Clinical Application
There are several factors that affect the accuracy of the waveform or the perfusion index. In low blood flow states (e.g., hypotension from shock or cardiac arrest), there may not be a sufficient movement of blood through the capillary bed to provide an accurate reading. Decreased capillary blood flow can also occur when the sensor site is cold and the blood vessels are constricted. Vasoconstriction is a normal response to cold, shunting warm blood toward the core to maintain a normal body temperature; however, it can be problematic when attempting to obtain an accurate SpO2 reading. Vibration from shivering and motion artifact during transport may also affect the quality of the waveform, although this is not as much of an issue with the later models of pulse oximeters. Nail polish may affect the ability of the light to pass through the fingertip and may need to be removed if a poor waveform or inadequate perfusion index is noted. Finally, the pulse oxi-meter is inaccurate below an SpO2 of 70% because the reference database in the machine does not contain information below 70%.
A normal SpO2 reading doesn’t mean the patient does not require supplemental oxygen. While anemia, or decreased hemoglobin, does not affect the SpO2, total blood oxygen content—and therefore the delivery of oxygen to the tissues—is decreased. Total blood oxygen content depends on the amount of hemoglobin in the blood and the amount of oxygen diffused into the blood. The total amount of dissolved oxygen in the blood can be increased by administering supplemental oxygen to patients suspected of anemia from acute blood loss, and may help prevent tissue hypoxia from inadequate oxygen transport. Patients in respiratory distress or shock often increase their respiratory rate and pulse rate in order to move more oxygen into the blood and circulate more oxygen to the tissues in response to a lack of oxygen at the tissues. In many cases, a patient in respiratory distress will be able to improve his SpO2 by increasing his respiratory rate and compensating for his hypoxemia.
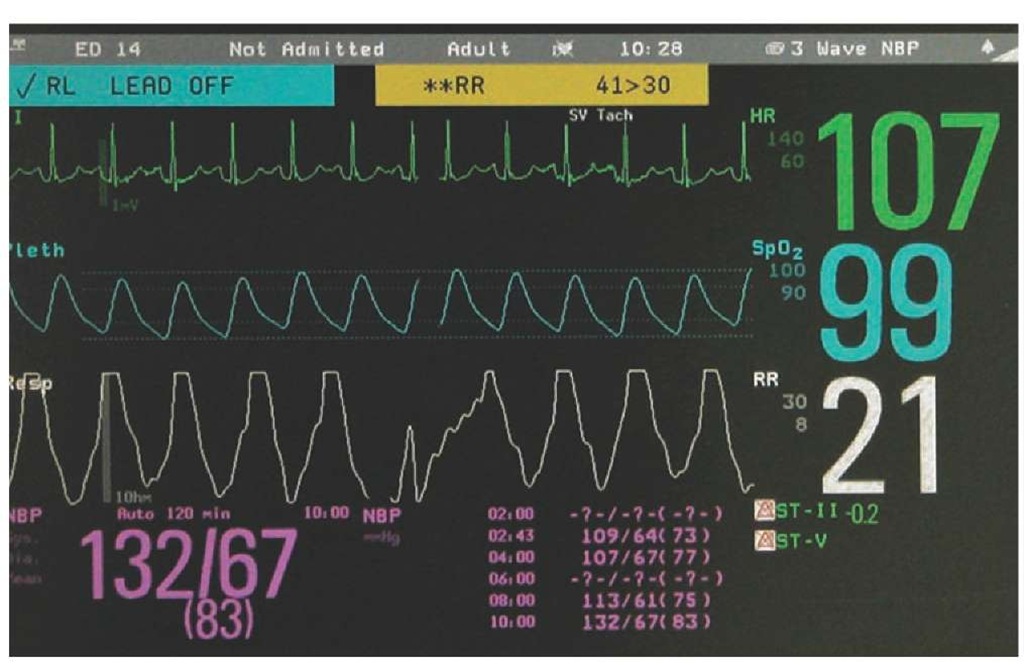
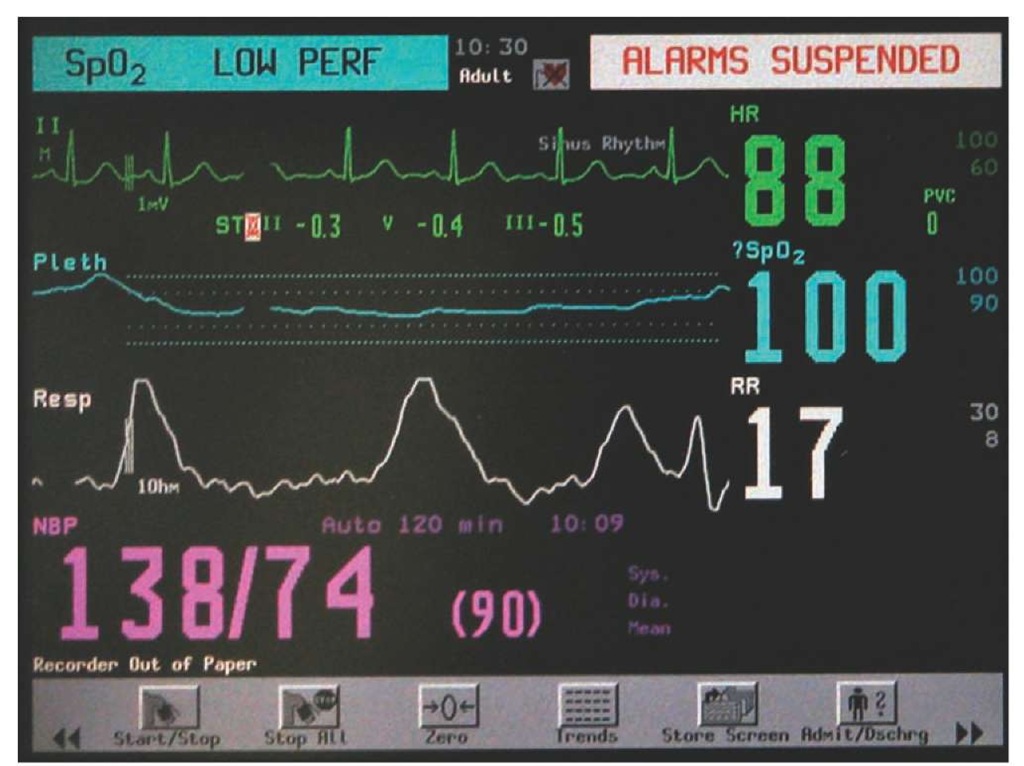
Figure 25-8 Normal pulse oximetry waveform.
Figure 25-9 Poor waveform that affects the accuracy of the SpO2 reading.
Certain conditions will also affect the SpO2 reading. Carbon monoxide also attaches to hemoglobin; because, it has a significantly higher affinity than oxygen. This means that carbon monoxide is 200 times more likely to attach to the hemoglobin molecule than oxygen, creating carboxyhemo-globin. Though the hemoglobin is bound to carbon monoxide rather than oxygen, the wavelengths of light used in first generation pulse oximeters are not capable of differentiating the two hemoglobins. A patient who has had carbon monoxide poisoning may demonstrate a normal SpO2. Other forms of hemoglobin (more specifically, one form called methemoglo-bin) will also provide a false SpO2 reading. Methemoglobin is a form of hemoglobin that is chemically different from hemoglobin and cannot carry oxygen. This is often the form hemoglobin takes as it reaches the end of its useful life. A small amount of methemoglobin is present in the blood at all times. However, the level can be markedly increased in some conditions, decreasing oxygen transport. Fortunately, co-oximeters are available that can detect the presence of these two conditions. This will be discussed later in this topic.
Pulse oximetry also does not provide an indication or measure of the patient’s ventilatory status. This is especially true when the patient is on high-flow supplemental oxygen. The supplemental oxygen can replace the other gasses in the lungs, increasing the oxygen gradient between the alveoli and the pulmonary capillary blood. This encourages transport of oxygen into the blood, even when there is insufficient airflow in and out of the lungs. That airflow in and out of the lungs (ventilation) is required to remove carbon dioxide from the system. With inadequate airflow, the carbon dioxide levels increase in the alveoli, decreasing the gradient from the blood to the alveoli, reducing carbon dioxide transport and therefore increasing blood carbon dioxide levels. Pulse oximetry alone would not detect this hypoventilation. This is well illustrated in a case report from 1993, approximately 5 to 10 years after pulse oximetry’s introduction into regular clinical use.3 In this case report, an elderly woman was monitored after a surgical procedure with blood pressure, ECG, and pulse oximetry on supplemental oxygen after her procedure. The patient became less and less responsive. Finally, the nurses could not wake the patient up. The patient was seen by the anesthesiologist, was noted to be ventilating very poorly, and was intubated and placed in the ICU until she woke up. The pCO2 on her blood gas was 280 mmHg, with a normal pCO2 at 40 mmHg. Most patients who acutely develop a pCO2 over 80 or 90 mmHg become minimally responsive or unresponsive. The patient’s SpO2 never fell below 96%. The take-home message from this case is while pulse oximetry is an excellent tool to help assess a patient’s oxygenation and ability to oxygenate a patient, it cannot detect hypercapnea, or a rise in CO2, from inadequate ventilation. This is where capnography can help.
Capnography
Capnography, the measurement of the amount of carbon dioxide exhaled from the lungs, is a newer technology that can help guide the Paramedic with treatment in several clinical situations. Several different methods of capnography are available to measure exhaled carbon dioxide. The measurement often cited is the end-tidal carbon dioxide, which is the amount of carbon dioxide in the air at the end of exhalation. End-tidal carbon dioxide is abbreviated as EtCO2. The three methods of measuring EtCO2 include colorimetric capnometry, quantitative (numerical) capnometry, and waveform capnography.
Colorimetric capnometry is a familiar form of EtCO2 for many Paramedics. This device consists of a piece of litmus paper within the sensor’s body. This paper is impregnated with a chemical that changes color when exposed to exhaled carbon dioxide (Figure 25-10). This device is placed in-line with the endotracheal tube immediately after endotracheal intubation to help confirm that the the endotracheal tube is in the trachea. If the endotracheal tube is in the trachea the capnometer should change color from purple up to yellow depending on the amount of carbon dioxide in the exhaled air. One exception is when a patient has been in cardiac arrest for a prolonged period of time. In this situation, very little CO2 is transported to the lungs because of circulatory collapse, therefore there is little in the lungs and a low level in exhaled gas.
The colorimetric capnometer is a qualitative device, meaning it gives gross estimations of the presence or absence of carbon dioxide and not specific levels of carbon dioxide. This, and other limitations, give colorimetric capnometry limited utility in the prehospital setting. Some Paramedics only use colorimetric capnometer as an initial method of endotracheal confirmation then utilize continuous waveform capnography or capnometers.
Figure 25-10 The EasyCap® colorimetric capnometer. The color changes from purple when exposed to > 4 mmHg CO2, to tan, and then to yellow when exposed to > 15 mmHg CO2.
Quantitative capnometers provide a numerical value for the EtCO2, reporting the CO2 measurement at the end of exhalation. In contrast, waveform capnography records the values of exhaled carbon dioxide throughout the inspiration-expiration cycle and graphs that value over time, producing a waveform that can be clinically useful to interpret.
Technology
As previously described, the colorimetric capnometers utilize a paper impregnated with a chemical that changes color depending upon the amount of carbon dioxide in the exhaled air. For quantitative capnometry and waveform capnogra-phy, the amount of carbon dioxide in exhaled air is found by shining a beam of infrared light through a sample of the exhaled breath. The intensity of the light is then compared to a measurement taken from an air sample that does not contain carbon dioxide. The certain wavelengths of infrared light are absorbed by the presence of carbon dioxide compared to the air that does not contain carbon dioxide. This is converted into a numerical measure of the carbon dioxide.
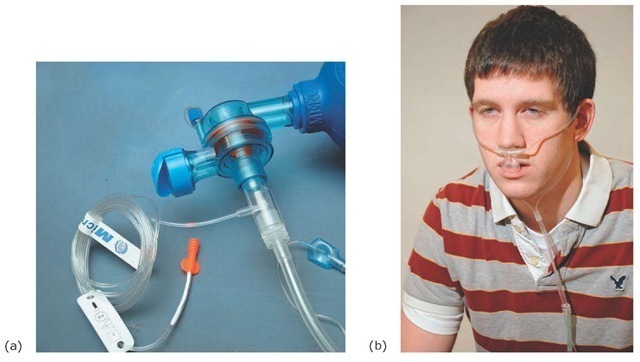
Exhaled air for use in capnography or capnometer is sampled in one of two different methods. Mainstream capnography involves placing the sensor in-line with the exhaled air stream and can only be used in intubated patients (Figure 25-11a). The sensor is placed between the endotracheal tube and the ventilation device (e.g., bag-valve mask assembly).
The second method is called sidestream sampling. Side-stream capnography involves taking a sample of the exhaled air by aspirating a small amount of it from the exhaled air stream, either from the endotracheal tube or through the use of a modified nasal cannula (Figure 25-11b). Sidestream technology allows capnography to be used in patients who are not intubated.
One disadvantage to sidestream capnography/capnometer is that there is some loss of carbon dioxide from the air sample that occurs between the patient and the monitor. This is overcome in many capnography/capnometer devices by calibrating the EtCO2 monitor whenever the monitor switches measurement methods from endotracheal measurements to nasal cannula.
A second disadvantage of nasal cannula sidestream capnography/capnometer is if the patient is receiving high-flow oxygen (e.g., using a nonrebreather or CPAP mask) at the time of sampling, the result will be artificially low because the high-flow oxygen blowing past the sampling port will wash out much of the carbon dioxide in the exhaled air.
The sampled exhaled air is taken to a chamber where a beam of infrared light is directed through the sample. The carbon dioxide present in the air absorbs some of the infrared light, changing the wavelength of the light that continues through to the sensor. This change in wavelength varies with the amount of carbon dioxide present in the sample. The sample taken from exhaled air is compared with infrared light beamed through a sample with a known concentration of carbon dioxide. This comparison determines the level of exhaled carbon dioxide in the patient’s breath. In the absence of respiratory disease, this measure of exhaled carbon dioxide should be within 5 mmHg of the partial pressure of carbon dioxide (PaCO2) of the patient’s arterial blood.
Figure 25-11 Mainstream versus sidestream sampling. (a) In mainstream capnography, the sensor is located between the endotracheal tube and the bag-mask assembly. (b) A modified nasal cannula is used to sample carbon dioxide from exhaled air.
Capnography: Waveform Interpretation
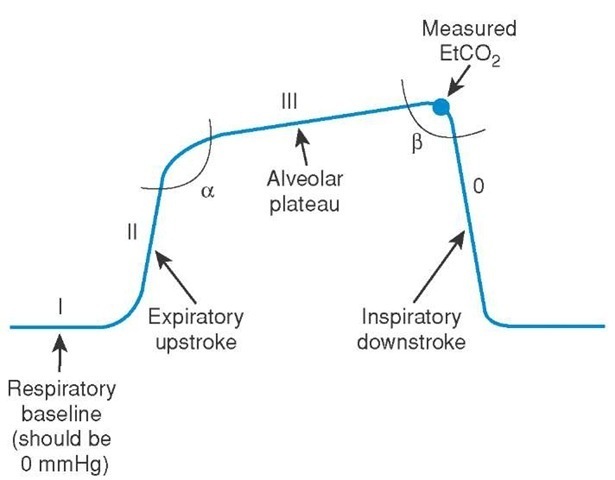
Unlike capnometers which either provide a visible color change or a numeric readout, a capnography provides a graph of the EtCO2 measurement as it changes during inspiration and expiration (Figure 25-12), The capnography waveform has several components, each representing a phase.
Phase I is the respiratory baseline and occurs at the time between inhalation and exhalation. It should be at zero, as it represents the carbon dioxide in free air, that is found in the anatomical dead space in the lungs.4 The next part of the waveform, Phase II, is also called the expiratory upstroke and represents the beginning of exhalation of air from the lungs that contains carbon dioxide. The third part of the waveform, known as Phase III or the alveolar plateau, represents exhalation of alveolar air during exhalation. The peak of this plateau at the end of exhalation is the EtCO2 measurement displayed on the monitor. The final portion of the waveform is the inspiratory downstroke or Phase 0, and represents the patient’s inspiration. During the inspiratory downstroke, the EtCO2 falls rapidly to zero, as the inspired air should contain little carbon dioxide.
Figure 25-12 Anatomy of a typical end-tidal capnography waveform.
The first angle on the waveform, the alpha angle, is the angle between Phase I and II and indicates the correlation between ventilation and perfusion in the lung (i.e., the movement of air in and out versus the flow of blood through the lungs). The second angle, the beta angle, the angle between Phase III and 0, is usually close to a 90-degree angle. However, it will increase if the patient is rebreathing exhaled carbon dioxide, as can occur if the oxygen flow rate on a nonrebreather is inadequate and the reservoir bag does not refill between breaths.