. Kong and coworkers (2007), in a retrospective study, compared clinical results of patients who underwent lumbar decompression surgery, with Coflex placement, with patient who underwent posterior lumbar interbody fusion (PLIF). They assumed that Coflex leads to a lower stress in adjacent levels that PLIF.
Pedicular stabilization
Overview
To reduce pain and disability, spine surgical procedures have three main components: decompression, stabilization and correction of deformity (Schwarzenbach et al, 2005). For many years, spine fusion of the affected segments has been the gold standard procedure for this treatment. However, patients undergoing arthrodesis are subjected to a large number of short and long-term morbidities (Huang et al, 2005).
Considering the concepts of spinal instability, defined by Junghanns (1968), Kirkaldy-Willis and Farfan (1982), and White and Panjabi (1990), and the history of instrumentation in the spine, stabilization methods must diminish pathologic motion, prevent deformity, reduce deformity and compensate iatrogenic destabilization (Schwarzenbach et al, 2005).
Dynamic stabilization with pedicular screws has been developed, as an alternative to fusion, to achieve segmental stabilization, without complications seen in fusion (Di Silvestre et al, 2010).
Henry Graf (1992) first described the system of pedicular screws, surrounded by nonelastic polyester ligament with tension to lock the motion segment in extension. This concept was to lock the facet joints, stopping rotation (Sengupta et al, 2004). This system presented some problems, because the lordosis that the Graf produces results in stenosis of lateral recess, especially if there was any preexisting facet arthropathy or in-folding of the ligamentum flavum, and increases load in posterior annulus, which is a feature of painful degeneration of the disc (Grevitt et al, 1995).
In 1994, Dubois proposed the Dynesys system, a pedicular screw-based system, with flexible rods as a dynamic stabilization. Based on Kirkaldy-Willis concept of degeneration, Dynesys attempts to alter the first and second phases, reducing segmental motion to a physiologic level, neutralizing bendig, torsional, and shear forces, thus reducing load on disc (Schwarzenbach et al, 2005)(Figure 6).
Strempel and coworkers (2000) introduced a pedicular based stabilization system, with rigid rods and hinged head screws. With this architecture, a division of the load between implant and anterior column is achieved. Screws are made of titanium alloy and, since 2002, are covered by hydroxyapatite for better bone ingrowths (Figure 6).
Fig. 6. Pedicular stabilization devices: A) Dynesys – dynamic in the flexible rod, B) cosmic: Hinged head screws
Indications
In instability, dynamic devices are indicated in some conditions, based on their design and biomechanical effects (Schwarzenbach et al, 2005). The main goal of Dynesys is to stabilize the degenerated segments in early stages of degeneration, defined by Kirkaldi-Willis (1982). Ko and coworkers (2010) presented a study with patients who underwent dynamic stabilization with Dynesys. These patients had symptomatic low back pain, as result of degenerative spondylolisthesis, radiculopathy, or neurogenic claudication and they failed to respond to conservative treatment.
Strempel and coworkers (2000) said that cosmic system may possibly relieve pain as well as restorate the neurologic function without correction. Fusion is necessary when corrections (mostly in the sagittal plane) are necessary to treat pain. With limitation, this system won’t be used when there’s a need to treat more than three segments of the spine. Indications for cosmic are: Symptomatic lumbar stenosis, chronically recurring low back pain in the case of discogenic pain and facet syndrome, recurrent disc herniation, combination with a spondylodesis, and extension of an existing spondylodesis in the case of a painful adjacent level degeneration (the last 2 indications are hybrid constructions).
Di Silvestre (2010) consider to use dynamic stabilization system with Dynesys to treat lumbar degenerative scoliosis in the elderly, as an alternative to fusion methods, in order to decrease blood loss (there is no need to decortications of the facets and transverse processes), eliminate need of bone graft, and thus decreasing operative time.
Surgical method
Patients were treated under general anesthesia, in prone position (Di Silvestre et al, 2010, Ko et al. 2010, Maleci et al, 2011). Medial unique incision must be made, but Wiltse intermuscular plane approach is an option in stabilization procedures without wide decompression (Wiltse et al, 1988, von Strempel, 2000). In cases of stenosis, using Dynesys stabilization, and needing wide laminectomy, patients are positioned with hips flexed in 90 degrees and, after decompression, patients are repositioned to maximum lordosis (Di Silvestre et al 2010).
Pedicular screws are placed, by fluoroscopic control, in a lateral point entry, at the basis of transverse process with convergence angle between 13 and 18o in Dynesys (Di Silvestre et al, 2010), and between 20 and 25o in cosmic (Stremple et al, 2000) horizontal to the sagital plane. The screws must be as long as possible to prevent shear forces. Removing and reinserting of the screws must be avoided, to prevent screw loosening (Di Silvestre et al, 2010, Stremple et al, 2000).
After screw placement, distraction must be taken up to 4mm in cosmic system (Maleci et al, 2011), and 2mm in Dynesys system, to expand the neural foramina. In cosmic system, when decompression is necessary, a transverse stabilizer must be placed (Maleci et al, 2011).
Clinical results
Nonfusion techniques have been developed to prevent complications seen in spinal fusion, as adjacent segment disease (Cakir et al, 2009). Additionaly, fusion involves longer operative time and blood loss, increasing the complication rate, mainly in elderly (Di Silvestre et al, 2010). Not to mention the need of bone graft, with potencial effects on donor site (Huang et al, 2005).
Graf ligamentoplasty has been often unsatisfactory, not preventing postoperative instability, with high percentage of destatibilzation of the affected segment (Guigui et al, 1994). This system presented some problems, because the lordosis that the Graf produces results in stenosis of lateral recess, especially if there was any preexisting facet arthropathy or infolding of the ligamentum flavum, and increases load in posterior annulus, which is a feature of painful degeneration of the disc (Grevitt et al, 1995). Kanayama and coworkers (2005) showed poor clinical outcomes with Graf.
Di Silvestre (2010) evaluated clinical results after dynamic stabilization with Dynesys in elderly patients with lumbar degenerative scoliosis, with questionaries (oswestry disability index, Roland Morris, and visual analog scale), and radiologic imaging. In this study, clinical results have shown nonfusion stabilization as a safe procedure in elderly patients, with low complication rate, and statistically significant improvement in clinical outcomes.
Cakir and coworkers (2009), compared patients who underwent surgical treatment with decompression and Dynesys or decompression and fusion, having concluded that, in monosegmental instrumentation, no differences in adjacent level have been found, in a minimum follow-up of 24 months.
In 2006, Schanke and coworkers found signs of degeneration in disc adjacent to Dynesys stabilization in 29% of discs after 2 years. In the same follow-up period, the authors reported complications in 17% of patients, with 4 loosen screws and 1 broken screw out of 96 screws. This proportion was maintained in a continuous follow up, after 2 years, and no progression of instability has been shown (Schaeren et al, 2008). Screw loosening was assessed by Ko and coworkers (2010). Seventy one patients, who underwent decompression and stabilization with Dynesys were evaluated. Loosening of the screws occurred in 19,7% of patients, but this did not affect their clinical improvement. It is interesting to note that such findings had never occurred in the middle vertebras in intermediary level. It’s more likely to occur on marginal segments.
Treatment of the dysfunctional segmental motion was assessed by Cansever and coworkers (2011), using radiologic parameters in postoperative time, in one year follow-up. Their results suggest that decompression with dynamic stabilization were effective for radiologic stability over time.
A recent article described nonfusion method in lumbar spinal fractures (Kim et al, 2011). In a 4 year follow-up (2002 – 2006), their results suggests that this method is one of the most effective to manage thoracolumbar fractures, especially in younger people.
Clinical results published with cosmic system, shows improvement in quality of life after dynamic stabilization, with decrease in visual analog scale of pain (Rodrigues et al. 2010, Strempel et al, 2006, Stremple et al, 2008). As complications, screw loosening was found in 5,2% and 5,03% cases, and just 1 case of adjacent disc degeneration was related. Screw breakage occurred in a low rate, but not all of them were symptomatic.
Rodrigues and coworkers (2010), in a retrospective evaluation of patients submitted to a pedicular dynamic stabilization with cosmic, showed an improvement in quality of life of these patients during the 29,5 months follow-up period. The SF-36 score ranging from 33.15% preoperatively, to 75.99% in the postoperative, was statistically significant using the student t test (p <0,0001). Maleci and coworkers (2011), using cosmic system, in a 2 year follow up period, showed good results, with a low complication rate. In this article, they emphasized advantages, such as reduction is surgical trauma, avoidance complication in graft donor site, and preservation of intervertebral cartilage. No spontaneous fusion has been observed in the follow-up, but a fibrous rigidity has been present.
Conclusion
Nonfusion techniques are new, compared to fusion, as an option in the surgical treatment for low back pain. As new techniques, long-term prospective studies must be designed to achieve their effectiveness.
The effects of fusion are well known in a long term analisys, with a large number of complications. Adjacent disc degeneration, donor site pain, pseudoarthrosys and high blood loss are aspects that must be avoided with nonfusion technologies.
The right indication is the most important key to the success of the surgical treatment. Up to now, good results have been shown with nonfusion surgeries, and these technologies are improving, to avoid complications, and preserve the physiological motion of the spine.
Long-term Follow-up studies must be taken, to a better understanding of these procedures, and indications in a large scale. But, the results obtained up to now are encouraging and hopeful.