SOCIOECONOMIC DISPARITIES
Socioeconomic status (SES), which is a multidimensional construct of a complex set of factors, including education, income, employment, and other social indicators, is a strong predictor of behavioral risk factors for cancer, as well as a major determinant of insurance status and access to health care. No single indicator of SES fully captures all of the important characteristics that may influence the association between SES and cancer risk, but a consistent pattern emerges across studies of cancer disparity, in which lower SES is related to higher cancer incidence and mortality, regardless of which indicator is used (Aarts, Lemmens, Louwman, Kunst, & Coebergh, 2010; Cheng et al., 2009; Clegg et al., 2009; Marcella & Miller, 2001). These socioeconomic differences in cancer explain a substantial part of the cancer disparities between racial/ethnic groups. In addition, recent studies have shown that the association between SES and cancer is independent of race/ethnicity (Albano et al., 2007; Yin et al., 2010).
Incidence
People with lower SES are more likely to use tobacco, be physically inactive, follow an unhealthy diet, and consume alcohol excessively, partly due to less awareness of the risks of these unhealthy lifestyles, industries’ marketing strategies that target socioeconomically disadvantaged populations, and environmental or community factors that provide fewer places for physical activity and less access to fresh fruits and vegetables (American Cancer Society, 2010). For example, data from the NHIS showed that in 2008, the smoking prevalence among persons with less than a high school diploma (27.5%) was 2.6 times higher than that in college graduates (10.6%); and persons living in a family below the poverty line had a 60% higher smoking prevalence (31.5%) than those living at or above the poverty line (19.6%) (Centers for Disease Control and Prevention, 2009). In addition, lower SES appears to be associated with increased exposure to environmental toxins (Evans & Kantrowitz, 2002), as well as reduced adherence to cancer screening recommendations that would help identify precancerous lesions (Blackwell, Martinez, & Gentleman, 2008). As a result, persons with lower SES are more likely to develop cancer than those with higher SES. In an analysis of SEER National Longitudinal Mortality Study (SEER-NLMS) data (Clegg et al., 2009), apparent gradients in incidence rates by educational attainment, family income, and poverty status were observed for all cancers combined in males and for lung cancer in both genders. Lung cancer incidence rates for men and women with less than a high school education were three and two times that of their college-educated counterparts, respectively; and those with family annual incomes less than $12,500 were 1.7 times more likely to be diagnosed with lung cancer than those with annual incomes of $50,000 or higher (Table 2.5). Incidence rates for all cancers combined were 11% and 7% higher in high-poverty areas (census tracts) than in low-poverty areas, for non-Hispanic White and Black men, respectively, and substantial area socioeconomic gradients in incidence were also observed for some specific cancer sites (Singh, Miller, Hankey, & Edwards, 2003).
TABLE 2.5 Age-Adjusted Incidence Rates by Selected Socioeconomic Characteristics, 1973-2001 (SEER-NLMS data)
|
|
All Cancers Combined |
Lung Cancer |
||
|
|
Male |
Female |
Male |
Female |
|
Educational attainment (years of education) |
||||
|
Less than high school graduates (s11) |
730.3 |
478.5 |
166.6 |
71.6 |
|
High school graduates (12) |
694.7 |
475.3 |
123.9 |
59.1 |
|
Some post high school education |
658.0 |
481.4 |
93.6 |
56.4 |
|
(13-15) College education or beyond (16+) |
602.3 |
443.3 |
57.6 |
35.9 |
|
Family income (1990 dollars) |
||||
|
<$12,500 |
729.5 |
499.8 |
150.9 |
81.4 |
|
$12,500-$24,999 |
712.8 |
475.3 |
142.8 |
62.2 |
|
$25,000-$34,999 |
711.0 |
461.4 |
143.5 |
51.0 |
|
$35,000-$49,999 |
634.7 |
485.4 |
93.5 |
58.8 |
|
$50,000+ |
637.2 |
448.6 |
91.0 |
45.9 |
|
Poverty status (ratio of family income to poverty threshold) At or below 100% |
723.9 |
492.5 |
151.4 |
69.8 |
|
100-200% |
677.5 |
449.8 |
144.6 |
62.9 |
|
200-400% |
688.8 |
447.9 |
119.6 |
57.7 |
|
400-600% |
642.9 |
481.0 |
105.7 |
54.4 |
|
Above 600% |
653.0 |
459.6 |
90.3 |
47.7 |
SEER-NLMS, Surveillance, Epidemiology, and End Results—National Longitudinal Mortality Study. Source: From “Impact of socioeconomic status on cancer incidence and stage at diagnosis: Selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study" by L. X. Clegg, M. E. Reichman, B. A. Miller, B. F. Hankey, G. K. Singh, Y. D. Lin, et al., 2009, Cancer Causes and Control, 20, pp. 417-435. Used with permission.
Stage at Diagnosis and Survival
Both individual- and area-level data showed that the proportions of late-stage diagnoses were higher in patients with lower SES than in those with higher SES, for most common cancer sites, such as the lung, colon and rectum, female breast, cervix, and prostate (Clegg et al., 2009; Schwartz, Crossley-May, Vigneau, Brown, & Banerjee, 2003; Singh et al., 2003). For example, among colorectal cancer patients, the proportions of distant-stage diagnosis for men and women who live in more affluent census tracts are 19.0% and 18.5%, respectively. In contrast, for men and women who live in poorer census tracts, the respective percentages are 23.7% and 22.1%. For female breast cancer, 67% of patients in more affluent census tracts were diagnosed at localized stage; the percentage was 59.0% for patients in poorer census tracts. As a result, more deprived cancer patients have worse outcomes than their more affluent counterparts (Byers et al., 2008; Gordon, 2003). Among male cancer patients, the 5-year survival rate for all cancers combined was 49% in high-poverty areas, contrasting with 61% in low-poverty areas. Among women diagnosed with cancer, the 5-year survival rates for all cancers combined were 53% and 63% in high- and low-poverty areas, respectively.
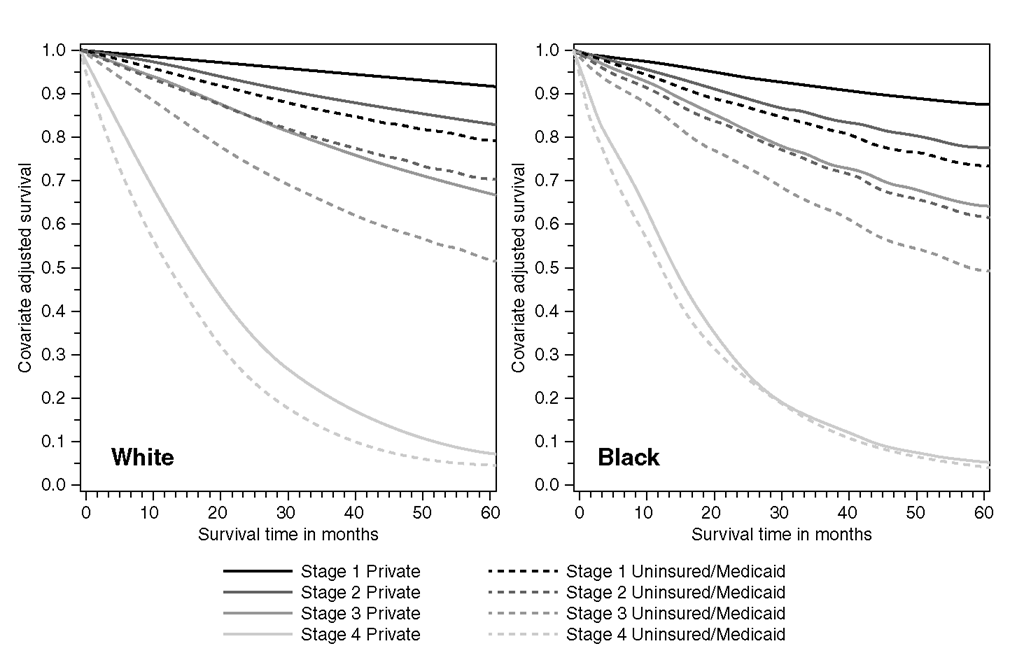
Disparities in stage at diagnosis and survival were also extensively reported by health insurance status, which is a major determinant of receipt of cancer screening and access to health care services, and is highly correlated with socioeconomic status. Analyses of the National Cancer Data Base (NCDB) revealed that individuals without insurance or with Medicaid insurance were more likely to be diagnosed with cancer in a later stage, or with a larger tumor size, than those with private insurance (Chen, Schrag, Halpern, Stewart, & Ward, 2007; Halpern, Bian, Ward, Schrag, & Chen, 2007; Halpern et al., 2008). Importantly, many cancer patients who are Medicaid-insured are uninsured at the time of diagnosis. For all cancers combined, patients without insurance or with Medicaid insurance were 1.6 times as likely to die in 5 years as those with private insurance (Ward et al., 2008). For both White and African American patients diagnosed with colorectal cancer in 1999-2000, privately insured patients with stage II disease had higher survival rates than patients with stage I disease who were Medicaid-insured or uninsured. Similarly, patients with stage III disease who were privately insured had survival rates similar to those for patients with stage II disease who were Medicaid-insured or uninsured (Figure 2.2) (Ward et al., 2008).
Mortality
Higher cancer mortality rates are consistently observed in populations of lower SES than in those with higher SES, because socioeconomically disadvantaged people are more likely to develop cancer, be diagnosed at a later stage, receive less optimal treatment, and have poorer survival.
FIGURE 2.2 Colorectal Cancer Survival by Stage and Insurance Status
This observation is consistent across studies regardless of whether individual- or area-level socioeconomic indicators are used. In an analysis of the U.S. mortality data for 2001, Albano et al. (2007) reported that educational attainment was strongly inversely associated with mortality from all cancers combined in both men and women aged 24-65 years, regardless of race. Among Black and White men, those with 12 or fewer years of education were more than twice as likely to die of cancer as those with more than 12 years of education. Cancer death rates among women with 12 or fewer years of education group were 1.8 (White) and 1.4 (Black) times those of their more educated counterparts. Elevated risks of death were also observed for the four most common cancer sites (lung, colorectal, breast, and prostate), among those with less education (Figure 2.3). Notably, disparities by educational attainment are generally larger than those by race. For example, Albano et al. also reported that for all cancers combined and for lung and colorectal cancers, the relative risks of death comparing less-educated (12 or fewer years of education) with highly educated (more than 12 years of education) individuals within each race group were larger than the relative risks of death comparing Blacks with Whites within each educational level, for both men and women (Albano et al., 2007). In addition to educational disparities, disproportionate cancer mortality rates are observed across area-based poverty levels. For example, the overall cancer mortality rate for men in high-poverty counties was 13% greater than that for men in low-poverty counties in 1999 (Singh et al., 2003).
FIGURE 2.3 Relative Risk of Death and 95% Confidence Interval From Cancer According to Education (<12 years vs. >12 years), United States, 2001