Introduction
Nicholas Andre recognized trigeminal neuralgia as a definite clinical entity in 1756 [1]. In 1773, John Fothergill described 14 cases of what he termed tic douloureux [2]. He noted that the pain in these patients was paroxysmal and sudden in its onset, the condition was more common in men than in women, and that it occurred more often in older people. His description of the symptoms is still used to make the diagnosis of trigeminal neuralgia. Despite various advances in neuroimaging and clinical electrophysiology, this remains a clinical diagnosis in which the patient’s history is the most important factor.
Characteristically, the patient with trigeminal neuralgia suffers from severe facial pain that occurs suddenly and is brief, at the most lasting a few minutes. The pain is very often described by the patient as knifelike, and may also be likened to an electrical shock. Some patients may develop an additional constant aching component upon which the knifelike pain is then superimposed. The pain is unilateral in more than 95% of cases, is confined to one or more of the distributions of the trigeminal nerve, and involves the lower face (second or third division) more frequently than the eye or the forehead. Bilateral trigeminal neuralgia may occur, but more often the patient will have symptoms first on one side of the face and then the other, rather than having simultaneous bilateral pain. The onset of pain may be set off by stimulation of a trigger point, or sometimes by the mere movement of, or any contact with, the skin over the face or mouth. The patient may experience symptom-free intervals between paroxysmal periods of pain. Women are affected more often than men and the disease is most commonly seen in patients older than age 50.
Treatment
A single, completely satisfactory method of treating trigeminal neuralgia in all patients has yet to be described. In all cases the initial therapy should be medical. Carbamazepine (Tegretol) and phenytoin (Dilantin) are the two drugs that have traditionally shown the greatest promise for patients with trigeminal neuralgia. Baclofen (Lioresal) may be useful in the treatment of patients whose pain has become refractory to treatment with carbamazepine or phenytoin [3]. Treatment with gabapentin (Neurontin) in recent years has become common in patients with trigeminal neuralgia, even though there are no large scale controlled studies of this drug’s efficacy in this disease [4]. When control of the patient’s symptoms is no longer possible with nontoxic levels of drugs, operative management should be considered.
The surgical treatment of patients with trigeminal neuralgia can be either nondestructive or destructive. The nondestructive procedure most frequently used is microvascular decompression of the trigeminal nerve root entry zone. The modern procedure, developed by Peter Jannetta, is based on observations made by Walter Dandy that in patients with trigeminal neuralgia, vascular compression of the trigeminal root at the pons is the etiology of the pain. By elevating the vessel off the nerve root entry zone, the procedure aims to produce pain relief without causing dysfunction of the tri-geminal nerve. Microvascular decompression is a very effective treatment giving long-term pain relief in more than 90% of patients who undergo the procedure. It may not be appropriate, however, for patients in poor health or in elderly patients who would not tolerate a craniotomy. It is also not appropriate in patients whose symptoms are caused by multiple sclerosis.
The goal of the destructive procedures is partial disruption of the sensory pathway to eliminate painful input. Peripheral neurectomy, retrogasser-ian neurotomy, and trigeminal tractotomy have, for the most part, been surpassed by the percutaneous procedures. These include retrogasserian glycerol rhizolysis, retrogasserian radiofrequency zhizotomy, and percutaneous compression of the gasserian ganglion. All three of these procedures can be performed percutaneously and meet the goal of modern surgical therapy, that is, long-term pain relief, minimal neurological deficit, and negligible morbidity.
Indications
A percutaneous ablative approach is indicated for patients with trigeminal neuralgia who no longer benefit from medical therapy or for whom the side effects of such medical therapy are no longer tolerable.
Glycerol rhizolysis or balloon compression may be indicated for patients with multidivisional pain. Selective radiofrequency rhizotomy may be indicated, especially in patients with isolated third division pain because it is possible to limit the nerve injury to the region of the jaw. Balloon compression, because it selectively injures large myelinated fibers, can be helpful for patients with first division pain.
The advantage of a percutaneous procedure over a craniectomy for microvascular decompression is that it is usually performed as an outpatient procedure. The risk of injury to the brain, other cranial nerves, or intracranial blood vessels is much less. The total hospital cost is less. Balloon compression and glycerol rhizolysis require less of an investment in equipment than radiofrequency rhizotomy. Balloon compression does not require the patient to be awake, whereas radiofrequency rhizotomy, and to some extent, glycerol rhizolysis, do require cooperation. Elderly patients in discomfort and under some sedation may find it difficult to provide such cooperation, and thus may be better candidates for balloon compression.
Preoperative Studies
Imaging studies performed before any of the percutaneous procedures should include a magnetic resonance imaging (MRI) (with and without contrast) of the brain and skull base to exclude a skull base tumor, and a submentovertex view of the skull, to ascertain any anomalous anatomy and the relative size of the foramen ovale. Serum clotting studies (prothrombin time, partial thromboplastin time, International Normalizing Ratio (INR), and platelet count) should be performed preoperatively, as abnormalities of clotting are contraindications to the percutaneous procedures.
Procedures
Approach: General Technique
Local infiltration anesthesia combined with intravenous (I.V.) sedation should be adequate for all of the percutaneous techniques. In the past, short-acting barbiturates, such as Brevitol, have been recommended. Diprivan administered as a continuous infusion may also be reliable in obtaining a controlled and adequate sedation. Supplemental O2 is administered by nasal cannula. Cardiovascular monitoring with I.V. access is essential as significant increase in blood pressure and bradycardia are often seen with stimulation of the trigeminal root fibers.
Intraoperative fluoroscopy (lateral) is required for localizing the tip of the rhizolysis needle. Biplane fluoroscopy [anterior-posterior (AP)/lateral] with a submentovertex projection allows the surgeon to both direct the needle toward the foramen ovale and gauge its course without repositioning the patient or the unit.
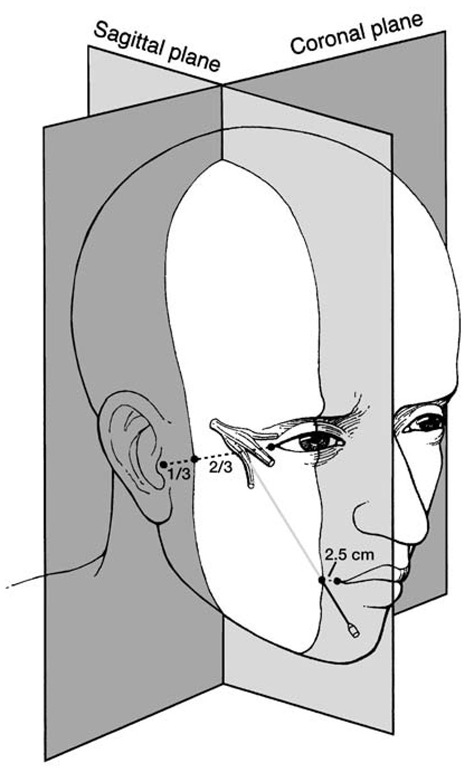
Ablative percutaneous procedures directed at the retrogasserian fibers share a common approach. This approach has been previously described by Hartel [5]. The usual site of needle insertion is approximately 2.5 cm lateral to the corner of the mouth on the symptomatic side. The entry site is more lateral and inferior for first division pain and more medial for third division lesions. Two additional landmarks are marked on the skin before starting the procedure. The first of the additional landmarks is a point directly beneath the midpoint of the ipsilateral pupil with the eyes looking straight ahead; the second is a point one third of the distance along the line drawn from the external auditory canal to the lateral canthus of the eye (Fig. 1). The intersection of the parasagittal and coronal planes drawn through these points is the approximate location of the foramen ovale and is the target of the needle tip (Fig. 2). The needle or cannula is directed to a point on a plane with the zygomatic arch, 2.5 cm anterior to the external auditory canal, and with the medial aspect of the pupil. Fluoroscopic guidance is always used when penetrating the foramen ovale. When the neurosurgeon is using the lateral view, the needle is directed just inferior to the lateral pterygoid wing. The surgeon should place a finger in the mouth to assure that the oral mucosa is not punctured. On the lateral radiograph the needle is seen to be directed toward the radiographic intersection of clivus and petrous bone. It is possible to puncture the internal carotid artery with this approach, as the artery is only protected by thinned bone at the skull base.
Once the foramen is entered, an anterior-posterior image can be obtained. With this image, the petrous bone is positioned in the radiographic center of the orbit. The trigeminal nerve forms a groove in the petrous bone as it enters Meckel’s cave. The radiofrequency electrode, balloon catheter, or spinal needle must be directed toward this groove to create a lesion in the retrogasserian fibers. When seen on a lateral view, the needle is directed at the radiographic intersection of the clivus and petrous bone.
Figure 1 Surface landmarks for penetration of the foramen ovale: needle of entry 2.5 cm lateral to the mouth, directed to the intersection of midpupillary line and a point one third of the distance from the tragus to the lateral canthus.
Retrogasserian Glycerol Rhizolysis
Results from the first series of patients treated by glycerol rhizolysis were published by Hakanson in 1981 [6]. Previously, glycerol was used in mixtures containing ethanol or phenol for the rhizotomy procedure. The observation that glycerol alone was effective for the treatment of trigeminal neuralgia eliminated the need for other substances in the procedure. Glycerol is a demyelinating agent that reduces sensory input to the trigeminal system [7].
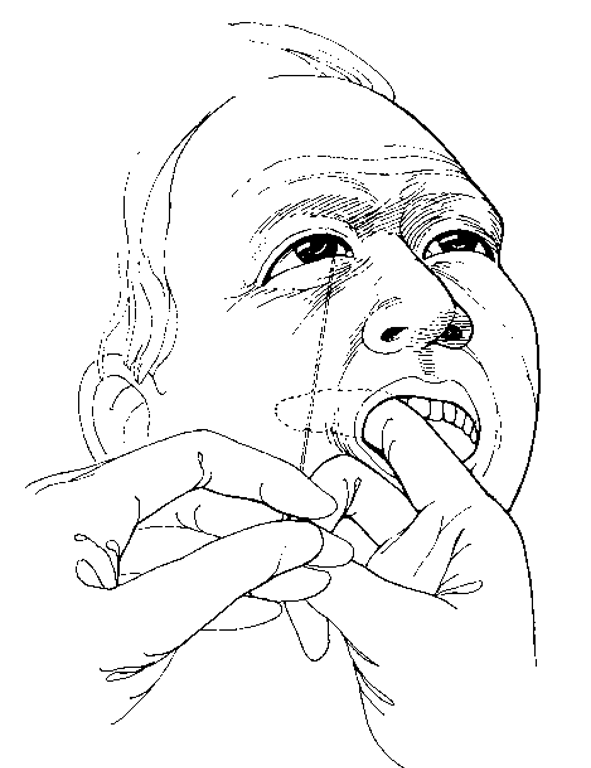
Figure 2 Point of needle in the foramen ovale. A gloved finger prevents penetration of the oral mucosa.
It may be easier to perform glycerol rhizotomy with the patient positioned on the transport stretcher rather than the operating room table (thereby decreasing the risk of displacing the glycerol during transfer of the patient from the table to the stretcher). Before starting the procedure, as a matter of patient comfort, the patient’s buttocks should be aligned with the fold in the table (as the patient will be in a sitting position for approximately 4 hours after injection).
An 18-gauge/4-inch Quincke needle with a 22-degree bevel and trocar (Popper and Sona, New Hyde Park, NY) is used after noting the above landmarks. After prepping the skin with an antiseptic solution, with the patient in the supine position, the entry point is anesthetized and the rhizotomy needle is used to puncture the skin of the cheek. The index finger of the surgeon’s gloved hand is placed in the patient’s mouth to guide the needle through the soft tissues of the cheek, taking care not to puncture the oral mucosa.
As the needle tip punctures the foramen, a slight contraction of the masseter muscle is often felt as a gentle bite on the surgeon’s gloved finger. Intravenous sedation is given for this step. As the trocar is removed from the needle, cerebrospinal fluid may drip from its lumen, but this finding is not essential for correct placement and may occur even if the needle is lateral to the intended target. Indeed if glycerol has been previously injected, cerebrospinal fluid may not flow from the trigeminal cistern at all.
The foramen ovale is entered while the patient is positioned supine. The location of the needle tip in the foramen ovale may be confirmed by instilling a small bolus of nonionic radiopaque contrast slowly under continuous fluoroscopy, with the patient in the semisitting position (Fig. 3). The volume of the contrast that can be instilled before overflow can be used as a rough estimate of the volume of Meckel’s cave. The average volume is 0.24 ml (0.1-0.5 ml). An X-ray is taken at this time for inclusion in the patient’s record. With the needle in place, the patient is moved from semi-sitting to supine position then back to the operative position (to spill the contrast out of Meckel’s cave). At this point if glycerol rhizolysis is the intended technique, the patient should be placed in as close to a 90-degree sitting position as possible; he or she may be moved to a stretcher if need be, so that head movement after injection is minimized. A small volume (0.25-0.75 cc) of sterile anhydrous glycerol is injected slowly and the needle subsequently withdrawn.
With injection of the glycerol, many patients have marked blood pressure elevation. Tearing of the ipsilateral eye and a flushing of the skin of the cheek may also be seen. Depending on the level of sedation, patients may complain of pain during and immediately after the injection. They should be reassured that this is normal. After the needle is withdrawn, the patient is transported to the recovery room in a sitting position where he or she remains for 2 to 4 hours. To minimize movement and reduce the risk of displacing the glycerol, the patient’s head may be taped to the stretcher with a pillow folded in half behind it.
Selective lesioning of the trigeminal branches may be obtained by positioning the patient’s head. When the head is in a neutral position (chin on the horizon), a lesion of the second and third division of the trigeminal nerve can be produced. With the head slightly flexed (chin below the horizon), first division lesions can be produced. Partial filling of the trigeminal cistern can also cause selective damage. For third division pain, half the cistern is filled. For second and third division pain, two thirds is filled.
Figure 3 Lateral fluoroscopic projection: needle in the trigeminal cistern.
Glycerol may be "floated" on top of iodine contrast for selective injury of the first division.
Glycerol rhizolysis will produce pain relief in a high percentage of patients within hours of injection. Diminished sensation in the involved root distribution is not essential for relief of pain, but its presence often correlates with a longer duration of the pain-free period. A few patients may not experience relief after glycerol rhizolysis. For these patients who do not respond within 7 to 10 days, the procedure may be repeated or other techniques may be used.
Jho and Lundsford reported 90% early pain relief with 55% of patients pain free without need for medication [8]. Other reports indicate a 30% to 50% recurrence rate over 2 to 10 years. Moderate to severe sensory deficit has been reported in 19% of patients, more often in patients who underwent multiple procedures. It is a matter of concern that it is difficult to predict the degree of sensory loss for each patient [9].
Selective Radiofrequency Rhizotomy
Radiofrequency trigeminal rhizotomy depends on a differential vulnerability of pain and touch fibers to thermocoagulation. The A-delta and C fibers that relay pain are more susceptible to injury than the A-alpha and beta fibers that carry touch sensation. There are two electrode types. Either a thin cordotomy-type electrode or a larger, curved electrode with temperature monitoring capabilities are available [10,11]. Thermistor controlled radio-frequency lesion generators are available from several sources (Radionics, Burlington, MA). Lesions are made sequentially with a temperature-monitoring electrode at 60 degrees to 90 degrees. The temperature is increased by 5-degree intervals, and the patient is re-examined after each lesion. When using a cordotomy-type electrode, the lesion is made at 10 V and 60 mA for 20 seconds, increasing gradually toward a maximum of 18 to 20 V and 90 to 100 mA [12].
The technique of needle placement is essentially the same as for glyc-erol rhizolysis but upon entering the foramen, sedation is stopped, as it is necessary for the patient to be awake for the prelesioning testing. The first-division fibers are located superomedially, as seen on both the lateral and AP views. Third division fibers are located in the lateral portion of the entrance to Meckel’s cave on the AP view, with the electrode just short of the edge of the petrous bone. On the lateral view, the electrode should be seen lying parallel to the petrous bone. It may be necessary to reposition the needle entry site to redirect the electrode tip appropriately. Third-division fibers are reached by redirecting the electrode curve inferiorly, with its tip lying 5 mm proximal to the clival line [13].
An insulated electrode is passed through the needle, and stimulation at approximately 50 Hz is used when adjusting the position of the electrode. Optimum position of the electrode is ascertained when a nonpainful pares-thesia is produced in the distribution of the intended trigeminal division at a low threshold (0.2-0.3 volts). If masseter muscle contraction is observed at less than 0.5 volts, the electrode is too close to the motor root and the needle should be repositioned laterally. An initial radiofrequency lesion can be made at 60 mA for 10 seconds, followed by a 20-second and then a 30-second lesion. It is important to test the patient in between each of the lesions.
If insufficient sensory loss is determined, the current can be increased by 10 to 70 mA and a series of three lesions made again. This can be repeated to a maximum of 110 mA. If a lesion cannot be produced by a maximum of 110 mA for 30 seconds, the needle is not in the appropriate position, and the procedure should be either terminated or the needle repo-sitioned. The endpoint of lesion production is deep hypalgesia in the division or divisions of the trigeminal nerve where the pain arises. The patient should experience the prick of a safety pin as touch but not as pinprick.
Retrogasserian Balloon Compression
Balloon compression of the trigeminal ganglion was described by Mullan and Lichter in 1983 [14]. Balloon compression is performed under general anesthesia and does not require patient cooperation, yet it can selectively treat pain limited to specific divisions [14-17]. Compression is especially helpful in first-division pain because the unmyelinated fibers that mediate the blink reflex are preserved by the mechanical injury generated by the balloon. Compression is also helpful for multidivisional pain. It is relatively inexpensive, with disposable units costing less than $500.
The balloon catheter is introduced through a #14-gauge blunt cannula that is directed to the foramen ovale. Straight or curved guiding stylets (Cook, Inc., Bloomington, IN) are positioned within the entrance to Meckel’s cave 18 mm beyond the foramen ovale. Anterior-posterior and lateral fluo-roscopic views provide guidance. The catheter is then directed to the site where the trigeminal nerve traverses the edge of the petrous bone through a small elliptical opening in the dura. The balloon is inflated for 1 minute to a pressure of 1.3 to 1.6 atmospheres, as measured by an insufflation syringe with an attached transducer (Merit Medical, Inc., Salt Lake City, UT). Alternatively, approximately 0.5 to 0.7 ml of radiopaque contrast is placed through the needle and the balloon distended.
When properly positioned, the tip of the balloon compresses the retro-gasserian trigeminal nerve against the petrous bone and the firm medial edge of the dura. Radiographically, the balloon will have a "pear” shape caused by its position at the Meckel’s cave entrance. The balloon is allowed to remain full for approximately 1 minute and subsequently, the balloon is deflated and the entire needle catheter assembly removed as a unit to avoid shearing off the tip of the catheter. During inflation, a significant trigeminal reflex response causes bradycardia. This indicates appropriate compression. If this is a concern, especially in the more elderly or medically unstable patient, the patient may be fitted with an external pacemaker set to trigger should the heart rate drop below 40 beats/minute.
By adjusting the angle at which the balloon catheter is inserted and the position of the catheter tip in the "porus trigeminus,” the entrance to Meckel’s cave, selective divisional injury can be obtained. By using a curved stylet to direct the catheter tip toward the medial portion of the porus, the first division is favored. Directing the catheter toward the lateral porus and angling the cannula so that it lies parallel to the petrous ridge favors third-division fibers.
Balloon compression has a higher incidence of masseter and pterygoid muscle weakness than other percutaneous techniques. This weakness usually resolves, but patients may experience temporomandibular joint discomfort until it does. This discomfort may be treated with anti-inflammatory medication. The recurrence rate for balloon compression is comparable to that in other percutaneous techniques, and the procedure can be repeated for recurrence without greater technical difficulty.
Complications and Recurrence
Complications seen from percutaneous ablative therapy for trigeminal neuralgia have been extensively documented. The oral mucosa may be penetrated during the approach, resulting in bacterial meningitis or brain abscess. A carotid-cavernous fistula may result from injury to the internal carotid artery. There is a possibility of otalgia from eustacian tube dysfunction, or temporomandibular joint tenderness along with jaw weakness. Aseptic meningitis has been reported, as well as intracranial hemorrhage from acute hypertension. Other reported complications are bradycardia with subsequent hypotension, neurokeratitis, temporary diplopia, optic nerve injury, subdural hematoma, postoperative herpes simplex activation, bothersome facial sensory loss and dysesthesias, and anesthesia dolorosa [18,19]. These potential morbidities need to be discussed with patients as part of the preoperative meeting even though the risk of their occurrence is 2% or less.
As long as the surgical endpoint selected is mild to moderate hypes-thesia, there will be a recurrence rate of 20% to 25%, depending on the time elapsed after surgery, with recurrence rates being twice as high for trigeminal neuralgia associated with multiple sclerosis. Recurrent pain occurs either because of regeneration of injured myelin or from progression of the disease to include untreated trigeminal sensory divisions.
Each of these ablative procedures can be safely repeated for recurrence, as long as the goal remains the creation of mild to moderate hypesthesia. There is no evidence to suggest that patients who have undergone a percutaneous ablative procedure are at any disadvantage should they later undergo microvascular decompression for recurrence. However, the success rate for treatment by a repeat procedure is lower than that for a primary procedure and the recurrence rate is higher.
DISCUSSION
Glycerol rhizolysis, radiofrequency rhizotomy, and balloon compression of the trigeminal ganglia are all effective, simple, and attractive techniques for treating trigeminal neuralgia in patients for whom medical therapy has become ineffective or drug-related toxicity has occurred; patients in whom a craniotomy and microvascular decompression is contraindicated because of age or poor health; patients who have been previously treated with micro-vascular decompression and have now experienced recurrence of pain; and a select group of patients with trigeminal neuralgia secondary to multiple sclerosis or nerve injury distal to the dorsal root ganglion. All of the procedures share the risk of complications related to needle placement. As a general rule, however, the incidence of complications is low. Satisfactory relief of pain should be obtained in more than 90% of patients for periods extending from 6 months to several years with these techniques. In cases in which pain relief is not satisfactory with a single procedure, a second attempt at that procedure or a different technique may be performed. It is important to remember that most patients can gain relief at the hands of a persistent surgeon.