Respirations
Respirations are assessed by observing the respiratory rate, depth, pattern, and work of breathing. The respiratory rate is assessed by watching chest rise or auscultating breaths with a stethoscope and counting the number ofbreaths (Figure 16-9). The normal adult respiratory rate at rest is between 12 and 24 breaths per minute. The respiratory rate can be determined by counting the number of respirations in either a full minute or the number of respirations in 30 seconds and multiplying that count by two. In general, the respiratory rate is best counted when the patient is not aware that the Paramedic is counting the rate. In contrast to the pulse rate, a patient can control his respiratory rate much easier than his pulse rate (Table 16-2).
Figure 16-9 Paramedic assessing a patient’s respirations.
Table 16-2 Normal Respiratory Rate by Age
|
Patient Age (yr) |
Breaths/Minute |
|
Infant (birth-1) |
Initially 40-60; rate drops to 30-40 after a few minutes; slows to 20-30 by 1 year |
|
Toddler (1-3) |
20-30 |
|
Preschooler (3-5) |
20-30 |
|
School-ager (6-10) |
15-30 |
|
Adolescent (11-14) |
12-20 |
|
Young or middle-aged adult (15-64) |
12-20 |
|
Older adult (65+) |
Depends on patient’s health |
Along with the rate, the Paramedic should note the depth of respiration. The depth can be described as shallow, normal, or deep. A shallow respiration is less than the normal chest excursion and typically produces an inadequate respiration. Another term used to describe shallow respirations is hypoventilation. Hypoventilation can be caused by drug overdose, head injury, or other conditions that can cause coma. A deep respiration is deeper than normal and is termed hyperventilation. Examples of conditions that can cause hyperventilation include respiratory distress, a metabolic condition, or drug overdose.
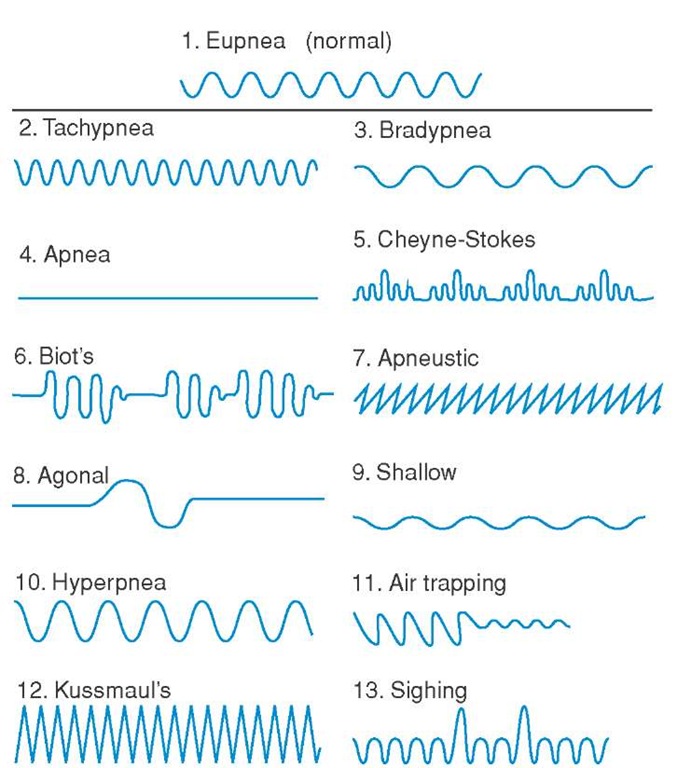
The respiratory pattern is considered the rhythm of the respirations. The respiratory pattern is the combination of the timing of the respirations and the depth of respirations (Figure 16-10). Different causes exist for many of these abnormal patterns (Table 16-3).
STREET SMART
The Paramedic should be prepared to assist ventilations whenever a patient is either hypoventilating or hyperventilating, as both of these respiratory situations can represent ineffective ventilation.
Figure 16-10 Abnormal respiratory patterns.
Table 16-3 Selected Abnormal Respiratory Patterns, Their Description, and Cause
|
Pattern |
Description and Cause |
|
Cheyne-Stokes |
Gradually increasing rate and tidal volume, which increases to a maximum, then gradually decreases; occurs in brain stem injuries |
|
Biot’s |
Irregular pattern and volume, with intermittent periods of apnea; found in patients with increased intracranial pressure |
|
Agonal |
Slow, shallow, irregular respiration; results from brain anoxia |
|
Kussmaul’s |
Deep gasping respirations, representing hyperventilation, "blowing off" of excess carbon dioxide and compensation for an abnormal accumulation of metabolic acids in the blood; though possible in any patient with metabolic acidosis, best known with diabetic ketoacidosis |
|
Central neurogenic hyperventilation |
Deep, rapid, regular respiration; found in patients with increased intracranial pressure |
Figure 16-11 Signs of increased work of breathing. (a) Accessory muscle use. (b) Sternal retractions. (c) Rib retractions. (d) Tripod position. (e) Pursed lip breathing.
The patient’s work of breathing is also assessed to measure the level of respiratory distress. There are several signs that indicate an increased work of breathing. During normal respiration, the chest expands effortlessly. When a patient is in respiratory distress, more effort is required to breathe and accessory muscles are recruited to help expand the rib cage, allowing the patient to inhale. When these muscles are used, they tend to become more defined (Figure 16-11a). When the work of breathing increases, more effort is needed to generate the negative pressure in the thorax required for inspiration. When this happens, the skin at the top of the sternum and the skin between the ribs are pulled inwards because of this negative pressure in the chest. These findings are termed sternal retractions (Figure 16-11b) and rib retractions (Figure 16-11c), respectively. Patients in respiratory distress also will position themselves in a way to help improve breathing. The tripod position (Figure 16-11d) is a sign that the patient is in severe respiratory distress. This position allows the overworked accessory muscles to work better, although most patients begin to tire when they are in such severe respiratory distress. Pursed lip breathing (Figure 16-11e) is another sign of increased work of breathing. When the exhalation pressure is high, the alveoli tend to collapse during exhalation. The patient puckers his or her lips while exhaling, providing some resistance to exhalation that provides pressure to keep the alveoli open.13-16
Blood Pressure
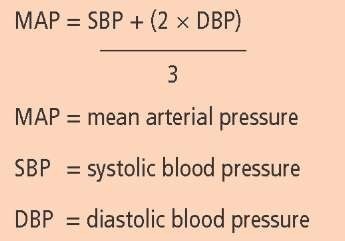
Blood pressure is a measure of the pressure within the blood vessels that make up the circulatory system. The pressure will vary depending upon the type of vessel and the phase of heart contraction. When the Paramedic measures blood pressure, he is measuring the pressure within the arterial system. Blood pressure is measured at its maximum and minimum. The maximum blood pressure is measured during systole when the heart contracts, and is called the systolic blood pressure. The minimum blood pressure is measured during diastole when the heart relaxes and fills, and is called the diastolic blood pressure. These two levels of blood pressure are generated by the heart’s intermittent contractions. Blood pressure can also be reported as a single pressure, the mean arterial pressure (MAP), which is the average pressure in the arterial system over time (Figure 16-12). A typical mean arterial pressure that will maintain adequate cerebral perfusion is about 60 to 80 mmHg.17 An adequate blood pressure is necessary for adequate perfusion of the body’s organs; however, a chronically elevated blood pressure can lead to increased risk of catastrophic cardiovascular events.
The pulse pressure is defined as the difference between the systolic and diastolic pressures. The pulse pressure can provide the Paramedic with an indication about the blood volume status or compensation for illness in a given patient.
Figure 16-12 Computing mean arterial pressure (MAP). Many automated noninvasive blood pressure monitors automatically calculate and display MAP.
Both the arterial and venous blood vessels have elasticity and change vessel diameter in response to changes in fluid volume, pressure, and pathological conditions, with the arterial system much more elastic than the venous system. Younger patients can compensate for changes in pressure and volume status because of the increased elasticity of their blood vessels. The pulse pressure in an adult at rest is normally approximately 40 mmHg. Conditions that affect cardiac output, the volume of blood pumped out of the left ventricle in one minute, can cause a decreased pulse pressure. In general, the dia-stolic pressure holds relatively steady or drops slightly, while the systolic pressure drops more than the diastolic pressure. Conditions that cause a drop in blood fluid volume (e.g., hemorrhage or shock from other causes) can cause a widening of the pulse pressure, especially in younger or otherwise fit patients.18 Those patients may be able to initially sustain a near normal or slightly decreased systolic pressure. However, when the heart relaxes, the diastolic pressure is significantly less than normal for that patient. Pulse pressure may provide the Paramedic with an early clue to shock in patients who otherwise appear to be stable.
To properly measure blood pressure, the patient’s arm should be positioned at the level of her heart. Support the patient’s arm at mid-chest level and center a properly sized cuff over the brachial artery of the arm (Figure 16-13). The blood pressure can be measured by either palpation or by auscultation. When measuring the blood pressure by palpation, the radial pulse is palpated by the Paramedic while inflating the blood pressure cuff. The Paramedic inflates the blood pressure cuff approximately 10 to 20 mmHg above the loss of the pulse, and then slowly deflates the cuff until the pulse returns. The point where the pulse returns is the systolic pressure. When reporting a blood pressure measured by palpation, the Paramedic verbally reports the pressure "by palpation" (for example, "124 by palpation") and records the systolic pressure as a fraction with a P as the denominator (e.g., 124/P). The palpation method is useful in situations where there is a lot of ambient noise that would make it difficult to auscultate the blood pressure.
The auscultation method is a more accurate method of measuring blood pressure. The Paramedic places the blood pressure cuff on the patient’s arm as previously described and places the diaphragm of the stethoscope over the brachial artery (Figure 16-14).19 The Paramedic inflates the cuff until the sound of the heartbeat disappears and inflates the cuff an additional 10 to 20 mmHg. Next, the Paramedic slowly deflates the cuff at a rate of approximately 2 to 3 mmHg per second and notes the pressure at which she hears the sounds of at least two consecutive beats. This is the systolic blood pressure. The Korotkoff sounds heard during the inflation and deflation of the cuff are caused by the change in the nature of blood flow though the artery.20,21 To obtain the diastolic blood pressure, the Paramedic continues deflating the cuff slowly, until she notes a muffling and then a disappearance of the Korotkoff sounds. This is the diastolic blood pressure. The Paramedic records both systolic and diastolic blood pressure readings to the nearest 2 mmHg.
Figure 16-13 Proper placement of a blood pressure cuff helps ensure accurate measurement.
Figure 16-14 Measuring the blood pressure by auscultation.
Blood pressure readings vary significantly with patient age, underlying physical and medical conditions, and current medications. A systolic blood pressure that is above the upper limit of normal indicates hypertension. A systolic blood pressure below the lower limit of normal indicates hypotension. In an adult, a blood pressure greater than 139 mmHg systolic or 89 mmHg diastolic are always considered abnormally elevated and a systolic pressure below 90 mmHg is considered abnormally low (Table 16-4).
Table 16-4 Normal Blood Pressures
|
Blood Pressure (mmHg) |
|
|
|
Patient Age (Years) |
Systolic |
Diastolic |
|
Infant and toddler (0-3) |
80 + (2 times age in years) |
Two-thirds systolic |
|
Preschooler (3-5) |
78-116 |
average 55 |
|
School-ager (6-10) |
80-122 |
average 57 |
|
Adolescent (11-14) |
88-140 |
average 59 |
|
Young and middle-aged adult (15-64) |
90-150 |
60-90 |
|
Older adult (65+) |
Depends on patient’s health |
Depends on patient’s health |
Temperature
The body’s normal core temperature ranges from 36.1°C to 37.7°C (97°F to 99.8°F). A temperature above 38°C (100.4°F) is considered a fever. An elevated body temperature is called hyperthermia. In contrast, hypothermia is defined as a body temperature less than 35°C (95°F). Relatively accurate estimates of core temperature can be obtained from oral, rectal, or tympanic thermometers (Figure 16-15), with the rectal temperature as the most accurate estimate of the core body temperature.