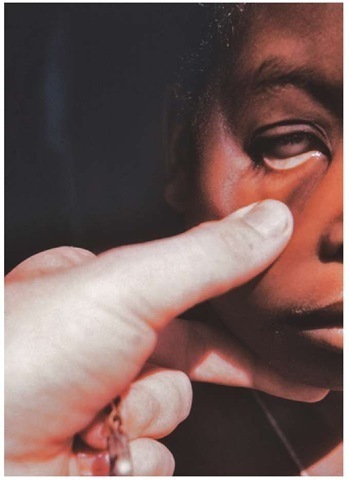
Skin Condition and Color
Skin condition and color is an important indicator of the patient’s ability to provide sufficient oxygen-rich blood to the tissues. While there is a wide range of normal skin tones, normally many fair skinned individuals will have a pink color or tone to the skin. The Paramedic may need to assess the color of the mucous membranes in the mouth, the palms of the hands and soles of the feet, or the conjunctiva (Figure 16-16) in darker skinned patients to determine skin color. Skin condition is generally categorized as normal, dry, moist, or diaphoretic. A patient with diaphoretic skin is sweating profusely. This state is associated with many different conditions.
Pain
As previously discussed, assessment of pain was considered the fifth vital sign by the Joint Commission on Hospital Accreditation in the late 1990s in an effort to strongly encourage all healthcare providers to adequately assess every patient for pain and reassess the patient after interventions.22,23 Various pain scales have been developed in an attempt to quantify the amount of pain. However, pain assessment is still a subjective report that varies between patients. A more detailed
Figure 16-15 Measuring temperature with a tympanic thermometer.
Figure 16-16 Assessing the conjunctiva for pallor that may indicate anemia or blood loss.
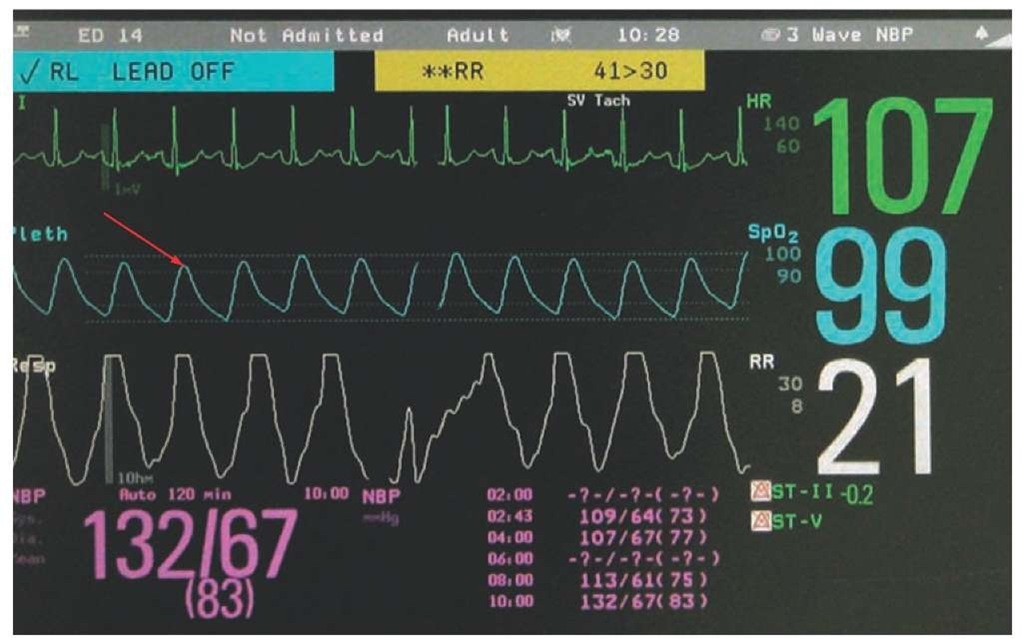
Pulse Oximetry
Hemoglobin is the molecule in red blood cells that accepts oxygen in the lungs and carries it to the body’s tissues to allow cellular respiration. Pulse oximetry is a noninvasive measurement of the percentage of hemoglobin in arterial blood that is bound to oxygen molecules.24 An accurate reading provides the Paramedic a good measure of the patient’s oxygenation, or his ability to move oxygen from the air in the lungs into the blood. It does not provide an indication of how well the patient is using that oxygenation. It also does not provide an indication of the patient’s ventilation, or note how well the patient is moving air in and out of the lungs during inhalation and exhalation. A normal pulse oximetry value in a healthy individual without lung disease is between 96% and 100% saturation. For individuals with chronic lung diseases, the patient’s personal normal pulse oximetry may actually be as low as 85% without supplemental oxygen.25
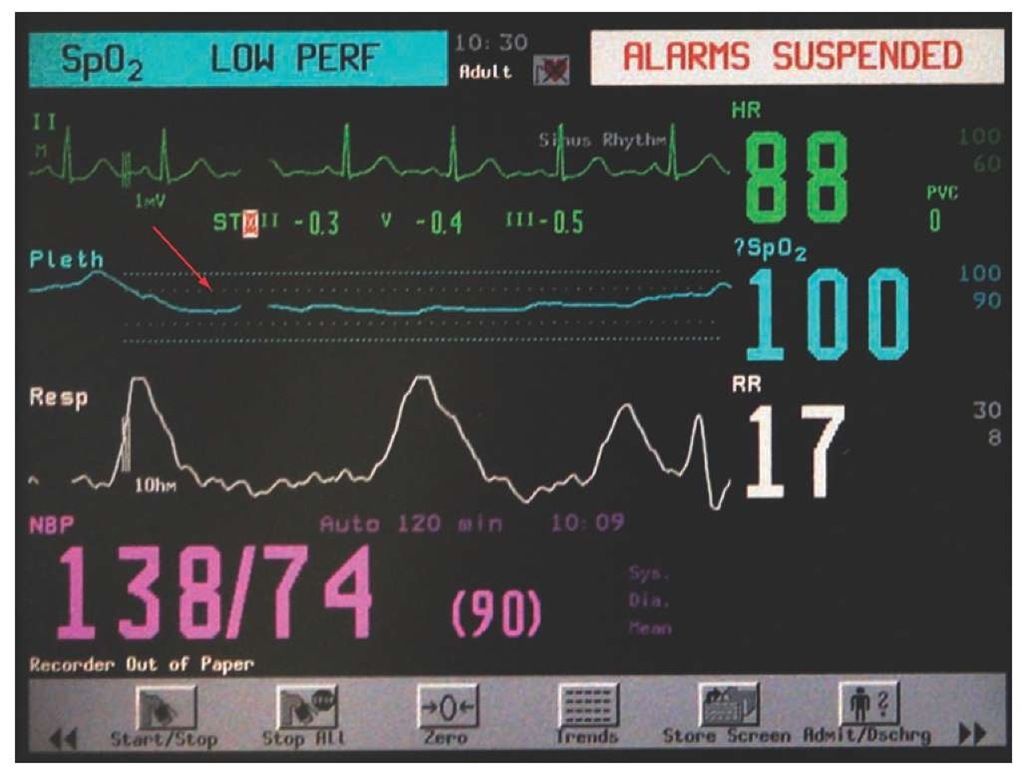
Pulse oximetry is determined by measuring the change that occurs when a beam of red light and infrared light is directed across a capillary bed. When hemoglobin binds to oxygen, it will cause an imperceptible change in the red and infrared light as it passes through the pulsating capillary bed. This change is translated into a percentage of oxygen saturation that is displayed for the Paramedic. Some pulse oxime-ters provide a waveform display in addition to the numerical value (Figure 16-17). This waveform fluctuates with changes in the patient’s blood flow during normal contraction of the patient’s heart. Because it is simple to measure the rate of these fluctuations, most oximeters will provide the patient’s pulse rate in addition to the oxygen saturation.
Figure 16-17 Normal pulse oximetry waveform. Notice the fluctuations that correspond with the patient’s pulse rate (red arrow).
Figure 16-18 Poor oximetry waveform (red arrow).
Several factors may affect the accuracy of the pulse oximetry reading. In order for the reading to be accurate, the patient must have sufficient blood flow in the capillary bed of the body part where the probe is attached. If the waveform is poor (Figure 16-18), then the oximeter will either not read or will provide an inaccurate reading. Blood flow to the capillary bed is decreased if the limb is cool, if the patient is hypovolemic (decreased circulating blood volume), or the patient is hypotensive. Traditional pulse oximeters only detect whether or not the hemoglobin is bound to another molecule. Other compounds (e.g., carbon monoxide) can also bind to hemoglobin in the red blood cells. If carbon dioxide is present, the pulse oximeter will still read a normal saturation level, even though the patient’s tissues do not receive sufficient oxygen and are hypoxic.26 Newer co-oximeters utilize additional wavelengths of light and can detect the presence of carbon monoxide and other compounds that can bind to hemoglobin.
It is important to note that even patients who present with a pulse oximetry reading within a normal range can benefit from supplemental oxygen. In many conditions, the surface capillary beds utilized to measure oxygen saturation may have fully saturated blood; however, due to blood loss or hypotension, deeper vessels—including those supplying the heart, brain, kidneys, and the intestines—may not have an adequate supply of oxygen. Blood itself not only carries oxygen by hemoglobin in red blood cells, but can also carry dissolved oxygen molecules within the plasma, or liquid portion of the blood. Patients who are in respiratory distress or suffering from a significant illness or injury should receive supplemental oxygen to ensure the organs continue to receive a sufficient amount of oxygen.
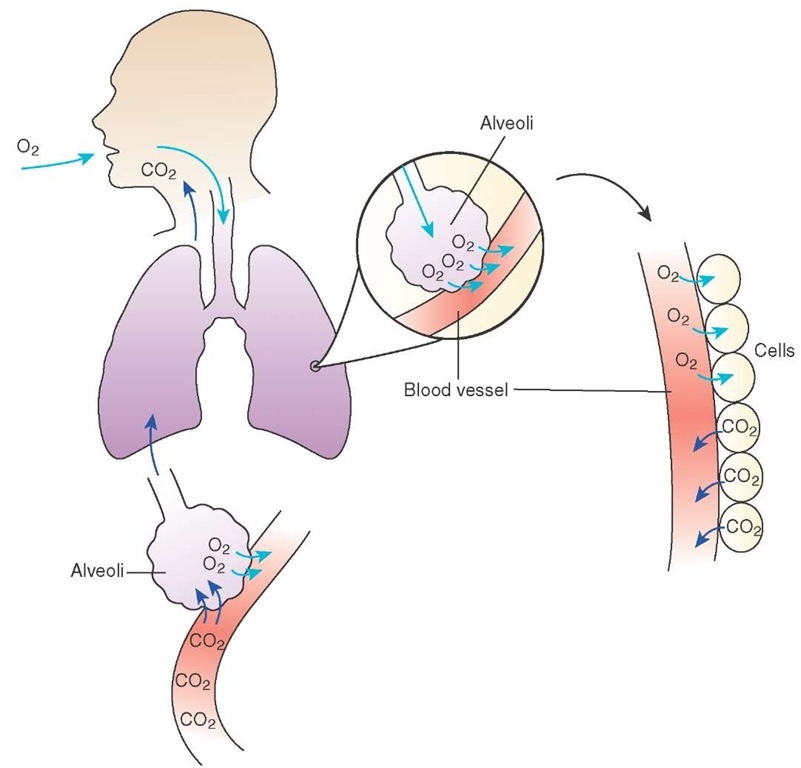
Capnography
The process of respiration includes the following steps (Figure 16-19):
■ Inhalation of oxygen-containing air into the lungs
■ Movement of oxygen from the air across the alveolar membrane into the blood
■ Movement of oxygen through the blood to the tissues
■ Absorption of oxygen into the cells
■ Production of carbon dioxide by the cells as they use the oxygen and glucose for fuel
■ Delivery of carbon dioxide back to the lungs
■ Movement of the carbon dioxide back across the alveolar membrane into the lungs
■ Exhalation of the carbon dioxide into the atmosphere.
From a respiratory system standpoint, the amount of exhaled carbon dioxide is related to the patient’s ability to move air in and out of the lungs. If the patient cannot ventilate adequately, the concentration of exhaled carbon dioxide will increase because the patient exhales a smaller amount with each breath, allowing the carbon dioxide level to build up in the lungs. If the patient hyperventilates, the exhaled carbon dioxide level will decrease because a larger amount of carbon dioxide is exhaled with each breath, decreasing the overall concentration of carbon dioxide in the lungs. In situations where the patient is able to circulate the blood adequately, capnography provides an indication of how well the patient is able to ventilate.
From a circulatory standpoint, the amount of exhaled carbon dioxide is directly related to the body’s ability to perfuse the tissues, or carry oxygen, glucose, and other nutrients to the cells in order to carry on the metabolic processes required to sustain life.27 If the patient is perfusing well, the carbon dioxide produced by the metabolic processes inside the cells will be transported back to the lungs for exhalation. Conditions that decrease the patient’s ability to circulate the blood (e.g., shock and cardiac arrest) will decrease the level of carbon dioxide in the lungs.
Figure 16-19 The process of respiration.
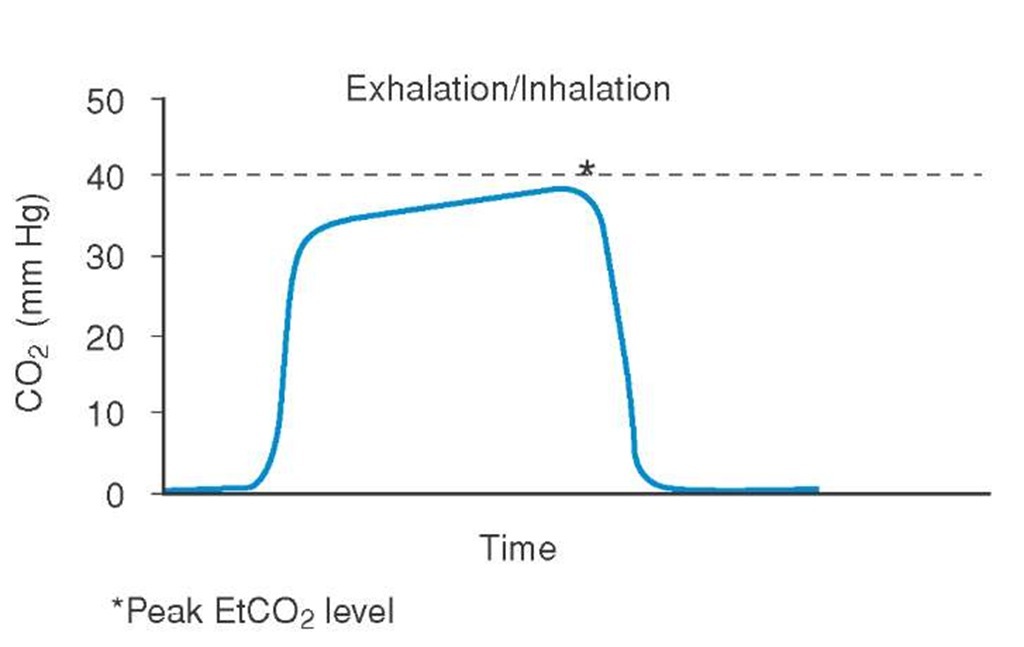
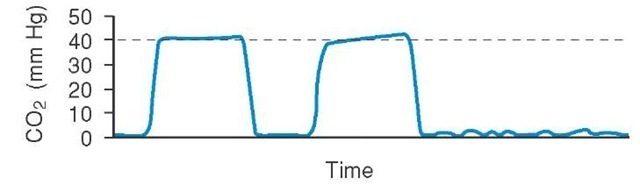
Waveform capnography provides a graphical representation of the exhaled carbon dioxide level over time.28,29 The level of carbon dioxide will vary with inhalation and exhalation (see the curve shown in Figure 16-20). The normal level of exhaled carbon dioxide is approximately 40 mmHg. End-tidal carbon dioxide levels (EtCO2) below 10 mmHg in the setting of cardiac arrest is associated with a 0% chance of survival. Elevated levels are seen in patients who are not ventilating adequately. A decrease in EtCO2 level during mechanical ventilation may indicate the patient has become hypotensive. It could also mean the ventilation rate is too high and should be slowed to a lower rate. The waveform’s shape and pattern can provide clues to the disease process in patients complaining of shortness of breath. Finally, using EtCO2 with patients who are intubated is an excellent patient safety tool, as the Paramedic can immediately detect a dislodged endotracheal tube by the change in waveform before the patient’s oxygen saturation is affected (Figure 16-21).
Figure 16-20 Typical capnography waveform.
Orthostatic Vital Signs
Orthostatic vital signs are vital signs that change with position. When an individual changes position from lying down to standing, the blood pressure normally has a tendency to drop due to gravity.
Figure 16-21 Sudden loss of the waveform in an intubated patient likely indicates endotracheal tube dislodgement.
The body will compensate initially for this drop in blood pressure by constricting the arterial sys-tem.33 If that does not provide sufficient compensation, then the heart rate will increase in an effort to maintain an adequate blood pressure. If the patient has a decreased blood volume, whether through hemorrhage or through dehydration, the body will not be able to completely compensate for this change by decreasing the size of the blood vessels alone. Therefore, measuring orthostatic vital signs can assess the patient for subtle volume loss that may not be evident during a supine or a seated set of vital signs. To measure orthostatic vital signs, the Paramedic measures the blood pressure and heart rate in the supine, sitting, and standing positions with at least one minute rest between position changes to allow the body to compensate for the change. Although this may be difficult to achieve in the prehospital environment, it is inadvisable with patients who have sustained sufficient trauma to require spinal motion restriction.
Positive orthostatic vital signs are defined as a heart rate increase of 20 beats per minute or greater, a systolic blood pressure drop of greater than 20 mmHg, a diastolic blood pressure increase of 10 mmHg, and/or dizziness or lightheadedness with position change.34,35 While ortho-static vital signs have been traditionally used as a means of determining blood loss or hypovolemia in patients who had otherwise normal vital signs, other factors—including medication, age, ingested substances (e.g., alcohol), and other medical conditions—can also produce orthostatic changes. In several studies specifically looking at blood loss, changes
STREET SMART
Two Paramedics should take orthostatic vital signs. One Paramedic remains dedicated to watching the patient. Any change in level of consciousness, ability to remain in the necessary position, or complaint of new or worsening symptoms is enough for the first Paramedic to cancel the remainder of the orthostatic vital signs. The second Paramedic is dedicated to measuring the pulse and blood pressure.
in pulse rate with position change could reasonably detect blood loss of between 500 mL and 1 L.36 Care must be taken when measuring orthostatic vital signs on a patient, especially when assuming the standing position. If the patient develops severe symptoms on changing position, measurement should not be completed, as it puts the patient at risk for fall and injury.
Concern-Based Physical Exam
Conceptually, every call for assistance begins with a patient’s chief concern or complaint. This is true whether the call was received emergently through the 9-1-1 system or non-emergently through a secondary system. From a dispatch perspective, the algorithms used to determine response resources are keyed from the patient’s or caller’s chief concern. From a Paramedic perspective, the chief concern is used to help focus the history and physical examination to find the most likely cause of the patient’s chief concern and detect life- or limb-threatening conditions that are associated with that condition. Detailed physical examinations are time-consuming and often provide more information than what is useful to the Paramedic. During most patient contacts, the Paramedic will perform a focused physical exam based upon the patient’s chief concern.
Focused Exam Matrix
In the prehospital environment, detailed head to toe exams are not practical for many patients. Instead, a focused physical exam is performed on the systems associated with the patient’s chief concern. The Paramedic performs a detailed examination of one or two related body systems and a brief examination of other relevant body systems. In this way, the Paramedic can efficiently use her time during the patient contact and assess for findings that can help confirm the paramedical diagnosis suspected by the history or suggest alternate conditions that require assessment.
The physical examination is also guided by the complexity of the patient’s chief concern. A patient who is complaining of ankle pain after twisting his right ankle on the sidewalk and did not strike any other part of his body may be appropriate for a single system-focused exam on that ankle. A patient with a strong cardiac and respiratory history complaining of general weakness may require a more extensive physical examination. The discussion throughout the rest of the topic will provide a guide to the elements of the physical examination that should be covered based upon the patient’s chief concern. It is not meant to be all inclusive, and should be modified by the Paramedic based upon clinical judgment, the specific patient’s presentation, and examination findings that suggest other conditions that may contribute to the chief concern.
Both the focused and detailed physical examinations take place after correcting life-threatening conditions that were discovered during the primary assessment. Some of the items assessed during the focused or detailed examinations are items that were assessed during the primary assessment.
Table 16-5 Physical Examination by Chief Concern (CC)
|
Chief Concern |
Primary System |
Secondary System |
Tertiary System |
|
Chest pain |
Cardiovascular |
Respiratory |
Neurological |
|
Gastrointestinal |
|||
|
Shortness of breath |
Respiratory |
Cardiac |
Neurological |
|
Abdominal pain |
Gastrointestinal |
Cardiac |
|
|
Loss of consciousness |
Neurological |
Cardiac |
Musculoskeletal |
|
Altered mental status |
Neuorological |
Psychiatric |
|
|
Musculoskeletal |
Musculoskeletal |
Skin |
|
|
Psychiatric |
Psychiatric |
Neurological |
They should be reassessed during the focused exam as necessary to provide the Paramedic with the information needed to efficiently and adequately treat the patient.