Inflammation: Acute Phase
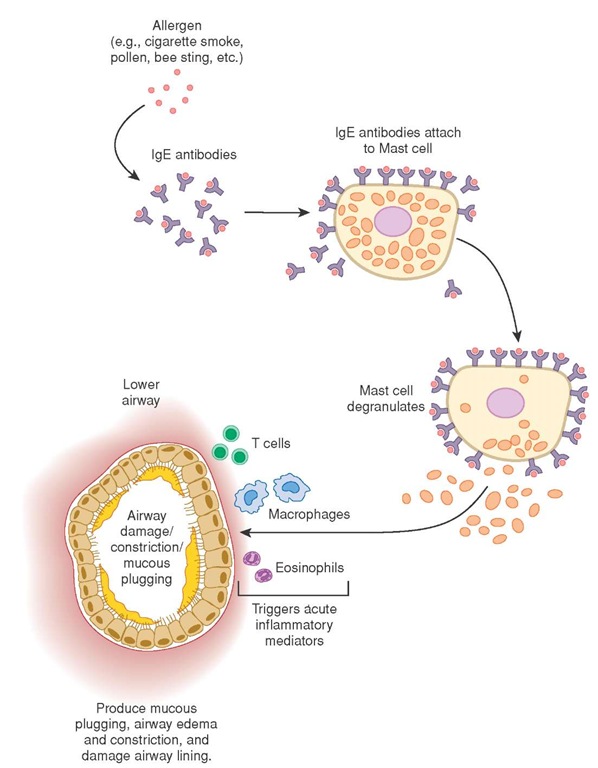
Forward scouts, the mast cells contained in the bloodstream, are triggered by trauma, hypoxia, toxins, or any source of cellular injury. They respond from the bloodstream almost immediately. Outwardly, the response of the inflammatory system is visible as redness (rubor), swelling (tumor), pain (dolor), and warmth (calor) at the injury site.
Looking beneath these outward manifestations, a complex process of inflammation is revealed. Mast cells, containing granules of chemical mediators like histamine and serotonin, break down or degranulate, releasing their contents into the surrounding interstitial fluids (Figure 11-12).
The chemical mediators histamine and serotonin cause vasoconstriction of the smooth muscle in the surrounding arterioles, thereby limiting the spread of injury. They also dilate the postcapillary venules, resulting in swelling and pain. Dilation of the capillary beds is important because it increases the permeability of the capillary walls and allows more white blood cells to migrate out of the blood and into the interstitial space surrounding the cells. The collection of white blood cells and fluids is called an exudate.
Mast cells also release two chemical messengers: chemotactic factors, which attract specific leukocytes (white blood cells) to the injury site. These chemotactic factors— neutrophil chemotactic factor and eosinophil chemotactic factor of anaphylaxis (ECF-A)—bring out the workhorses of inflammation—neutrophils and eosinophils—during the early stages of the inflammatory response.
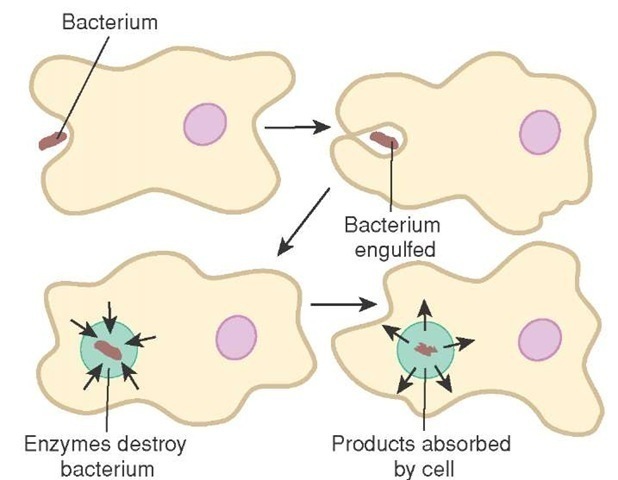
Neutrophils destroy bacteria by engulfing them in a process called phagocytosis (Figure 11-13). Then the neutrophils break down the bacteria with their lysosomes. Eosinophils destroy parasitic infestations, such as helminthes (worms), and release enzymes that slow the inflammatory response.30 Chief amongst these enzymes is histaminase, an enzyme that breaks down histamine.
Figure 11-12 Mast cell degranulation.
Inflammation: Prolonged or Chronic
Mast cells also create chemical mediators such as leukotrienes (slow acting substances of anaphylaxis— SRS-A). Leukotrienes produce chemical effects which are similar to histamine and help to prolong the inflammation, if necessary. Leukotrienes could be considered as long-acting histamine.
Perhaps most notable to the patient is the presence of prostaglandins, a chemical mediator released from the mast cell that creates the sensation of pain. However, the primary function of prostaglandins is not to create pain but to increase vascular permeability and smooth muscle contraction later in the inflammatory response.
If the infection is persistent (i.e., greater than 24 hours), then monocytes, which later become macrophages, come to the aid of the neutrophils and a similar process continues.31 At this stage the body typically mounts a fever response. The fever is induced by chemicals from the neutrophils and the macrophages, which are released after exposure to the bacterial remains (endotoxins).
The cellular remnants of this battle, containing dead and dying leukocytes and bacterial remains, either migrate to the skin’s surface as pus or are carried away in the lymphatic system as purulent exudate. If the purulent exudate is walled off in a specific area, then it is called an abscess. Abscesses can be difficult to resolve without a surgical procedure such as incision and drainage (I&D).32
Figure 11-13 Neutrophils engaged in phagocytosis of an invading bacteria.
Support for Inflammation: The Complement System
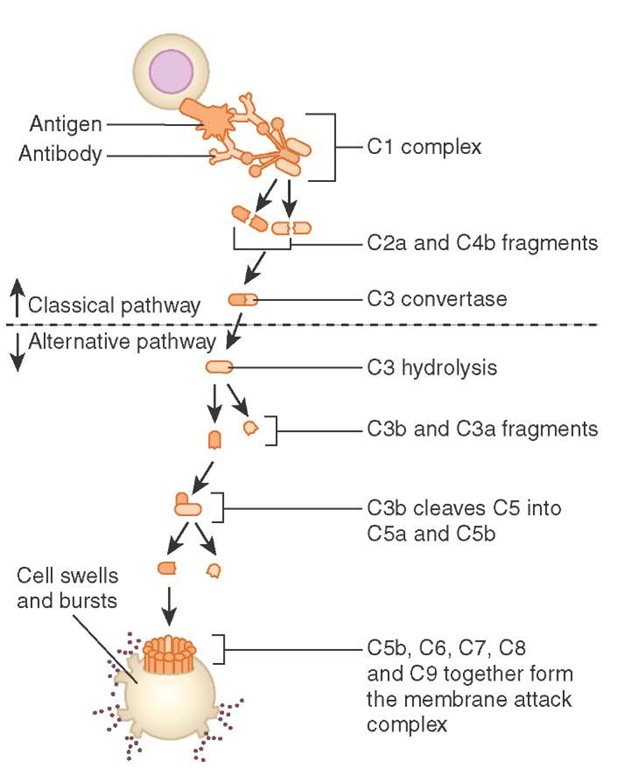
The complement system, as the name suggests, supports and controls the inflammatory response. Plasma proteins circulate in the blood and make up almost one half of the blood proteins. The other half of the blood proteins are albumin. The blood proteins comprise the complement system and can be activated by either one of two mechanisms.
The first mechanism includes the classic pathway, an immune complex, in which an antibody (e.g., IgG or IgM) has attached to an antigen and stimulates the complement system. The activated plasma proteins of the complement system act as anaphylatoxins, increasing the degranulation of mast cells and attracting other white blood cells (leukocytes) to the site. The plasma proteins mark resistant bacterium by attaching fragments ofthemselves to the bacterial cell wall, a process called opsonization, thus enhancing the impact of the leukocytes.
With the second mechanism, the alternative pathway, toxins secreted by the bacterium or fungi stimulate the complement system and cause all of the same effects as the classic pathway.
In some cases the body does not recognize the bacteria and cannot mount an effective antigen-antibody defense. In those cases, the complement system creates a membrane attack complex (MAC), which attaches itself to the cell’s walls and forms a tube from the outside to the inside. The tube allows water to enter the cell, the cell to swell, and the cell to lysis (Figure 11-14).
Support for Inflammation: The Coagulation System
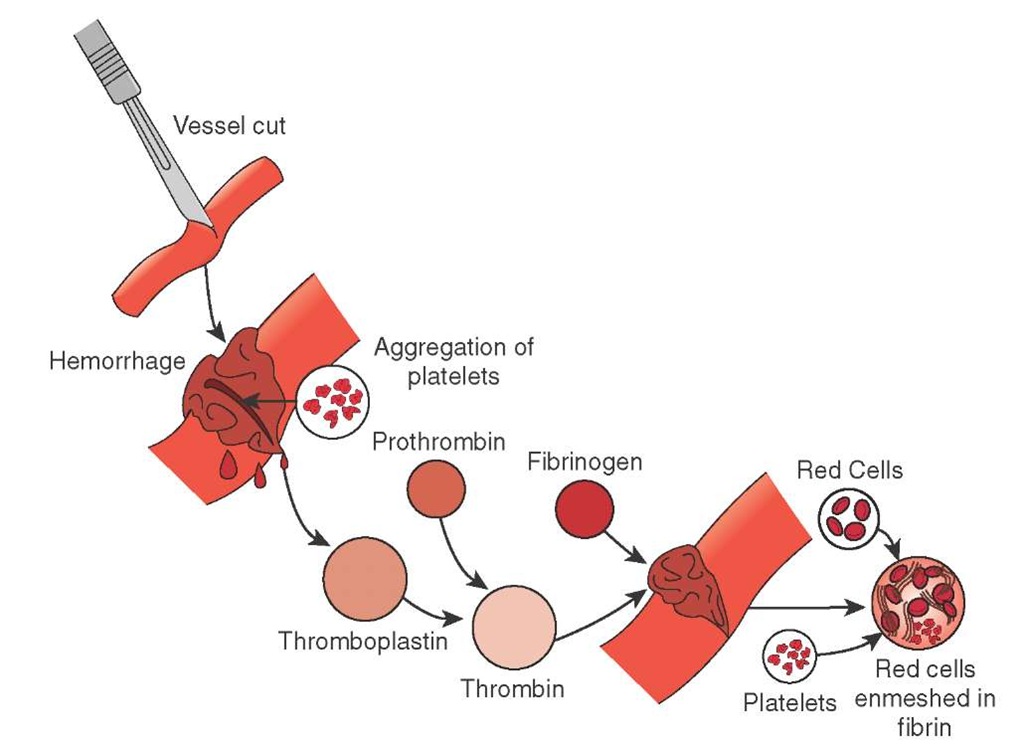
The term "coagulation" evokes thoughts of blood clots and hemorrhage. However, during the inflammatory response the coagulation system acts to entrap fluids (exudates) and foreign bodies (Figure 11-15).
Both endotoxins (via the extrinsic pathway) and kinins (via the intrinsic pathway) can stimulate the coagulation cascade to begin. Circulating prothrombin, a plasma protein, is converted into thrombin, which in turn is converted into fibrinogen and then fibrin. The resulting fibrin net prevents the spread of the infection to adjunct tissues by essentially walling off the site.
Perhaps as important as preventing the spread of infection, the fibrin net keeps the offending microorganisms confined to a smaller area for phagocytic action by neutrophils and macrophages. Finally, the fibrin net serves as scaffolding for scar formation and healing.
Support for Inflammation: The Kinin System
Another class of circulating plasma proteins is the kinin group, made up of chains of amino acids. Like the coagulation cascade, kallikrein is activated and converted to bradykinin in a cascade. However, kallikrein is present in sweat, tears, saliva, urine, and feces and can be converted into bradykinin.
Figure 11-14 The complement system creating a membrane attack complex.
Figure 11-15 Coagulation.
Bradykinin is similar to histamine in its actions. It causes vasodilation, increased permeability of the vascular bed, and works with prostaglandins to produce pain. Bradykinin was first discovered in Brazil by three pharmacologists working with snake venom which caused circulatory collapse. Using this early work, scientists developed a new class of antihypertensive drugs called ACE inhibitors.
Immune Response
The immune response is the body’s specific defense against substances that are not part of the body (by definition, antigens). Antigens can be exogenous, from outside of the body, and enter the body by injection, ingestion, or inhalation. Antigens can also be endogenous, from within the body (e.g., a virus that has replicated within a cell). Whatever the source of the antigen, the body’s immune system reacts.
Lymphocytes within the body respond to the site of injury and, depending on the type of lymphocyte, incapacitate the antigen. B lymphocytes, from bone marrow, produce antibodies that then attack the cell. T lymphocytes, from the thymus gland, recognize the antigen and attack it directly.
B Lymphocytes
After an infection, some remaining B lymphocytes remain in contact with the antigen. This contact stimulates the B lymphocyte to divide. The resulting clones can either have a memory of the antigen, called memory cells, or they become plasma cells. Plasma cells generate antibodies, a type of protein globulin called immunoglobulins.
Five types of immunoglobulins have been identified: IgA, IgD, IgE, IgG (gamma globulin), and IgM, and each immunoglobulin fits into the surface of an antigen in a key and lock fashion, linking them together. The result of this union is to either neutralize bacterial toxins or activate the complement system. Complement proteins then cause the swelling and rupture of the cells via membrane attack complexes.
If the same antigen is introduced again, circulating memory cells will recognize the antigen and plasma cells will start to release antibodies. This phenomenon is called humoral immunity.
T Lymphocytes
Originating in the bone marrow with B lymphocytes, T lymphocytes travel to the thymus where they mature and exit the thymus immunocompetent (i.e., capable of providing immunity) and travel to the lymphatic system. Once in the lymphatic system, specific cytotoxic T lymphocytes, or killer T cells, attack antigens which antibodies could not bind to. They form an antigen-antibody complex (i.e., antigens for which the patient does not yet have immunity).
Cytotoxic T cells can release lymphokine, a chemical that attracts macrophages, or they can release cell-killing toxins. Some even release interferon, a glucoprotein that inhibits cell growth.
Helper T cells bind to macrophages or B lymphocytes and together produce a protein (interleukin) which stimulates more production of both B and T lymphocytes. The resulting activity of T lymphocytes produces cell-mediated immunity.