Painless Injections
Patients complain, sometimes bitterly, about the discomfort which can accompany an intramuscular injection. This discomfort can be related to the needle puncture and the tearing/shearing of the dermis and muscle as the needle passes through the tissue layers, as well as the presence of the medication within the tissue.
Several products are available that help to reduce the pain of needle insertion. The first, a eutectic mixture of local anesthetics (EMLA), is a cream of lidocaine 2.5% and prilo-caine 2.5%. EMLA is available as a self-adhesive anesthetic disk or a cream that is applied to the intended injection site and left in place for a minimum of 60 minutes. Following removal of the dollop of cream, or the patch, the skin should be anesthetized.53,54 While EMLA cream may not be convenient for use in the field, it should be considered in cases where repeated injections of medicine may be needed.
Alternatively, fluori-methane has great potential for use in the field.55-57 Fluori-methane, a topical refrigerant, numbs the skin at the injection site in as little as 15 seconds. Fluori-methane, also referred to as a vapocoolant spray, can be either applied directly to the skin, though some patients complain of transient sharp discomfort, or onto a cotton ball for topical application. One study suggested that a vapocool-ant spray was equally as effective as EMLA cream. Another study indicated that placing ice alone on the skin, for 30 seconds, was not effective in reducing pain during injection.
The next potential source of injection pain is the trauma created by the needle’s insertion. One study suggests that the biomechanics of injection (i.e., proper injection technique) is important to the patient’s comfort.58-61 A needle held and inserted in a linear manner, perpendicular to the plane of the skin, reduces the "path width" compared to the path width seen with a curved (arcing) needle path. Tissue shearing is minimized and therefore patient discomfort lessened.
Finally, there is the matter of the medication deposited within the muscle. This discomfort is, in large part, due to the leakage of the caustic and irritating drugs into the pain receptors of the subcutaneous tissues. The deeper muscle layers are relatively free of pain receptors. The application of a few easy to perform techniques which "lock" the drugs into the muscle will decrease the patient’s discomfort and improve the Paramedic’s confidence with injection skills.
Two techniques have been developed by nurses to decrease this leakage and the accompanying discomfort. Both techniques involve careful attention to the particulars of the injection technique. The first technique, the airlock, is performed while preparing the drug in the syringe for injection. The second technique, the Z-track, involves manipulation of the injection site during the injection.
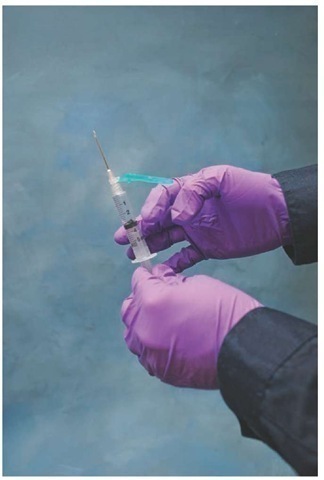
The airlock technique has the Paramedic injecting a small bubble of air into the injection, essentially sealing off the drug below from leaking out to the subcutaneous tissues above. To create an airlock, the Paramedic fills the syringe with the medication as usual. With the syringe clear of the ampoule, the Paramedic would then withdraw the plunger further, clearing the drug from the needle and entraining about 0.1 mL of air into the syringe. It is important that the Paramedic verify that the correct volume of drug remains in the syringe (Figure 26-13).
Quickly inverting the syringe should cause an air bubble to be created at the apex of the plunger. With the air bubble in place, the Paramedic would proceed to the injection. For the airlock technique to work, it is essential that the syringe remain at an upright 90-degree plane from the injection surface. This ensures that the air bubble is injected at the end of the injection. The ventrogluteal (VG) site and the dorsal gluteal (DG) site are conducive to this technique.
Figure 26-13 Airlock technique.
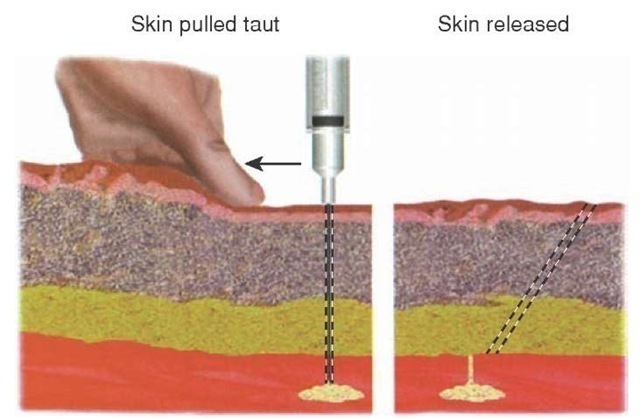
Another technique that can help prevent drug leakage into the subcutaneous tissue is the Z-track technique. The Z-track technique creates an offset injection pathway, using subcutaneous tissue to block leakage.62
To create a Z-track, the Paramedic with the drug-filled syringe in the dominant hand, bevel up, would pull gentle traction on the injection site with the nondominant hand. Frequently, Paramedics will grasp the upper arm, if the deltoid is used, and pull traction with the thumb of the nondominant hand. With a smart flick of the wrist, as if one was throwing a dart, the needle is inserted into the skin. After aspiration confirms proper placement, the drug is injected in a deliberate fashion. Injecting the drug too quickly can create discomfort as stretch receptors are stimulated by the presence of the space-occupying depot of medicine. Alternatively, injecting, or "pushing," the drug too slowly can cause increased patient apprehension. Practice establishes the best rate of administration.
The next actions taken by the Paramedic are critical to the success of the Z-track technique (Figure 26-14). Before the needle is withdrawn from the skin, the Paramedic must release the traction on the skin. Thus, when the needle is completely withdrawn the skin overlying the muscle will slide over the medication depot, closing it off to the surface.
Figure 26-14 Z-track injection technique.
Injection Site Massage
Some controversy surrounds the common practice of massaging the area surrounding the injection site immediately after the injection. In some cases, it is acceptable to gently massage the area surrounding the injection. Gentle pressure applied to the area dissipates the impact of the sharp pain receptors through competition with various pain fibers. However, some medications are caustic to the muscle tissue. With these medications, massaging the area distributes the medication over a larger area, creating more discomfort for the patient.
The Paramedic should be knowledgeable about the medication before just routinely proceeding with massaging all injection sites. For example, it is acceptable to massage the site following an injection of morphine sulfate in order to decrease the patient’s discomfort, but massaging the site after an injection of diazepam would only serve to increase the patient’s discomfort.
Also at issue with the routine practice of massaging an injection site is its impact on absorption. While intramuscular injection of insulin is uncommon, its rate of absorption is quicker via intramuscular injection than subcutaneous injection. This quality makes intramuscularly injected insulin attractive during a diabetic emergency. However, massage of the injection site can dissipate the insulin even further, making its uptake more rapid and creating a risk of unanticipated hypoglycemia. If the Paramedic is unsure if massaging the injection site is acceptable, then the maxim of "do no harm" should be followed and the injection site should not be massaged.
Special Populations
The two extremes of age—elderly and children—each present a special challenge for the Paramedic who must perform an injection. Both the patient and the provider alike are anxious during a pediatric injection. To develop strategies to improve success, the Paramedic must take into account the child’s developmental stage and adjust the approach accordingly.
In many cases, the infant is unaware of the events surrounding him or her, but is acutely aware of the discomfort that follows. In those cases, it may be acceptable to have the infant held in the mother’s arms to be comforted after the procedure.
The greatest challenge may be the toddler. The toddler is keenly aware of his or her environment, is able to comprehend the situation, and receives a great deal of emotional feedback from parents as well as caregivers. Typically, a toddler must be temporarily restrained during the injection. One technique is to place the toddler on the parent’s lap, chest to chest, with the parent’s arms entrapping the child. The toddler’s legs would then be aside and behind the parent. The Paramedic would approach the parent from behind, grasp the outstretched leg, and perform the injection.
The elderly patient presents a challenge of another kind. The combination of age and poor nutrition reduces muscle mass, limiting available injection sites. These emaciated patients, with less muscle mass and loss of the capillary beds, tend to absorb medications less readily.
STREET SMART
Uninformed Paramedics mistakenly think it is preferable to inject medications below the level of injury of a paraplegia patient, eliminating the pain which can accompany an injection. The drug absorption below the level of the spinal injury is erratic and unpredictable.
Conclusion
The large number of medication administration routes and techniques represent a substantial portion of the universe of skills that a Paramedic must master. Each medication route has its advantages and its drawbacks, its indications and its contraindications. It is the Paramedic’s responsibility to ensure that the patient’s medication needs and the preferred medication route are compatible.
key points:
• It is a Paramedic’s responsibility to choose the right drug and the right dose for the patient, and to administer it by the right route at the right time in order to achieve the optimal therapeutic effect.
• Forms of medication can be grossly categorized into liquids, solids, and injectable liquids.
• Injectable forms of medication come in either ampoules or vials. Vials are essentially resealable ampoules and may be used for multiple patients.
• The apothecary system of measurements includes units of grain (gr) and is rarely used today by physicians.
• The common household system or United States customary system contains such units as the ounce and the teaspoon and remains the predominant system of measurement in the United States and Canada.
• The metric system is based in units of 10.
• Insulin and penicillin are examples of medications that are measured in international units (IU). This unit represents the relative strength of the substance after it has been tested on an organism.
• Conversions of metric measurements are based on a factor of 10. All multiplications above 1 gram are noted in the Greek prefixes kilo-, hecto-, and deca-, whereas all divisions of a gram are noted by the Latin prefixes deci-, centi-, milli-, and micro-.
• The most accurate method of converting a patient’s weight from pounds to kilograms is dividing the patient’s weight in pounds by 2.26 and obtaining the weight in kilograms. However, the Paramedic may also divide the patient’s weight, in pounds, in half, then subtract 10% off from the result for an approximate weight.
• A drug concentration is described as the amount of drug in 1 milliliter (mL) of a solution.
• Some prehospital medications must be mixed just before use to ensure maximum effectiveness.
• A standard drug order states the amount of the drug, the name of the drug, and the route that is to be administered.
• When an adult dose must be adjusted to a pediatric dose, and the pediatric dosing is not available, then the child’s total body surface area (BSA) is divided against the total body surface area of an adult-approximately 1.73 meters squared for a 6-foot tall, 150-pound adult. The resulting percentage is then taken from the adult dose and is roughly equal to the pediatric dose.
• Intravenous fluids may be infused at a "wide open" rate to administer a large volume of fluid quickly, at a prescribed rate per hour or minute, or at a KVO rate of 50 mL per hour to keep the catheter patent.
• Methods for determining an intravenous drug infusion rate include the formula method and the clock method.
• Weight-dependent intravenous drug infusions include the patient’s weight in the standard drug infusion calculation.
• To convert Fahrenheit to Celsius (medical standard temperature measurement), the EMS provider subtracts 32 from the Fahrenheit result and then multiplies by 5/9.
• Paramedics practice the five rights of medication administration.
• After being given any drug, the patient is reevaluated to see if the drug was effective. This re-evaluation, and subsequent documentation of patient response to medication, is so important that some Paramedics refer to it as the sixth right, the right documentation.
• The initials DARE, a simple mnemonic, can help Paramedics remember the elements of documentation for every medication administration.
• The Paramedic can use the mnemonic AIR to obtain an informed consent from a competent patient.
• Local routes of medication administration are intended to target a specific organ or function. Optic medications are applied directly to the eye, and otic medications are applied to the ear.
• The inner mucosa of the nostrils has a rich capillary bed that is an excellent route for the administration of systemic medications. Local nasal medications can be applied via an atomizer into the intended nostril, propelling the medicine against the mucosa. Like the nose, the mouth has a capillary-rich mucosa that will rapidly absorb any medicine and distribute it systemically.
• Though not widely used, local topical medications may include the application of a topical antibiotic at the insertion site of an intravenous catheter. Other local medications can be douches (solutions introduced into the vagina via an apparatus) or enemas (solutions introduced into the anus via an apparatus).
• The enteral route of systemic drug administration refers to medications given via the gastrointestinal tract (e.g., oral medications). Parenteral routes of medication administration include inhalation and injection.
• The sublingual route is an enteral route whereby medication, in a liquid or solid form, is placed in the space inferior to the tongue, where it is rapidly absorbed. The distinct advantage to the sublingual route is that it bypasses the liver and thus avoids hepatic first pass metabolism. Using the buccal route, or cheek, is similar to administering medications sublingually.
• The vast majority of self-administered medications are swallowed. The solid pill, capsule, or liquid is then absorbed in the gastrointestinal tract, where it is passed (via the portal circulation) through the liver and on into the central circulation. From an EMS perspective, the patient must be able to maintain the airway independently and swallow the medication.
• Gastric tubes can be placed to instill feedings as well as medications in the form of liquids or suspensions. Most Paramedics insert an orogastric tube in order to evacuate or decompress the stomach. Use of a special gastric tube, called a Sengstaken-Blakemore tube, permits the Paramedic to apply direct pressure inside the stomach or esophagus to the source of bleeding.
• Intermittent suction or the placement of a dual-lumen gastric tube helps prevent a gastric tube from adhering to the gastric mucosa, leading to local irritation and bleeding. After the placement of a gastric tube, the patient should be monitored for signs of hypoxia, such as premature ventricular contractions (PVC), and altered level of responsiveness. If the gastric tube is obstructed, the Paramedic can irrigate the tube with saline or sterile water instilled into the tube via syringe.
• Drugs that are absorbed from the rectum avoid inactivation by stomach acids and intestinal enzymes. Around 50% of the absorbed drug bypasses the portal circulation, minimizing the impacts of first pass metabolism and biotransformation. To administer the medication, the patient is placed in a modified left lateral position, called the Sim’s position. The rectal administration route is useful when the patient is unable to accept oral medications, such as in the case of persistent vomiting or continuous seizures in children.
• When a rapid onset of drug action is required (e.g., during an emergency), the parenteral route offers the most direct route to the target organs, sidestepping the gastrointestinal system (enteral administration) and delivering drugs directly to the central circulation. Advantages of these routes include circumventing the GI absorption process, maintaining more predictable serum drug levels, and using them with patients who are uncooperative or incapable of cooperation (e.g., unconscious).
• Intranasal administration takes advantage of the nasal passages. They are lined with very vascular mucous membranes that can absorb medications quickly and without the risk of first pass metabolism associated with enteral routes of drug administration. The intranasal route works well with patients with altered mental status or combativeness, and/or when the Paramedic is in a moving ambulance. Several drugs can be administered intranasally. The clear advantage of intranasal administration of drugs is the decreased risk of accidental needle injury.
• Naxolone is a drug used for suspected opioid overdoses. The use of naxolone intranasally is considered "off-label use," meaning the FDA has not approved the drug for use in this manner. The volume administered intranasally should be no more than 1 mL of liquid, and the drug should be atomized to a particle size of between 10 mcg and 50 mcg, the optimal particle size for absorption.
• The inhalation of medications is the inhalation of drug-laden vapors into the bloodstream via the respiratory route. Pulmonary treatments focus on the delivery of respiratory agents directly into the pulmonary tree. The common drawback to both these methods is the dependence on the patient’s respiratory function.
• As air enters the lungs, it meets resistance as the structures narrow. The resistance slows the air down; by the time it reaches the alveoli, it is nearly still. This encourages fallout, as large particles carried in the air settle out as the velocity is lost. The result is that nearly particulate-free air enters the alveoli. This works against large droplets of aerosolized medications and reduces the effectiveness of many respiratory drugs.
• The metered dose inhaler (MDI) is a portable and well-accepted respiratory treatment platform. However, it is relatively ineffective, depositing less than 20% of the medication in the distal lung fields. A spacer device can be used to increase MDI’s effectiveness. Dry powder inhalers (DPI) use a pulverized solid drug for inhalation with a delivery device similar to an MDI. Again, the effectiveness of the medication depends on the patient’s inspiratory effort.
• By suspending the medication in a stream of air, the small volume nebulizer (SVN) is thought to produce a better particle size for inhalation (about 1 to 3 microns). Prior to using an SVN, the Paramedic should conduct a history to determine the patient’s responsiveness to MDI bronchodilators. He should also perform a physical, auscultating for wheezes or absent breath sounds. Key to assessing the effectiveness of any SVN treatment is the patient’s subjective judgment regarding her own dyspnea. For intubated patients, a SVN may be attached in-line with the bag-valve-mask assembly.
• Topical medication absorption into the subcutaneous capillary beds, or transdermal medicine, offers a drug administration route that can have sustained systemic delivery of a medication. Medications given via a transdermal patch can include nicotine, hormone replacement, opiate analgesics, and nitroglycerine.
• The components of a hypodermic syringe include the syringe and the needle, often connected via a luer lock or slip-tip adaptor. Syringes are labeled according to the volume within the barrel (e.g., 1, 3, 5 mL) and the calibrations on the side of the barrel. The exception is insulin syringes, which are labeled in international units (IU). Surface tension and adhesion of water to the walls of the syringe form a meniscus. The volume of the drug in the syringe is determined by comparing the bottom of the meniscus with the calibration on the barrel.
• The needle is the second component of the hypodermic syringe. Measured in gauges, the smaller the number means the larger the diameter of the needle (e.g., 14 gauge > 20 gauge). The Paramedic should choose a needle size dependent on the viscosity of the fluid and speed of delivery. Injecting a drug into a medication port of an intravenous set, or performing an intramuscular, subcutaneous, or intradermal injection, all require a specific size and length needle.
• Retractable needles, self-sheathing needles, needles that have a retractable hard case that is advanced over the needle as the needle is withdrawn, and hooded needles that have a protective covering over the needle are all efforts made through engineering controls to help prevent needlestick injury.
• It is every Paramedic’s responsibility to safely dispose of used/contaminated needles into a safe sharps container. The sharps container should be close at hand, within arm’s reach, and be easy to access.
• Medications are packaged in either vials or ampoules. There are prefilled ampoules/syringe systems as well as glass ampoules that have to be broken before the medication can be withdrawn. When withdrawing air from a vial, it is essential that the Paramedic first inject air, in equal volume, into the vial before withdrawing the medicine to prevent a vacuum.
• There are many routes of injection that deliver a drug directly into the target organ. Indirect parenteral injections are also effective means of delivering medications. However, the greatest drawback is its dependence on adequate circulation to reach the target organ.
• Positioning the patient is the first step in preparation for an injection. The injection site selected should not be hard, swollen, or tender and must be free of rashes, moles, birthmarks, burns, scars, or broken skin. The Paramedic should place an isopropyl-soaked pad on the site and, working outward in ever-expanding circles, prepare an area approximately twice the length of the needle. The skin is stabilized with the Paramedic’s nondominant hand and, with the needle in the dominant hand, the needle is inserted under the skin. With the needle in place, the Paramedic would gently aspirate to ensure that the needle was not inadvertently placed into a vein.
• Intradermal injections may be used when preparing an intravenous site with a local anesthetic or for tuberculosis testing. The objective of an intradermal injection is to place a small quantity of medicine just under the epidermis and in close proximity of the subcutaneous tissue. Point of care blood testing can be performed with blood glucose analysis or field troponin levels. A finger stick or, for pediatric patients, a heel stick is performed to obtain a small sample of blood for analysis.
• Subcutaneous injection of medication is the slowest and least dependable means of obtaining therapeutic drug levels in the bloodstream. Acceptable sites for subcutaneous injections including the abdomen, the lateral aspects of the upper arm, and the anterior thigh, as well as the ventrodorsal gluteal area. Frequent subcutaneous injections at one site, such as may occur with repeated insulin injections, result in tissue fibrosis.
• Intramuscular injection deposits the drug between the layers of the muscle, and below the subcutaneous tissue, providing rapid systemic action. Intramuscular injections are contraindicated in patients with peripheral vascular disease and disease states which create hypoperfusion (e.g., anaphylactic shock). Intramuscular injection is a preferred route for so-called depot medications deposited under the skin to produce sustained therapeutic levels over a longer period of time.
• There are four common sites for intramuscular injection. The first site, the ventrogluteal (VG) muscle, is located on the lateral thigh proximal to the hip. A more anterior injection site is the middle portion of the vastus lateralis (VL) muscle of the thigh. Requiring less exposure and easier access is the deltoid muscle. The most common intramuscular injection site is the dorsogluteal (DG) muscle. The gluteus is located proximal to the inferior portion of the patient’s flank.
• EMLA cream, a topical anesthetic, can be used to reduce the pain of needle insertion. Fluori-methane and vapocoolant spray are also applied directly to the skin for anesthetic effects. The deeper muscle layers are relatively free of pain receptors, although irritation may occur from a drug if leaked into subcutaneous tissues. To prevent this, the airlock and Z-track techniques may be used by the Paramedic for intramuscular injections.
• The elderly and children each present a special challenge to the Paramedic who must perform an injection. To develop strategies to improve success of a pediatric injection, the Paramedic must take into account the child’s developmental stage and adjust the approach accordingly. For the elderly, the combination of age and poor nutrition reduces muscle mass, limiting available injection sites.