History
Division of the corpus callosum for the treatment of patients with seizure disorders dates back to the observations of Van Wagenen in the 1930s [1]. He noticed that patients with strokes affecting the corpus callosum often had improvement in the frequency of their attacks. Experimental evidence for the importance of commissural fibers for the spread of epilepsy was demonstrated in the primate by Erickson, lending further support for this therapeutic approach [2]. Additional reports by Bogan in adults [3] and Lues-senhop in children [4] established corpus callosotomy (CC) as a standard technique in the surgical treatment of epilepsy.
Indications
Adults
Candidates for CC include patients with medically intractable primary generalized epilepsy or partial epilepsy with rapid secondary generalization that is either unlocalized or localized to unresectable cortex. Differentiation between these two groups is often difficult, although relevant, in that patients with lateralized electroencephalograph^ findings often have a better outcome [5,6]. The most common generalized epilepsies treated with CC are characterized by atonic or akinetic seizures, often involving sudden drop attacks. Patients with predominantly tonic or tonic-clonic seizures also respond to CC and, in fact, most patients considered for CC have multiple seizure types.
Children
In the pediatric age group, one must balance the potential disruption of cortical reorganization mediated by the intact corpus callosum with the potential excitotoxic injury of persistent frequent seizures in the developing brain [7]. The consensus is that early surgery is indicated, depending on the severity of the seizures [7]. Indications in this age group are similar to the adult, although there is a higher proportion of patients with hemispheric disease, such as infantile hemiplegia, forme-fruste infantile hemiplegia, and Rasmussen’s syndrome. Although CC can be used as a substitute for hem-ispherectomy, if the source of the seizures can be localized and hemispher-ectomy can be performed, this is preferable. Corpus callosotomy to treat hemispheric disease should be reserved for children with residual neurological function in the damaged hemisphere and in whom hemispherectomy is contraindicated. Children with Lennox-Gastaut show a significant improvement in seizure control and quality of life [8,9].
Contraindications
Patients in whom a resectable focus can be identified are clearly not candidates for CC. Surgical cure after successful resective surgery is much higher than for CC. Bilateral synchronous epileptiform abnormalities do not necessarily imply a worse outcome; however, the discovery of bilateral independent foci should raise concern. Age, mixed hemisphere dominance, and mental retardation have also been considered contraindications in some series; however, many surgeons do not automatically exclude such patients, although successful outcome is less likely [10]. One third of children with severe mental retardation may benefit from CC, particularly if focal or hemispheric damage is documented [7]. Patients with multifocal, bifrontal asymmetric epilepsy may be at higher risk of developing more intense seizure foci postoperatively.
Technique
Complete section is approximately twice as effective as partial section in controlling seizure frequency [6,10]. Nevertheless, most centers currently perform a partial section initially to avoid a potential acute disconnection syndrome, although even partial CC may disrupt cortical function, particularly in patients with mixed dominance (see below). Completion of CC is then performed as a second operation if seizure control is inadequate. Initial posterior CC has been described; however, anterior section with sparing of the anterior commissure and fornix is the preferred first operation unless clearly posterior epileptogenic abnormalities are documented. Preoperative evaluation for coagulopathy, including a bleeding time, is essential, as patients are generally on multiple anticonvulsants.
Anterior 2/3 Callosotomy
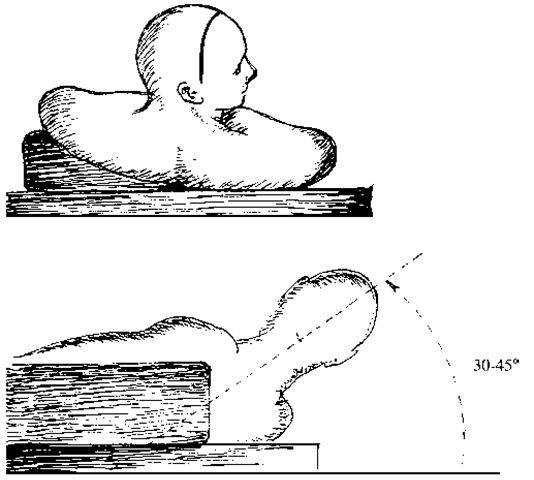
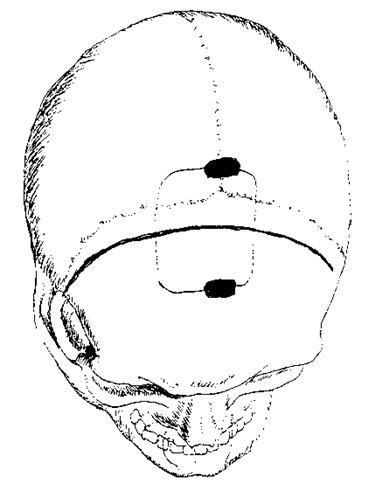
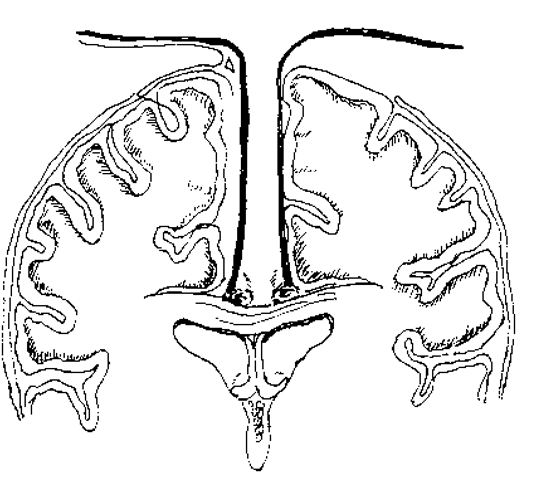
The surgery is performed under general anesthesia. Electroencephalogram is not necessary, but if used, requires appropriate anesthetic agents that do not interfere with the recording. Mannitol, decadron, and prophylactic antibiotics are administered intravenously. The patient is placed supine on the table with the head turned toward the nondominant hemisphere, a shoulder roll under the contralateral shoulder and the vertex elevated by 30 to 45 degrees (Fig. 1). This position permits a minimum of retraction, as the dependent hemisphere is retracted by gravity and the operating microscope retains stereoscopic vision in the horizontal plane. A partial bicoronal incision is made 2 cm in front of the coronal suture, of sufficient length to permit the cra-niotomy, which extends 4 cm in front of, and 2 cm behind, the coronal suture and from 1 cm over the sagittal suture to the temporal insertion of the dependent side of the cranium (Fig. 2). Reviewing the angiogram from the Wada test or obtaining a Magnetic Resonance Venogram (MRV) may be helpful in surgical planning but it is usually possible to work around any draining veins. The dura is reflected over the sinus and the interhemispheric dissection is performed using loupes or the surgical microscope (Fig. 3). If gravity alone does not supply sufficient retraction, additional force can be attained either with two rolled up cotton paddies or gentle pressure from a self-retaining retractor. The glistening white corpus callosum is identified and exposed along its length, as are the two pericallosal arteries. Division of the corpus callosum is best performed under the operating microscope by dividing a small portion of the callosum and identifying the midline cleft between the ventricles where the septum pellucidum inserts. The use of frameless stereotaxy can be helpful in distinguishing the callosum from the cingulate gyri and defining the depth of the callosum, depending on the degree of brain shift. Without entering the ventricle, this cleft is followed first anteriorly around the genu and down to the rostrum. Additional posterior division can be performed with the help of frameless stereotaxy to achieve a 2/3 division. Alternatively, a metal clip can be placed at the back of the callosal division and a lateral radiograph obtained to ensure that the callo-sotomy has been carried out behind the line bisecting the glabella-inion line. A final metal clip is then placed at the posterior margin of the callosotomy to demarcate the limits of the resection in case a second operation is required to complete the callosotomy. Anticonvulsants are continued postoperatively.
Figure 1 The patient is placed supine and the head is elevated to 30 to 45 degrees. The head is turned to the right so that gravity can help retract the nondominant hemisphere and the microscope can maintain stereoscopic vision.
Posterior 1/3 Callosotomy
At least 3 months after the first procedure, decision is made regarding completion of the callosotomy. The patient is placed in a similar position with slightly more head flexion. A partial bicoronal skin incision is placed over the parietal eminence, sufficient to expose the craniotomy. The bone flap extends from 1 cm behind the lambdoid suture to 4 cm in front and from 1 cm over the sagittal suture to 4 cm lateral in the direction of the nondominant hemisphere. Division of the posterior callosum is performed down to the arachnoid to preserve the arachnoid overlying the pineal and quadrigem-inal cisterns. The posterior hippocampal commissure is divided with the callosum.
Figure 2 A partial bicoronal skin incision is performed and the temporalis muscle is not violated. A burr is used to drill slots over the sinus and a craniotomy is elevated 2/3 in front and 1/3 behind the coronal suture, extending just over the midline.
Postoperative MRI
All patients should undergo postoperative magnetic resonance imaging (MRI), and sagittal images must be reviewed to assess the extent of the callosal section.
Results
Seizure Frequency and Intensity
The best results occur in patients with nonlocalizable but focal hemispheric disease [7]. Seizure onset before age 5 has been associated with a better outcome, and mental retardation with a worse outcome [6,9]. For all patients, secondarily generalized seizures are controlled in 70% to 80% of patients, whereas only 25% to 50% of patients find relief from complex-partial seizures.
Figure 3 Interhemispheric dissection exposes the corpus callosum between the pericallosal arteries.
Corpus callosotomy is not intended as a curative procedure, but reports of complete cessation of seizures can occur in 5% to 7% of patients [11]. In one series, greater than 80% reduction in seizure frequency was found for major seizures in 65% of patients, focal motor seizures 38%, atonic seizures in 76%, and absence in 68% [10]. For all seizures together, the percentage of patients obtaining better than 80% reduction in generalized seizures improves from 29% after anterior section to 62% after completion of callosal section [10]. Up to 30% of patients may develop more intense or newly patterned seizures postoperatively from removal of callosally mediated inhibitory interhemispheric connections, particularly in patients with bilateral independent frontal foci [12]. On the other hand, development of a lateralized focus may also occur after CC, which may be amenable to cure after further resective surgery [13,14].
Neuropsychology
Patients with early onset central nervous system (CNS) disease and signs of severe lateralized CNS dysfunction, including a structural lesion, impaired memory, neurological deficit, and contralateral speech function tend to have a good neuropsychological outcome [15]. In such patients, the preserved functions are subserved almost entirely by the intact hemisphere. In patients with mild to moderate CNS dysfunction, surgery can disrupt callosally mediated interhemispheric compensatory mechanisms causing a decrease in manual dexterity postoperatively [15]. If the speech-dominant hemisphere is contralateral to the hemisphere controlling the dominant hand, which can occur in a late-onset, left hemisphere seizure disorder, postoperative speech deterioration can occur [15]. Other forms of mixed dominance, such as memory function contralateral to speech or hemianopsia contralateral to language, may result in postoperative mutism or alexia without agraphia respectively [16]. Isolated posterior callosal section can produce a syndrome of sensory disconnection with the language-dominant hemisphere not having access to stimuli presented to the contralateral hemisphere [10]. In the pediatric age group, several authors have noticed significant improvements in behavior and attention in up to 81% of children after callosotomy [17,18].
Complications
Ventriculitis, meningitis, and death have been reported from earlier series of CC. More recent reports have noted fewer complications, including subdural hematoma, asymptomatic venous infarctions, and wound infections. Transient postoperative leg weakness and a decrease in spontaneity of speech is not uncommon after anterior 2/3 section, either from acute disconnection or retraction injury [7].
The Future of CC
The vagal nerve stimulator (VNS) has been proven efficacious at reducing seizure frequency for partial seizures [19-21] and may be useful in primarily generalized epilepsy as well [22]. Long-term results appear promising [23]. Data are lacking on the relative success of VNS compared with CC for controlling generalized epilepsy, but the advantage of the VNS is a significant reduction in operative morbidity and decreased neuropsychological sequelae. Although seizure control will probably not be as effective, the VNS may be used as a first operative intervention, before CC, for unresectable foci.