Adjusting the Infusion Rate
Before starting any infusion, it is important that the Paramedic review the indications for the infusion as well as the contraindications. A reassessment of the patient’s vital signs, jugular venous distention, and lung sounds should be made. Then the Paramedic should check for signs of pulmonary edema to establish a baseline.
The selection of an intravenous administration, in part, determines the rate of infusion. For example, a micro-drop administration set cannot produce the same volume of flow in mL per hour, even when the fluid is running as a straight stream, that a macro-drip administration set can.
Conversely, it is more difficult to dispense a precise volume for infusion using a macro-drop intravenous administration set. For this reason, Paramedics use micro-drop intravenous administration sets as a standard practice for medication infusions to help ensure that the exact dose is administered. When a precise volume of infusion is needed, the Paramedic would suspend the solution ("hanging the bag") from a hook-like device called a hanger. The Paramedic gradually releases the roller clamp, counting the drops in one minute to equal the desired flow rate. EMS drug infusion rates are influenced by a number of physical factors which are part of the reality of practice in the field and can alter the drip rate.
To control the drip rate, the roller clamp or screw clamp applies pressure against the tubing to offset the pressure within the tubing, thus increasing or decreasing flow accordingly. The pressure within the tubing is a function of the height of the column of fluid and the diameter of the tubing.
Many factors can influence the rate of flow, such as the friction loss within the tubing, the diameter of the tubing, the viscosity of the fluid within the tubing, and the length of the tubing. Assuming that all these variables remain constant, the lone act of raising or lowering an intravenous bag—for example, to go through a door or enter an ambulance—will alter the height of the column of fluid. Therefore, the pressure within the tubing is affected, and that will in turn change the drip rate. This all happens without adjusting the roller clamp. Once a drip rate has been established, it is important to try to constantly maintain the intravenous bag at the same height.
Even with the best efforts of the Paramedics involved in a patient’s care, other factors that cannot be as easily controlled will influence a drip rate. For example, cold fluids run through an IV access tend to cause vasospasm in the affected vessel. Efforts to warm fluids can help prevent this occurrence. However, warming an intravenous fluid to room temperature still means that chilled (less than body temperature) fluid is being infused.
Temperature changes, which are not common in the hospital setting, are a fact of life for the Paramedic. Intravenous tubing exposed to cold temperatures, such as occurs when transferring a patient to the ambulance in sub-zero degree weather, will stiffen the IV tubing and alter the tension applied by the roller clamp, as well as change the viscosity of the fluid within the tubing. Even when the patient is safely secured within the ambulance’s temperature-controlled patient compartment, other factors (such as turbulence at the end of a catheter or slack in an armboard) can cause the IV catheter to migrate up against a valve or the wall of the vein, occluding the flow.
With all of these variables in mind, it is important that a Paramedic regularly confirm, and then re-confirm, the drip rate, particularly if a medicated solution is being infused. Minimally, a drip rate should be rechecked after the patient is placed in the ambulance and then upon arrival at the hospital. Preferably, the drip should be checked with every set of vital signs. Out-of-control drip infusions, called runaway infusions, can have serious implications. A runaway infusion of a medicated solution results in the patient being overmedicated. As is the case with any overdose, a runaway infusion must be reported to medical control so that appropriate measures can be taken to mitigate the medication’s adverse effects and negative impact.
The value of prehospital intravenous infusions for trauma patients is being debated. Early consensus seems to indicate that a minimal infusion, one that maintains end-organ perfu-sion (i.e., a minimal systolic pressure of approximately 80 to 90 mmHg), should be established.37,38 A runaway infusion during trauma resuscitation can adversely affect the patient in multiple ways, including increasing intracranial pressure, diluting coagulation factors, and increasing hemorrhagic losses.39 A runaway infusion can be just as devastating for the medical patient as well. A runaway infusion can quickly volume overload the patient with kidney or heart failure. Subsequently, the patient can experience hypertension, pulmonary edema, or cerebral swelling.
Mechanical Flow Control Device
Paramedics use mechanical flow control devices to more accurately control intravenous flow of any drug infusions which are caustic, viscous, or have vasoactive medications. Several types of flow control devices are available on the market. Some work by a venturi effect, controlling the flow by adjusting an aperture, described as dial-a-flow devices. Others work by placing pressure on the tubing, either through a rotary piston or a linear compression (such as massaging fingers), and "milking" the tubing at a precise rate. Smaller syringe pumps apply pressure to the plunger in precise pulsations to inject the drug into the fluid stream.
The advantage of all of these devices is that they can more accurately control flow (Figure 27-23). Many are also equipped with air-in-line alarms, indicating a break in the closed intravenous system, and fluid empty alarms as well as obstruction alarms. The greatest advantage of these flow control devices may be the margin of safety that they bring to the less-controlled environment of out-of-hospital emergency medicine. While not impossible, the risk of a runaway infusion is virtually eliminated by these devices. On the downside, the costs of flow control devices, including the costs of training Paramedics in their proper use, may be prohibitive.
Figure 27-23 Flow control device.
Secondary Intravenous Infusions
If a continuous infusion is running and an intermittent infusion of a medicated solution is needed, the Paramedic can establish a secondary infusion, or piggyback infusion, to the primary infusion. This practice has several advantages, including the ability to immediately terminate the intermittent infusion (e.g., if the patient had an allergic reaction) and permit a bolus and/or drug to counteract any ill effects, such as anaphylaxis-induced hypotension. Use of a secondary intravenous infusion also eliminates the need for a second IV access and the accompanying difficulty, and time, of preparing and establishing an intermittent infusion device (saline lock) which would normally be necessary.
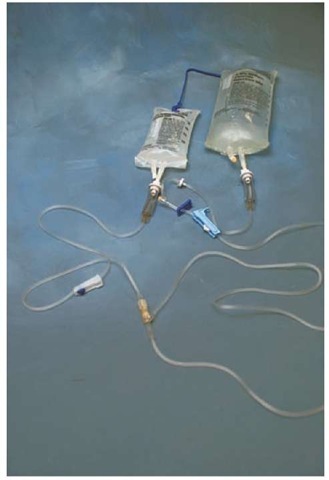
After assessing to ensure that the primary infusion is running and that the IV access is patent, the Paramedic would prepare the secondary IV. Special secondary administration sets which have a shorter length are available (Figure 27-24). The secondary set would be run out as per the procedure described previously for a continuous infusion administration set. The secondary intravenous set would be connected to the continuous intravenous set, now called the primary infusion, via a medication port. If a needle is used to attach the two sets, it will be necessary to first cleanse the port with an alcohol prep pad.
Figure 27-24 Secondary intravenous administration set.
With the two administration sets now attached, the primary set is placed lower than the secondary set. This is usually accomplished by using a plastic or metal hanger that comes with the secondary administration set. The secondary administration set will now take dominance over the primary administration as its fluid column is higher and thus there is more pressure. When the column of fluid in the secondary administration set equals the level of the fluid in the primary administration set’s drip chamber, then the primary drip will resume flow at its previous adjusted rate.
Intravenous Injection
Paramedics frequently use IV access as a means for the rapid injection of IV medications during an emergency. Early insertion of an intravenous access device during patient care provides Paramedics a nearly instant ability to administer drugs directly into the circulation and to target organs.
If the IV access site has an intermittent infusion device attached, then the Paramedic would attach a syringe and withdraw about 10 mL of fluid from the device and discard the waste into an approved sharps container. The Paramedic would then attach another syringe, either filled or prefilled with the medication, to the infusion device and inject the medication. This process is called IV push. Note that if a needle is used then the self-sealing membrane of the injection port must be cleansed. Immediately after injecting the medication, the device is flushed with 10 to 20 mL of NSS to clear the medication from the device and assure that all of the medication goes into the circulation (Figure 27-25).
Figure 27-25 Saline flush with prefilled syringe.
If the IV access site has a continuous infusion in place, then the Paramedic would first clamp the tubing, using the roller clamp or slide clamp, and then attach the syringe or prefilled ampoule, as just described. Once the IV push is completed, the Paramedic may elect to flush the tubing with 20 mL of NSS and then unclamp the line. He may also choose to unclamp the line and allow a free flow of fluid to flush the IV line for approximately one minute, then re-adjust the flow rate.
If the patient is in cardiovascular collapse, then the patient’s arm should be raised to help the medication drain out of the limb. Similarly, if the patient is in cardiac arrest, then the limb should be raised and a minimum of one minute of external chest compressions performed to ensure that the drug is circulated.
In every case it is important that the Paramedic observe the IV access site for swelling, pain, and other signs of infiltration while injecting the medication. Some Paramedics purposefully place the medication port proximal to the IV access site so that the IV insertion site can be observed. If an infiltration is suspected, then the IV push is stopped and measures taken to counteract the effects of any medication that has leaked into the subcutaneous tissue. It is important to report any intravenous infiltration. If unchecked, some medications (for example, 50% dextrose) can cause severe local tissue necrosis with the potential for subsequent tendon, muscle, and nerve damage.
Obstruction of Intravenous Flow
The flow of an IV may slow, or even stop, for a number of reasons. Before removing the IV catheter, the Paramedic should assess the situation for correctable errors. Starting at the solution bag, the Paramedic would methodically inspect the entire intravenous apparatus. For example, flow will stop if the solution bag is empty, a clamp has slipped, or the tubing is kinked. After assessing the administration set and determining that it is clear of mechanical obstructions, the Paramedic would then turn his attention to the IV access site.
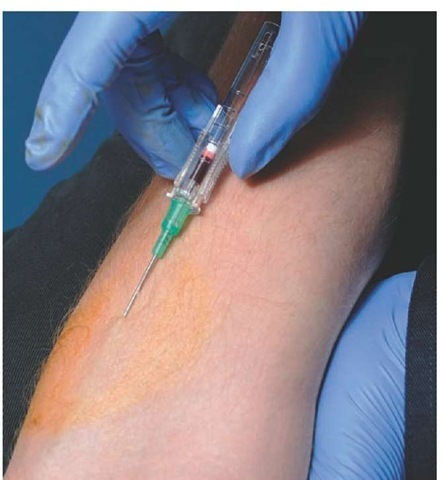
An infiltrated IV access site will eventually slow or stop an infusion. If the IV access site is infiltrated, then the IV catheter must be removed immediately (this process is discussed later in the topic). Finding no visible obstructions or infiltration, the Paramedic may elect to see if there is a return of blood, called a flashback, when the solution bag is lowered below the level of the patient’s heart. A flashback (Figure 27-26) indicates that the IV access remains patent.
Some IV catheters are positional, meaning that the catheter lodged up against the wall of a vein or a valve and the IV flow has been obstructed. To correct a positional IV catheter, the Paramedic may elect to withdraw the needle slightly. This process includes breaking the dressing down or raising the hub of the IV catheter off the skin with a gauze pad. If the IV access is in a joint, it is advisable to place the joint onto a padded splint. If a padded splint is used, then distal circulation, sensation, and movement should be assessed before and after the splint’s application to ensure that the splint is not constrictive. The distal circulation, sensation, and movement should be checked periodically thereafter.
Figure 27-26 Flashback of blood verifies venous competency.
An obstructed IV catheter should never be forcibly injected with solution (IV flush) to remove any obstructions. The risk of forcing a thrombus into the circulation is not equal to the benefit of having an intravenous access. The Paramedic should consider removing the suspect IV catheter and re-establishing a new IV access.
Complications of Intravenous Infusions
Despite the best efforts of Paramedics, local or systemic complications can occur as a direct result of an IV access or infusion. An attentive Paramedic can usually detect these complications and mitigate the circumstances in order to reduce the harm to the patient.
Arteries and nerves tend to be bundled with veins, particularly deep veins. Therefore, they are at risk for accidental needle puncture. An unintentional arterial puncture would be recognized if the Paramedic noticed a pulsating column of blood within the fluid column. However, recognition of an arterial puncture is more difficult in zero flow states, such as cardiac arrest. Careful attention to anatomy, noting the location of proximal arteries by their pulse points, can help decrease the incidence of accidental arterial puncture.
A nerve can also be accidentally punctured during an IV insertion attempt. Patients usually alert the Paramedic immediately following an accidental nerve puncture. The patient will complain loudly of shooting pain, numbness, and tingling in the affected limb. Immediate withdrawal of the offending needle should provide the patient with immediate relief.
Immediately following successful cannulation of a vein by an IV catheter, and frequently thereafter, the Paramedic should assess the IV access for signs of infiltration or infection. Infiltration can occur by several mechanisms puncture of the posterior wall, enlargement of the initial incision site, or displacement of the catheter. Regardless of the mechanism, the IV solution seeps into the interstitial fluid compartment (ICF) (i.e., the third space). The resultant swelling can create increased pressure within a compartment, which can lead to impingement of nerves, muscle damage, and compression of blood vessels (compartment syndrome).
One of the earliest signs of infiltration can be a slow infusion. Other signs of infiltration include local edema, complaints of pain at the site, and localized cooling of the skin (Figure 27-27). An infiltration of an unmedicated solution should be treated by immediate removal of the catheter and application of a warm compress to the site. Any infiltration of medicated solutions should be reported and treated immediately.
Occasionally IV sites become infected. While a Paramedic would not see an infection of an IV site from a recently placed IV, patients receiving at-home intermittent intravenous infusions with temporary indwelling intravenous catheters and those who are discharged home after a short hospital stay may have signs of an infection at the insertion site. An infection at the insertion site is called a thrombophlebitis. An IV access site is essentially a puncture wound, and the body responds to an IV cannulation as it would any wound. A thrombus is formed at the wound and the injury healing process begins. However, the catheter keeps the wound open. Bacteria tends to track into the wound, by capillary action, and the area becomes inflamed.40-42
Figure 27-27 Infiltration of medication at intravenous site.
Signs of thrombophlebitis include warmth in the area, pain upon palpation, and reddened and swollen tissues. As the infection progresses, the infection can advance up the vein, creating a visible red trail along the course of the vein and pain along the vein’s length.
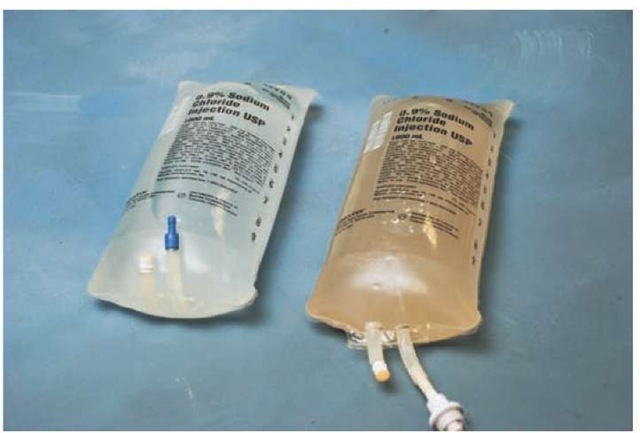
While a Paramedic may rarely see a thrombophlebitis related to a fresh IV, Paramedics may be witness to a pyrogenic reaction, a devastating systemic complication of intravenous therapy. A pyrogenic reaction occurs when a contaminated fluid, or fluid run through a contaminated administration set, is infused and leads to nearly immediate sepsis. Symptoms of a pyrogenic reaction usually occur within 30 minutes of the initiation of the infusion and include complaints of headache, chills, and backache. Signs that will accompany a pyrogenic reaction include fever, tachycardia, and, in severe cases, cardiovascular collapse. Examination of the solution for contaminants as well as verification of the expiration date can help reduce the incidence of pyrogenic reaction (Figure 27-28).
If a pyrogenic reaction is suspected, the Paramedic should immediately discontinue the infusion. The administration set and intravenous solution should be retained for microbiological examination and the lot numbers of the solution recorded on the patient care report. Fortunately, with the advent of disposable single-use administration sets and tightly controlled manufacturing processes, the number of pyrogenic reactions is very low.
Another potentially devastating complication of intravenous infusions is volume overload. A volume overload occurs when a positional IV access is inadvertently adjusted and the infusion flow is unrestricted. It can also occur when a clamp is released (e.g., to administer a fluid bolus) and the infusion rate is not re-adjusted.
The symptoms of a volume overload include a nonproductive cough, wheezing, and complaints of shortness of breath or headache. Accompanying signs of volume overload include hypertension, marked jugular venous distention, and crackles in the lung fields that are indicative of pulmonary edema. Initially, the Paramedic should reduce the infusion to KVO/TKO or consider using an intermittent infusion device (a saline well). Prehospital care of the patient with a suspected volume overload centers on symptomatic relief and supportive care.
Figure 27-28 Grossly contaminated solution (on the right), as compared with clean solution (on the left).
Another serious complication of intravenous infusions is an air embolism. An air embolism can occur when the Paramedic fails to run fluid through an intravenous administration set to flush the line prior to use. Symptoms of air embolism include chest pain and lightheadedness. Signs of air embolism include cyanosis, as well as hypotension which can, in severe cases, lead to cardiovascular collapse. If an air embolism is suspected, the infusion should be stopped. The patient should then be placed in the left lateral recumbent position, with the right lung superior and the feet elevated above the level of the heart. The Paramedic should provide supportive care and contact medical control for further instructions.