Miscellaneous Effects on the ECG
Electrolyte abnormalities, particularly potassium, can cause changes in the appearance of the 12-lead ECG. While the Paramedic does not usually have access to lab results, the patient’s history may suggest the potential for electrolyte disturbances. For example, patients in end-stage renal disease may experience elevation of potassium levels while those patients receiving diuretics may have a decreased level of potassium unless they receive potassium supplementation.
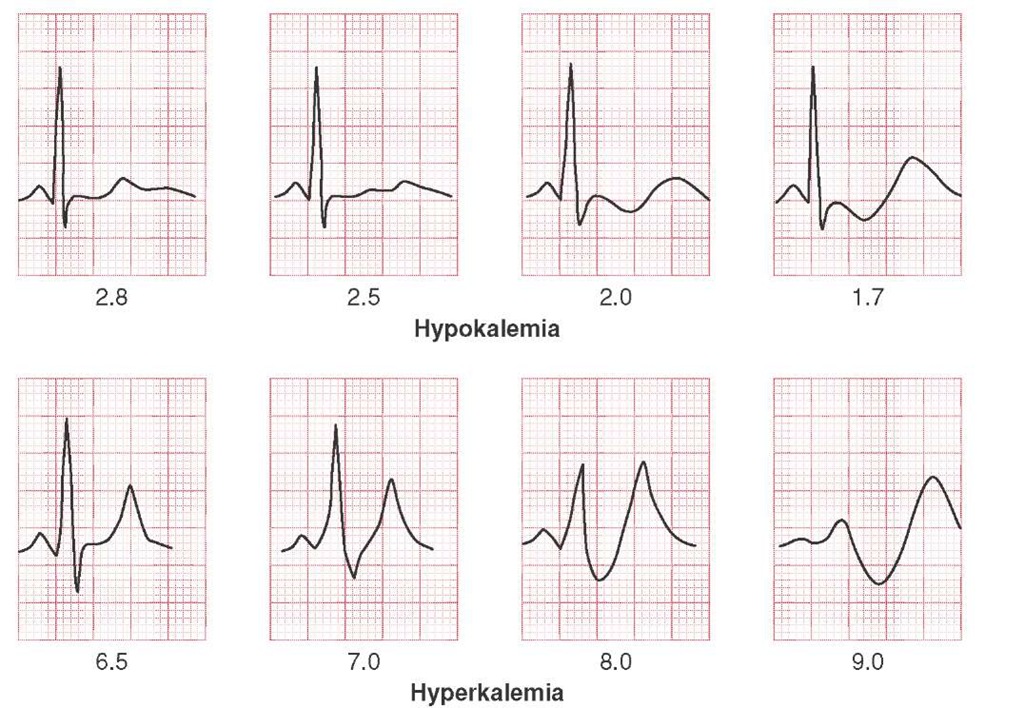
A normal potassium level, between 3.5 mEq/L and 4.5 mEq/L, is important for optimum cardiac cell function. If the patient is hypokalemic (i.e., serum potassium less than 3.5 mEq/L), then the patient may be prone to decreased inotropy. This can lead to generalized weakness or malaise, and/or dys-rhythmias such as atrial flutter and bradycardia.
Causes of hypokalemia are numerous and include vomiting, aggressive gastric suctioning, diarrhea (secondary to infectious diseases), or abuse of potassium-wasting diuretics such as furosemide. With hypokalemia, the 12-lead ECG may show T wave flattening, ST-segment depression, and/or U wave development.49,50
Hypokalemia is often associated with low magnesium levels or hypomagnesemia (Figure 34-27). Hypomagnesemia may predispose the patient to a form of polymorphic ventricular tachycardia called torsades de pointes.51
Albuterol is a bronchodilator but also drives potassium into the cells. Aggressive use of albuterol (i.e., stacked treatments) may cause changes in cellular uptake of potassium, putting the patient at risk for low potassium levels and dysrhythmias.
Perhaps more problematic for the Paramedic may be hyperkalemia. A serum potassium level above 4.5 mEq/L is considered hyperkalemia. One of the most common causes of hyperkalemia is kidney failure. Patients who are on kidney dialysis are at obvious risk of hyperkalemia prior to dialysis. Other at-risk patients include patients with diabetes who are experiencing diabetic ketoacidosis, patients with severe burns, patients with crush injury, and those patients with acute tubular necrosis secondary to shock.
Figure 34-27 ECG changes associated with hypokalemia and hyperkalemia.
The common ECG alterations seen in hyperkalemia are changes in the T wave. At potassium levels greater than 4.5 mEq/L but less than 6.5 mEq/L, the T wave appears tall and peaked and is best seen in inferior leads (Lead II and Lead III). As the potassium level continues to climb toward 8 Eq/L, the QRS starts to widen and a left axis deviation may be appreciated. Finally, as the potassium level climbs above 8 mEq/L, the P waves all but disappear and the QRS starts to flatten into a sine wave configuration. It is at this time the patient’s cardiac output has dropped precipitously and the patient is at risk for ventricular fibrillation or asystole.
Arrhythmias caused by hyperkalemia are very difficult to treat with defibrillation or the usual emergency drugs without lowering the serum potassium level. Calcium chloride, calcium gluconate, or sodium bicarbonate, all competitive electrolytes, may be used to lower potassium levels. Alternatively, serial treatments with Albuterol may help to treat mild to moderate hyperkalemia. In severe cases, it may be necessary to administer 50% dextrose with short-acting insulin.52 The insulin helps to drive both glucose and potassium into the cells.
STREET SMART
Calcium is needed for regular cell function. Loss of calcium (serum calcium levels less than 8.5 mg/dL) or hypocalcemia is rare. Typical causes of calcium disturbances are chronic diseases. The effect of calcium is seen on the QT interval. Hypocalcemia causes a widened QT interval whereas an elevated serum calcium causes a short QT interval. To remember that calcium is related to QT, the Paramedic need only remember that QT interval is corrected for heart rate and recorded on the 12-lead ECG as such (i.e., QTc). The little c could represent calcium, to remind the Paramedic of other causes of prolonged/shortened QT intervals.
Extra-Cardiac Causes of ECG Changes
Potentially devastating extra-cardiac pathologies, such as intracranial hemorrhage, hypothermia, and pericarditis, can also cause changes on the 12-lead ECG. While not pathognomonic for these pathologies, they are another sign to be added to the symptom complex for diagnosis.
An acute rise in intracranial pressure secondary to sub-arachnoid hemorrhage, intracerebral bleed, or an epidural bleed may lead to wide and deeply inverted T waves in the chest leads.53-55 The Paramedic’s attention is likely focused on other more urgent matters during one of these events. However, 12-lead ECG evidence, if obtained, may be useful at the emergency department.
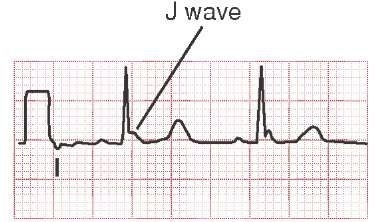
Hypothermia affects all cellular functions and can also cause changes in the ECG. When a patient is hypothermic, all of the interval durations (i.e., PR, QRS, and QT) lengthen and positive deflections at the J point, or point where the ventricular complex ends and the ST segment begins, become noticeable. These deflections are in the same direction (polarity) as the QRS and are termed Osborn waves (sometimes called the camel-hump sign). The Osborn wave is seen in all leads, but is more prominent in the inferior limb leads. The size of the Osborn waves correlates directly with the degree of hypothermia. Osborn waves are often difficult to discern because of artifact from muscle tremors (Figure 34-28), but are seen in 80% of patients with hypothermia (below 33°C/91.4°F).56
Finally, pericarditis, an inflammation between the pericardium and the epicardium, can cause chest pain and 12-lead ECG abnormalities. Initially, the Paramedic may be led to believe that the chest pain is secondary to acute coronary syndrome. However, nitrates are not useful in treating the pain of pericarditis, so it is important for the Paramedic to seek historical clues to the diagnosis of pericarditis (i.e., fevers, etc.) as well as ECG evidence.
The inflammation that occurs between the sac surrounding the heart and the epicardium leads to swelling which puts some pressure on the myocardium. The myocardium cannot repolarize as it normally does due to the swelling, so there are T wave changes. The T will become pointed and tall (similar to a hyperacute T wave found in an MI). However, the changes tend to occur in all leads rather than within contiguous leads only, leading the Paramedic to suspect other causes for the chest pain, such as pericarditis.
Evaluation
One of the advantages of the 12-lead ECG is its ability to predict the clinical progression of the patient’s disease if left unchecked. For example, in the case of a patient with an anterior wall myocardial infarction (AWMI), the patient may eventually develop cardiogenic shock secondary to lost myo-cardial function. In this case, the patient had an IWMI that could, predictably, either extend to the mitral valve (causing mitral valve regurgitation) or extend into the right ventricle. It is estimated that 50% of IWMI extend into the right ventricle, with a resultant loss of preload.
Figure 34-28 Osborn wave secondary to hypothermia.
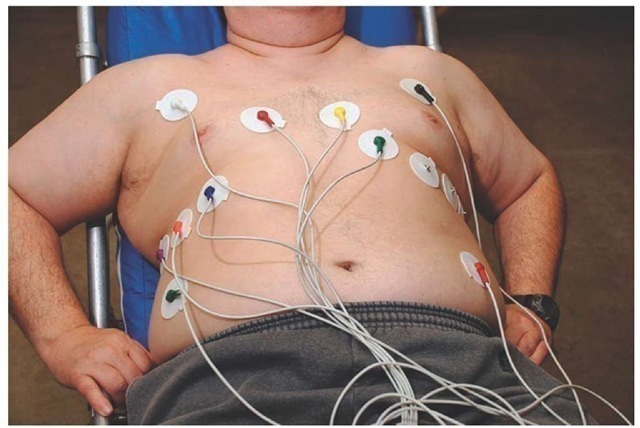
Figure 34-29 Lead placement for a 15-lead ECG, which is helpful in assessing the right ventricle.
STREET SMART
The right ventricle essentially primes the pump (the left ventricle). Loss of right ventricular function, secondary to myocardial injury, can lead to profound hypotension. For this reason, some Paramedics perform a 15-lead ECG to identify right ventricular involvement before administering vasodilators such as nitroglycerin.
15-Lead ECG
An additional diagnostic test available to the Paramedic if the Paramedic suspects right ventricular involvement is the 15-lead ECG.57 The electrode placement for a 15-lead ECG will place positive electrodes onto the right side of the chest and view the right ventricle.
Locations for these electrodes are the 5th right intercostal space at the midclavicular line, 5th right intercostal space anterior axillary line, and 5th right intercostal space at midaxillary. The corresponding V4 to V6 wires from the left chest electrodes are switched over to the right electrodes and the ECG is rerecorded (Figure 34-29). The repeated ECG is marked right chest leads or V4R, V5R, and V6R.
Conclusion
The diagnostic 12-lead electrocardiogram is a useful tool in the Paramedic’s assessment tool box with the potential to improve patient outcome by early detection of cardiac abnormalities. This is especially true in situations where the patient presents with an acute ST elevation myocardial infarction, where the patient can be triaged to the appropriate hospital, or in cases of dynamic changes in the ECG that change with treatment, uncovering underlying cardiovascular disease.
key points:
• Death from AMI remains a national health problem.
• Aggressive prehospital treatment including obtaining and interpreting a 12-lead ECG can favorably impact patient mortality and morbidity.
• Paramedics must have a higher index of suspicion with patient populations that may present with atypical cardiac symptoms.
• A regular ECG uses standard limb leads, augmented limb leads, and precordial leads.
• The regular ECG allows for inferior, anterior, and lateral views of the left ventricle, as well as combinations.
• Accurate 12-lead ECG requires proper patient preparation including standardized electrode placement.
• A 12-lead ECG is printed in a standard configuration.
• Viewing a specific combination of leads, called contiguous leads, allows correlation to specific ventricular walls.
• Based upon coronary artery anatomy, ECG changes in contiguous leads permit Paramedics to estimate damage in specific arteries.
• Estimation of damage in specific arteries permits prognosis and planning.
• Understanding an acute myocardial infarction requires an understanding of penumbra.
• Additional ECG evidence, such as new onset left bundle branch block (LBBB) and reverse R wave progression (RRWP), are important in supporting the diagnosis of myocardial infarction.
• Some 12-lead ECGs do not show acute changes. The Paramedic should focus on treating the patient based on history.
• There are numerous extra-cardiac causes to ECG abnormalities.
• 12-lead ECG interpretation takes a disciplined approach that gathers all the pertinent information to prevent premature interpretation.
• Based on the 12-lead ECG interpretation and the patient history, the Paramedic can make a field diagnosis.
• Additional information is also available from the 12-lead ECG that can lend insight into other health conditions.
• The 12-lead ECG can help differentiate ventricular tachycardia (VT) from supraventricular tachycardia.
• The addition of three right-sided leads can help identify right ventricular AMI.
• Early detection of MI, via 12-lead ECG, and rapid transportation to an interventional cardiac care center can lead to better patient outcomes.