Radiofrequency in medial branch block for facet joint pain
The patient is placed in prone position on the radiolucent table. The anatomical landmarks of the spinal structures reflected on the skin are marked under fluoroscopic guidance including midline and facet joints and transverse processes. The skin is then sterilized in the standard fashion. Local anesthesia with 2% lidocaine was injected into the subcutaneous tissue but not extended. Then a 10-cm, 22-gauge cannula with a 5-mm exposed tip was introduced percutaneously under fluoroscopic guidance to the medial branch of the distal portion of the spinal posterior rami nerve. The tip depth and site were adjusted according to the sensation similar to the clinical presentation. The point is the most sensitive area of soreness, numbness, heaviness and distention using the techniques of twirling, rotating the tip around the lesions. Then stimulation at 5 Hz with 0.5 msec pulse duration was used to confirm the nerve position. The temperature of the electrode tip was then raised to 80°C for 90 seconds.
The nerve supply of the facet joint originates from two levels. One branch of the primary ramus arises from the nerve root at the same level as the joint and another branch from the level above. Therefore therapeutic injection of the facet joint should include the joint above the suspected level (Lynch and Taylor, 1986). For example, the facet joint between the L4 and L5 vertebral bodies is innervated by the medial branch nerves from the L3 and L4 nerve roots. In the lumbar region, the medial branch of the posterior ramus lies in a groove on the base of the superior articular facet, where it lies in direct contact with the base of the superior surface of transverse process, passing between the mammillary and accessory processes. The nerve actually passes under mammilloaccessory ligament, and this is the most reliable site for locating the nerve in lumbar spine. The L5-S1 facet joint is innervated by three nerves, L4, L5, and S1.
Radiofrequency for sacroiliac joint pain
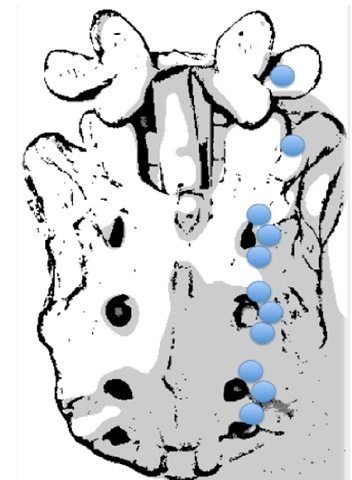
RF for sacroiliac joint (SIJ) pain is to lesion the possible afferent nerve from SIJs. All procedures can be done in an outpatient setting using local anesthesia. Inclusion criteria includes axial low back or buttock pain > 6 months in duration with tenderness overlying the SIJ(s); failure to respond to conservative therapy (e.g. physical therapy and pharmacotherapy), including long-term (>2 months) pain relief with SIJ corticosteroid injections; and > 75% pain relief as calculated from a 6-hour post-block pain diary following a single diagnostic SIJ injection (Cohen & Abdi 2003; Cohen et al., 2008). At each level, placement of the electrode in close proximity to the nerve was confirmed using electrostimulation at 50 Hz, with concordant sensation achieved at < 0.5 V. Prior to lesioning, the absence of leg contractions was verified with stimulation at 2 Hz up to 2 V. After satisfactory electrode placement, 0.5 ml of lidocaine 2% was injected through each cannula to reduce thermal pain and ensure blinding. The RF probe was then reinserted and a 90-second, 80° C lesion was made using a RF generator set to the lowest audible volume to blend in with ambient noise. For S1-3 lateral branch procedures, the RF needle targeting points illustrated on Fig. 6. To ensure that anesthetic spread to adjacent foramina did not impede sensory testing, electrodes were placed and stimulated at contiguous levels before denervation commenced. Once the needles were properly positioned, monopolar electrodes were sequentially inserted into the cannulae and 2.5-minute lesions were made using a water-cooled RF heating system (Pain Management SInergy System, Baylis Medical) and generator (PMG-115-TD, V2.0A, Baylis Medical). Using cooling-probe technology, the tissue temperature immediately adjacent to the cooled electrode was maintained at 60° C, while the target tissue was heated to 75° C, resulting in a lesion diameter ranging between 8 and 10 mm (Fig. 6). For safety reasons, this aggressive lesioning precludes using cooling probe technology for lumbar primary dorsal rami.
Fig. 6. The RF needle targeting points for sacroiliac joint pain
Evidence base medicine of radiofrequency application for low back pain
Intradiscal radiofrequency annuloplasty for discogenic low back pain
Among three major intradical RF annuloplasty procedures, IDET with spinecath was most commonly used and well-studied (Freeman et al., 2005; Pauza et al., 2004). Although the first results showed 50-70% efficacy, however, different opinions were noted in two randomized control trials and various positive and negative studies. In fact, no one will argue that the outcome is worse in severe degenerative disc disease and multi-segment degeneration. The evidence of transdiscal biacuplasty and disctrode is lacking. Both need prospective control trials to prove their efficacy.
Medial branches radiofrequency for low back pain from facet joints
Van Boxem et al. reviewed five recent randomized trials on the efficacy of RF facet denervation for chronic LBP. Three of them are positive, one is negative and one is equivocal (van Boxem et al., 2008). Among all the applications of RF and PRF, cervical facet and lumbar facet syndrome are most evidently effective. Although most of the symptom relief period is limited, these minimal invasive and safe procedures are worth using to treat selected patients with LBP from facet origins.
Radiofrequency for low back pain from sacroiliac joints
The diagnosis of SIJ-related LBP is difficult and there are still limited clinical studies supporting the efficacy of RF procedures in the treatment of SIJ pain. The treatment of SIJ intraarticular steroid injection is promising. Before a good prospective controlled study proves its efficacy, RF procedure applying to SIJ pain should be used as a second line procedure (Cohen 2005).
Radiofrequency for lumbar dorsal root ganglion in low back pain combined with or without lumbosacral radicular pain
Most prospective controlled trials for RF applying to DRGs are small or limited by inadequate study design or relative short term follow up (Malik & Benzon 2008). However, the best evidence trial of RF for DRG in treatment of LSR pain showed negative results (Geurts et al., 2003) Even if there are some retrospective studies with positive efficacy, a well-designed, randomized controlled trial is necessary.
Complication and management
The possible complications of RF denervation include bleeding, infection, nerve damage, broken electrodes and post-denervation neuritis. However, the complication rate is relatively lower than other more invasive procedures. And even though there are some case reports which mention permanent nerve damage (Abbott et al., 2007), the incidence decreases with the use of PRF, which is a less destructive procedure.
There are different considerations of IDET procedures even the complications are infrequent. One retrospective study review the complications of 1675 IDET procedures, six nerve injuries and six post-IDET disc herniation were reported. Other complications includes catheter breakage, temporary bladder dysfunction. Furthermore, the intradiscal heat may cause endplate injury and accelerate disc degeneration (Derby et al., 2008).
Conclusion
Chronic low back pain is a complicated situation that influences most members of the population at sometime during their lifetime. There are numerous of treatment modalities developed according to the diagnosis of different pathologies including non-invasive treatment and surgical intervention. Because chronic low back pain diagnosis is difficult, and the cause is multi-factorial, most treatment results for chronic LBP are unexpected. RF is a less invasive procedure that targets the pain transmission route. It can be applied reasonably to all pain problems. The evidence for the efficacy of RF for different kinds of etiologies causing chronic LBP is accumulating. Although there are some negative results and weak evidence of its efficacy, RF is still a treatment of choice because of low risk.