Electrocardiographic Diagnosis of Acute Myocardial Infarction
To make an electrocardiographic diagnosis of acute myo-cardial infarction, the Paramedic looks for hyperacute T waves, T wave inversions, ST-segment depressions, and ST-segment elevations as well as Q waves in all leads. When a pattern of ischemia is noted (ECG changes in contiguous leads), then the Paramedic may have a high index of suspicion that the artery which perfuses the corresponding wall is occluded.28
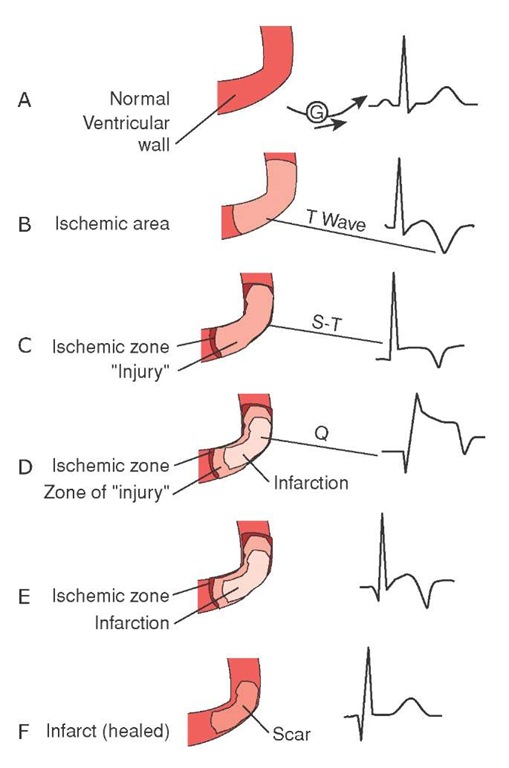
The presence of Q waves in the face of concomitant ST elevation speaks to the evolution of the infarction and may indicate that this MI has been in progress for several hours (Figure 34-15). However, the presence of ST elevations indicates that there may be myocardium that can be salvaged with thrombolytic therapy or interventional cardiology.
Reciprocal Changes
Supporting evidence of an acute myocardial infarction in progress are reciprocal changes. Reciprocal changes are ST-segment depressions seen on the 12-lead ECG in leads that face the wall opposite of those with ST-segment elevations. Reciprocal changes are more commonly seen in inferior wall AMI (approximately 70%) versus anterior wall AMI (about 30%).29,30 The presence of reciprocal changes is an excellent marker of acute myocardial infarction in progress and has a positive predictive value of 90%.
The ST-segment depression of reciprocal changes is thought to be due to "mirror reflections" of the electrical signal from the affected wall. The ST-segment depression seen in a reciprocal change is more downsloping than those caused early in an AMI and is typically seen when the AMI is large.
As an example of the predictive value of reciprocal changes, ST depression in leads V1, V2, V3, and V4 (all anterior leads) suggests an acute myocardial infarction in evolution in the posterior wall and an occlusion of the circumflex artery (Cx) (Table 34-4).
Figure 34-15 Wave changes during evolution of myocardial damage.
Table 34-4 Reciprocal Changes
|
Wall |
Artery Lead |
Reciprocal Wall |
Reciprocal Leads |
|
Inferior |
RCA II, II, aVF |
Lateral |
I, aVL |
|
Anterior |
LAD V3, V4 |
Inferior |
II, III, aVF |
|
Lateral |
Cx I, aVL, V5, V6 |
Inferior |
II, III, aVF |
STREET SMART
ST depressions seen in reciprocal changes can be helpful in distinguishing infarction from the normal variants in African American males who have ST elevations.
R Wave Progression
In a normal 12-lead ECG, there is a series of changes in the primary deflection of the QRS from negative in V1 to positive in V6, called an R wave progression, in the precordial leads. Starting with the deep S wave in V1, the deflection in the precordial leads gradually changes direction, with a transition at approximately V3 or V4, until V6, where there is a tall R wave.
Whenever there is an electrical disturbance in the anterior wall, secondary to ischemia, then the R wave progression is disturbed (specifically when there is a loss of R waves in the anterior precordial leads). The loss of an R wave progression, sometimes called a reverse R wave progression, is suggestive of an anterior wall AMI.
If the transition occurs early (i.e., before V3), it may be indicative of a posterior wall AMI. The Paramedic may then want to consider obtaining leads V7, V8, and V9 (discussed later). If the transient occurs later, after V4, it can be suggestive of an anterior wall AMI. However, a late transition can also occur if the patient has a thick chest or has respiratory disease, particularly if there are small R waves in the right precordial leads, or may be a normal variant in some women.
STREET SMART
Some Paramedics may use the term "poor R wave progression." The American Heart Association prefers the term "reverse R wave progression" instead. It should be noted that improper lead placement can cause a reverse R wave progression.
The isolated appearance of a reverse R wave progression (RRWP) should not be taken to mean that the patient is having an anterior wall AMI. There are other causes of RRWP which include a pre-existing left bundle branch block, dex-trocardia, and Wolff-Parkinson-White (WPW) syndrome. Nevertheless, the presence of a reverse R wave progression, coupled with a good history for ACS and other 12-lead ECG changes in the anterior leads, is helpful in diagnosing an anterior wall AMI.
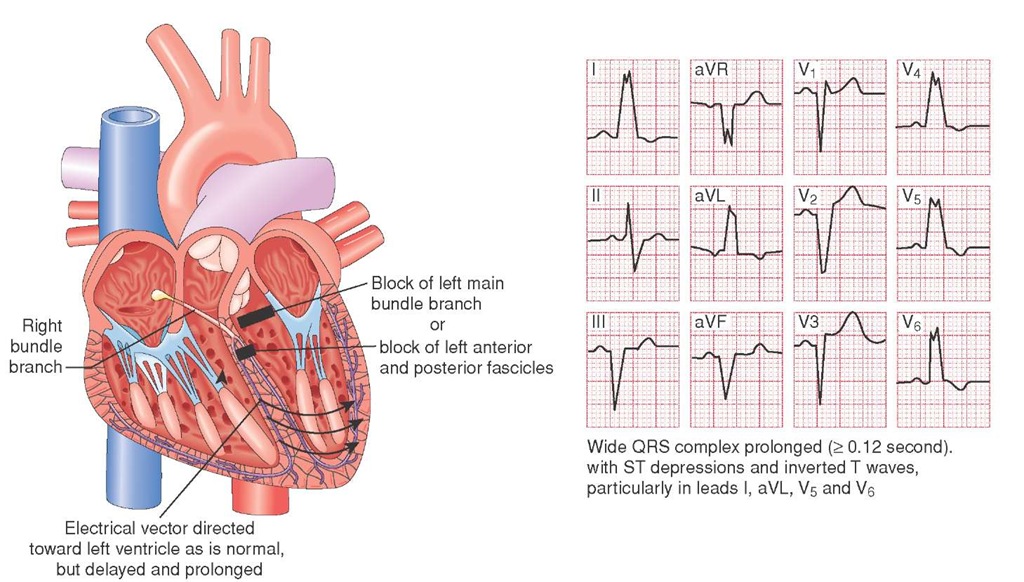
New Onset Left Bundle Branch Block
A left bundle branch block (LBBB) (Figure 34-16) is a partial heart block (when the impulse fails to be conducted) which involves one or both the left fascicles of the left bundle. As a result, the ventricular wall of the affected side must be depolarized by a wave front from the opposite side. This delay in depolarization prolongs the QRS to greater than 0.14 seconds for a left bundle branch and a small narrow R wave (less than 0.04 seconds) in all leads. The Paramedic may also observe that the T wave is opposite in deflection to the QRS in all precordial leads, as well as a notching in the anterolateral leads.
The characteristic appearance of a notched QRS in V6 (i.e., RsR’) is the result of the electrical impulse crossing the right bundle branch, depolarizing the right ventricle, then crossing the interventricular septum to depolarize the left ventricle.
A common cause of an LBBB is occlusion of either the left anterior descending (LAD) coronary artery or one of the septal perforators which branch from the LAD. These coronary arteries perfuse the septum and the bundle branches that lie within.
Because of the delayed repolarization, the ST segment of the septal leads will be elevated and the 12-lead ECG will have the appearance of an anterior wall AMI (AWMI). However, there are a number of benign conditions, including advanced age and hypertension, that can also cause an LBBB.31
In some cases, because of advanced atherosclerotic disease, the patient may experience a rate-related bundle branch block. These blocks occur because the bundle branches are incapable of repolarizing, secondary to decreased perfusion, at faster rates. Because of slower conduction, there is reduced strength of contraction and the patient may experience heart failure.
STREET SMART
Whenever an LBBB occurs, the patient is at risk of heart failure. Therefore, the administration of any Vaughn-Williams Class 1 drugs (i.e., lidocaine or procainamide) can slow conduction even further, leading to worsened heart failure and even to drug-induced complete heart block.
Typically, the altered electrical pathway associated with LBBB makes the ECG diagnosis of AMI complicated. Therefore, if a Paramedic observes an LBBB on initial 12-lead ECG, no further interpretation is possible because a diagnosis of AMI by ECG cannot be made with confidence. However, the presence of a new onset LBBB during the course of patient care is an ECG finding highly suggestive of an AMI.
The Paramedic should report the appearance of a new onset LBBB and, coupled with a patient history suggestive of ACS, have a high index of suspicion that the patient is having an AMI.32-34 Patients with a new onset LBBB have a worse prognosis for their AMI compared to those without the conduction delay. Because of the prolonged conduction, and the resultant decreased inotropy, a patient with an LBBB may experience as much as a 25% loss of cardiac output. Paramedics should treat new onset LBBB more aggressively, with a keen eye on the development of heart failure.
Figure 34-16 Left bundle branch block.
STREET SMART
An LBBB during the course of an AMI can progress to a complete heart block. As a result of this complete heart block (CHB), the escape rhythm will be idioventricular. Typically, patients with an idioventricular rhythm require a pacemaker.
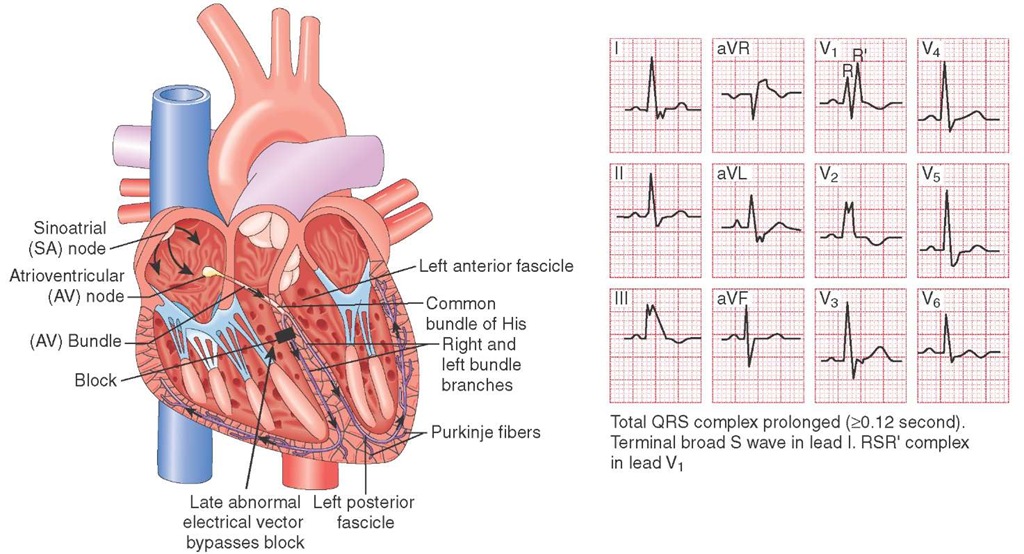
Right Bundle Branch Block
A right bundle branch block (RBBB) is a type of heart block in which the impulse fails to be conducted down the right bundle of the bundle of His. In a RBBB, the impulse travels rapidly to depolarize the interventricular septum and down the left bundle branch to activate the left ventricle. Since the right bundle branch is blocked, the impulse must cross the inter-ventricular septum to activate the right ventricle. Because it takes more time to depolarize the entire ventricle, the QRS is greater than 0.12 seconds in width.
The ECG diagnosis of RBBB is also supported by a small terminal R wave in V1 and a slurring of the S wave in the lateral leads (i.e., Lead I and V6). The T wave in V1 will also be in the opposite deflection of the QRS.
A RBBB is one of the most common defects in ventricular conduction (Figure 34-17). RBBB occurs often, and without apparent cause, in normal hearts. Treatment is directed at the cause of the conduction defect, which can include myocardial infarction (MI) or ischemia, heart failure, pulmonary embolism, or valvular disease.
Nondiagnostic ECG
In some cases, the patient may have a benign 12-lead ECG. The absence of patterns of ischemia on a 12-lead ECG does not preclude the diagnosis of an AMI. When the 12-lead ECG is nondiagnostic, the Paramedic should maintain a high index of suspicion based on the patient’s clinical presentation and, more specifically, the history of present illness.
In some cases, the diagnosis of AMI on 12-lead ECG is missed because of the low amplitude of the QRS. When the amplitude of the QRS is less than 5 mm in the standard limb leads (i.e., low amplitude QRS), an assessment of ST-segment change is nearly impossible. Causes of low voltage, resulting in a low amplitude QRS, include pericardial effusions leading to constructive pericarditis, pleural effusions, and obesity.35-37
Electrical Alternans
When every other ECG complex has alternating amplitude (i.e., the one QRS complex is smaller when compared to the next), then the patient may have electrical alternans. Electrical alternans is more frequently seen in the precordial leads and is a sign of pericardial effusion.
The alternating amplitude of the QRS is thought to be the result of the heart swinging, in a pendulum fashion, from the wave created in the pericardium as the heart beats within the accumulation of fluid.
Figure 34-17 Right bundle branch block.
Alternative Etiologies for ECG Abnormalities
The Paramedic should keep an open mind when reading a 12-lead ECG for alternative causes of prolonged QT intervals, T wave abnormalities, and ST-segment elevations. Although these aberrant changes do not typically mimic the pattern of ischemia, a quick glance could mislead a Paramedic into thinking that there is a pattern of ischemia. Careful attention to the ECG for patterns of ischemia and a disciplined approach to interpretation will yield the best results.
Prolonged QT Intervals
One of the first ECG changes which can occur as a result of anterior wall myocardial ischemia (AWMI) can be a prolonged QT interval. However, there are a host of other etiologies for prolonged QT intervals.38,39 The majority of causes of acquired prolonged QT intervals involve electrolyte abnormalities (e.g., hypokalemia) and medications. Vaughn-Williams Class I and III drugs are the leading offenders and have been repeatedly implicated as the cause of prolonged QT intervals. Other potential offenders include psychotropic medications (particularly tricyclic antidepressants and phe-nothiazines), antibiotics (such as erythromycin), and toxins (such as organophosphates).40
In some cases, the cause of the prolonged QT interval is congenital. These patients may have presented in their youth with unexplained syncopal episodes. For this reason, any patient, regardless of age, who has an unexplained syncope should be a candidate for a 12-lead ECG.
STREET SMART
One of the first ECG changes associated with hypothermia is a prolonged QT interval. The difficulty in obtaining a 12-lead ECG, because of the cold skin and resultant poor penetration of the electrode gel, makes this assessment problematic.
The length of the QT interval is inversely related to the patient’s heart rate. Therefore, when calculating a patient’s QT interval, it must be corrected with the heart rate. Typically, Paramedics and physicians use Bazett’s formula to obtain the correct QT interval. Under emergency conditions, the QTc (corrected QT) can be derived from information on the 12-lead ECG. Alternatively, the Paramedic can take the heart rate and, for every ten (10) beats above 70, subtract 0.02 seconds from 0.40 seconds, and for every ten (10) beats below 70 add 0.02 seconds.
T Wave Abnormalities
Generally, the T wave in a normal ECG is in the same deflection as the preceding QRS in the limb leads. The normal T wave is slightly asymmetrical, with the upstroke of the leading edge of the T wave being gentle compared to the downstroke. Any deviation from those conditions would be abnormal.
T wave abnormalities can include T wave inversion, flattened or low-amplitude T waves, and peaked or hyperacute T waves. There are numerous causes for the T wave abnormalities that can be suggestive of a number of disorders (Table 34-5). With the exception of hyperkalemia, the isolated presence of a T wave abnormality is not diagnostic of any condition and requires further investigation.
Hyperacute T Waves
Hyperacute T waves are defined as T waves greater than 5 mm in the limb leads and greater than 10 mm in the precordial leads. While a peaked T wave in contiguous leads is suggestive of ischemia, hyperacute T waves in all leads is highly suggestive of hyperkalemia.41,42 Hyperkalemia can be the result of renal failure or crush injury, or seen in cases of diabetic ketoacidosis (DKA). Conversely, flattened T waves are suggestive of hypokalemia, a deficit in serum potassium that can be the result of potassium-wasting diuretics (e.g., furosemide).
ST-Segment Abnormalities
While an ST-segment depression is suggestive of ischemia when seen in select contiguous leads, a global ST-segment depression, affecting all of the precordial leads, suggests the etiology is likely extra-cardiac (Table 34-6).
Table 34-5 Potential Causes of T Wave Abnormalities
|
• CNS disorders |
|
o Cerebrovascular accident (CVA) |
|
o Subarachnoid hemorrhage |
|
• Cardiac disease |
|
o Mitral valve prolapse |
|
o Myocarditis |
|
o Pericarditis |
|
o Ventricular hypertrophy |
|
o Conduction disorders |
|
• Bundle branch block |
|
• Ventricular preexcitation |
|
• Post ventricular tachycardia |
|
• Electrolyte disorders |
|
o Hyperventilation |
|
• Pulmonary conditions |
|
o Pulmonary embolism |
|
o Pneumothorax |
|
• Gastrointestinal conditions |
|
o Acute pancreatitis |
|
o Acute cholecystitis |
|
• Pharmacology |
|
o Digitalis |
|
o Antidysrhythmic agents |
|
o Alcohol |
|
o Cocaine |
Table 34-6 Causes of ST-Segment Depression
|
• Hypokalemia |
|
• Hypothermia |
|
• Hypertrophy-Ventricular |
Medications, for example, can cause alterations in the ST segment. A classic cause of ST-segment depression is digitalis. Digitalis alters ventricular depolarization, resulting in a "ladle" appearance of the ST segment (Figure 34-18).
Other causes of ST-segment depression include suba-rachnoid hemorrhage and hypokalemia. Hypokalemia (serum potassium less than 2.8) will produce ST-segment depression in 80% of patients, along with flattened T waves (Figure 34-19).
Similarly, ST-segment elevation can be a normal variant, with some patients demonstrating a 1 to 2 mm ST segment rise, particularly if the ST segment has an upward concavity and/or a notch at the J point (Table 34-7). This finding is particularly common among African Americans and leaves the ST segment with a fishhook appearance.
STREET SMART
Current pacemakers are so efficient that they do not leave a "foot print" (a pacer spike) on the rhythm strip. The only evidence of a pacemaker may be the slow and wide QRS as well as a slight ST-segment elevation noted in the precordial leads.