THE TURN OF the 21st century brought about dazzling advances in biomedical research. The progress made in the field of medicine, and particularly the discovery of stem cells, opened new avenues for treating conditions that would have been incurable otherwise. Though much experimental work has been done on stem cells, the clinical translation is still in initial phases.
Stem cells were identified in the early 1980s from a mouse blastocyst; it took scientists almost two decades before successfully isolating them from human blastocysts. The striking features of stem cells are their qualities of self-renewal and pluripotency, which enable them to develop into various kinds of adult tissue if a suitable environment for nurturing is provided.
By regenerating damaged tissue using stem cells, scientists are trying to find ways to treat many diseases including, but not limited to, Parkinson’s disease, myocardial infarction, diabetes, and spinal cord injury. Although it is too early to say how far the scientists will succeed in treating these conditions, the results so far have been very promising, and researchers are working enthusiastically toward finding a cure for such diseases using stem cells.
Stem cells have been derived from sources such as embryos, umbilical cords, and adults. They have the potential to proliferate multiple times and differentiate into various kinds of tissue. The differentiation of the stem cells can be either spontaneous or occur through a directed mechanism when certain stimuli or agents are present to initiate a specific process. By retaining the property of plasticity, they have the ability to transform into any kind of cell, with the exception of placenta and the extra-embryonic membranes that are formed during the embryonic development. Among all the stem cells, those derived from embryonic tissue have the highest potential for self-renewal and differentiation.
EMBRYONIC STEM CELLS
Embryonic stem cells, the original building blocks of life, are the body’s founder cells. Being undif-ferentiated in nature and capable of self-renewal, they can differentiate into any kind of tissue. They are isolated from the developing embryo.
An ovum and a sperm fertilize to form a zygote, which serially divides to develop into a ball of loosely connected cells, called a morula, by the fourth day of development. The morula then gives rise to an inner and an outer cell mass, which transform into an embryo and extraembryonic tissue (necessary for the initial development of embryo), respectively. The inner cell mass gives rise to three germinal layers—ectoderm, endoderm, and mesoderm—which go on to form different organs and tissues as the embryo matures.
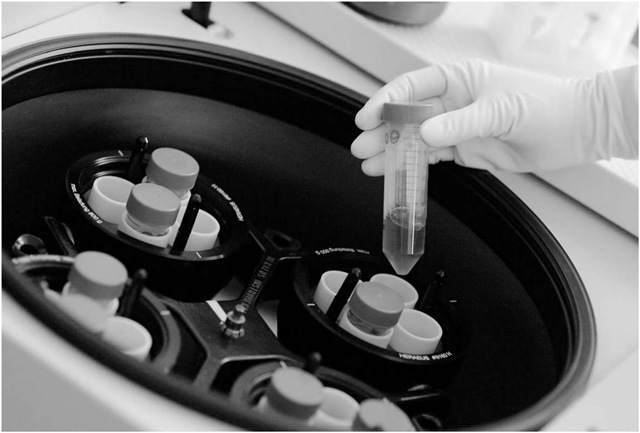
Embryonic stem cells are derived from the inner cell mass of the blastocytes around day four or five postfertilization. After isolation, the embryonic stem cells are cultured in the laboratory, and the stem cell lines are obtained with the potential to differentiate into various kinds of cells when provided with a cytokine cocktail in a suitable environment.
So far, using animal models, researchers have successfully isolated stem cells and shown them to differentiate into various types of cells in both in vitro (outside the body in an artificial environment) and in vivo (within the body) studies. Successful differentiation of embryonic stem cells into neural, vascular, and other solid organ cells was an important milestone that provided enough evidence for scientists to reproduce similar experiments, using human embryonic stem cells. Stem cells therefore were obtained from human embryos that were otherwise to be discarded following in vitro fertilization (a scientific approach to fertilization).
A stem cell policy was immediately drafted by the U.S. government in August 2001 that restrained scientists from using federal funding to obtain any further stem cells by destroying human embryos.
However, it allowed them to continue to work on the almost 60 embryonic stem cell lines that had already been obtained or for which the derivation process had been initiated before the policy’s implementation. The National Institutes of Health (NIH) funded infrastructure awards for the development and distribution of the existing embryonic stem cell lines; this played a vital role in providing 21 well-characterized human embryonic stem cell lines for widespread distribution to scientists for research purposes by March 2007.
Because the federally funded studies can only use the lines registered with NIH before August 2001, passionate scientists have continued their efforts to find other ethically acceptable ways to generate human embryonic stem cells. One such group of scientists is focusing on retrieving stem cells from the dead embryos, and another is trying to come up with a proper definition of embryonic death. There is a hope that if all the scientists, ethicists, and politicians agree on a proper definition of embryonic death, then perhaps some of these dead embryos can be cultured in the laboratory with the hope of retrieving some individual revivable cells, which can be ultimately used to cure diseases or form various organs. In addition, exciting new developments in nuclear transfer techniques hold the promise of patient-specific embryonic stem cell lines.
Germ cells, just like embryonic stem cells, have also been shown to have the potential of self replication. Germ cells are usually derived between week five and nine of development from the gonadal ridge—a part of the embryo that later produces eggs or sperm. However, as compared with the embryonic stem cells, germ cells have less potential for self replication and for tumor formation (an uncontrolled, abnormal, circumscribed growth of cells in any animal tissue; neoplasm). The germ cells will, however, also make tumors if they are not carefully manipulated before implantation.
UMBILICAL CORD STEM CELLS
Although the pluripotency of stem cells obtained from umbilical cords has been controversial in the past, there is now evidence that they are a rich source of stem cells and can be used as an alternative to blastocyst- or gonadal ridge-derived embryonic stem cells.
Containing two arteries and a vein surrounded by some connective tissue, the umbilical cord is a vital structure that connects the developing fetus to the placenta. The stem cells from cord blood are much easier to get because they can be readily obtained from the placenta at the time of delivery. The stem cells isolated from the stromal tissue around the vessels have been shown to transform into chondrogenic, osteogenic, neurogenic, adipo-genic, and several other types of cells. A broader range of recipients may benefit from cord blood stem cells. They are a rich source of early stem cells, particularly hematopoietic cells (blood-forming stem cells), which are used to treat a host of blood-related diseases. Cord blood stem cells also offer some exciting possibilities for gene therapy for certain genetic diseases, especially those involving the immune system.
Because there are few ethical issues surrounding the stem cells derived from umbilical cord, they remain an excellent alternative to embryonic stem cells. Once banked, the umbilical cord stem cells can be transplanted back into the donor, to a family member, or to an unrelated recipient. The high scale of cost for storing cord stem cells makes their use limited to only a few privileged individuals, and prohibitively expensive for the general population.
ADULT STEM CELLS
Although adult stem cells have the potential for differentiation and self-renewal, unlike embryonic and umbilical cord counterparts, they can only differentiate into a limited number of single or multiple cell lines. There is no consensus on their origin. Some think they are the remnants of embryonic stem cells, but others believe them to be a separate entity. They have been isolated from brain, bone marrow, peripheral blood, blood vessels, epithelia of the skin and digestive system, cornea, liver, and pancreas; thus, adult stem cells have been found in tissues that develop from all three embryonic germ layers, that is, ectoderm, endoderm, and mesoderm.
The most common source of adult stem cells has been the bone marrow-derived hematopoi-etic stem cells that have been used extensively in bone marrow transplantation for treating blood cancers like leukemia, multiple myeloma, and so on. Recently, they have also been used to repair damaged cardiac muscles by injecting them into the affected areas to induce the formation of new vessels and improve the functional capacity of the heart. A subset of CD34+ stem cells also has the ability to home into ischemic sites, allowing potential intravenous delivery of such adult stem cells.
Researchers have also isolated adipogenic, osteogenic, and chondrogenic cell lines from bone marrow-derived cells in addition to blood cell lines. Adult stem cells in the central nervous system have been shown to develop into astrocytes, neurons, and oligodendrocytes and are usually concentrated in some specific areas of the brain. Because adult stem cells are derived from, and later are transplanted back to, the same patient, there is no risk of immune reaction, unlike with embryonic stem cells, where immunosuppression therapy may be needed to avoid cell rejection.
Some scientists have shown a concern that adult cells may have comparatively higher chances of mutation (a sudden structural change within a gene or chromosome resulting in the creation of a new character or trait not found in the parental type) and less pluripotency; however, this may not be true unless adult stem cells are made to pass through more than 30 doublings—a practice that is not done clinically, per U.S. Food and Drug Administration regulatory guidelines.
While debate has centered around embryonic stem cells, stem cells can be derived from a number of sources, including from umbilical cords and adult patients.
conclusions
Although stem cell research has progressed tremendously over the last two and a half decades, scientists are still facing many challenges that need to be addressed before stem cells can be safely and regularly used for treating various diseases. However, there is a consensus that they can have a lot of advantages and may play a pivotal role in treating various medical illnesses.
Scientists are also trying to obtain embryonic stem cells by alternative ways that will be ethically as well as scientifically acceptable. Given the successful use of mesenchymal stem cells in bone marrow transplant and the preliminary promising results of some clinical trials from Europe involving human stem cells, there is no doubt that stem cell therapy—if and when applied after having addressed all the current concerns revolving around it—will revolutionize the practice of medicine in the future.