Doppler
An ultrasonic vascular Doppler device is sometimes used to detect peripheral pulses (Fig. 46-12). Apply a conductive gel and place the Doppler transmitter over the artery being assessed. The earpieces or a special speaker attached to the Doppler device amplify the sounds. They may also be recorded on a computer or on a special printout. The nurse will need special instruction in the use of this device.
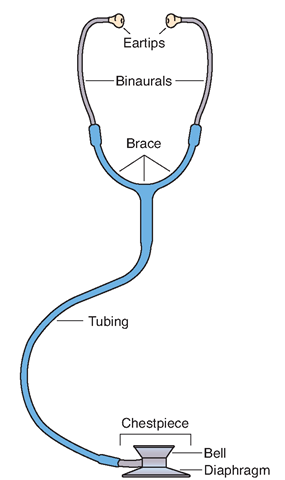
FIGURE 46-11 · Parts of a stethoscope.
FIGURE 46-12 · The Doppler device is used to auscultate the pulse in some situations, particularly if the pulse is difficult to hear or feel. Here, the nurse counts the dorsalis pedis pulse (pedal pulse) in the foot. If the Korotkoff’s sounds are very difficult or impossible to hear the Doppler provides an alternative when measuring blood pressure as well.
Measuring the Pulse
Many automated blood pressure machines also measure the pulse. If this is not the case, the nurse counts the client’s pulse (heart rate). There are a number of locations for doing this (see Fig. 46-10).
Radial Pulse
The radial artery in the wrist is most commonly used to count the pulse because of its convenient location. In Practice: Nursing Procedure 46-2 outlines the steps in counting a radial pulse.
Apical Pulse
The apical pulse (AP) is more accurate than the radial pulse and is always the pulse taken for children younger than 2 years. In Practice: Nursing Procedure 46-3 outlines the steps in counting the apical pulse. Always measure the client’s apical pulse if any question arises about the heart’s rhythm or rate or if it appears that the heart has stopped. In some cases, the healthcare provider orders apical pulse measurement as a routine order.
Apical-Radial Pulse
An apical-radial pulse (A-R) measurement is ordered when it is suspected that the client’s heart is not effectively pumping blood. If the apical and radial measurements are not the same, a pulse deficit exists. This must be reported to the healthcare provider. Two nurses are needed to carry out this procedure (see Fig. 46-13). In Practice: Nursing Procedure 46-3 gives the steps for taking this measurement.
Nursing Alert It is impossible for the apical pulse to be lower than the radial. If this finding occurs, you have made a mistake. Take both pulses again.
FIGURE 46-13 · Apical -radial pulse. One nurse counts the radial pulse while the other counts the apical rate. Both use the same watch. The person counting the radial pulse calls the time.
Pedal Pulse
The pedal pulse (foot pulse) is felt over the dorsalis pedis artery or the posterior tibial artery of the foot. The pulse point is located on top of the foot, posterior to the toes (see Fig. 46-12). The status of blood circulation to the foot can be determined at these pulse points. A strong pulse indicates that circulation to the lower extremities is unrestricted, whereas a weak and irregular pulse suggests impaired or restricted blood flow. Use caution in palpating the pulse site, so that the pulse is not completely obliterated with excessive pressure. Inspect the feet for color, temperature, and presence of edema (swelling). Also observe the condition of the client’s toenails and cuticles. Always check pedal pulse bilaterally (in both feet) for comparison. If a pedal pulse cannot be detected, the documentation should state “pedal pulses not palpable” and indicate if this is in the right or left foot, or both. Avoid documenting “absent pedal pulses” because the pulses may actually be present, but are not detectable manually; this is an instance in which the Doppler might be used. If pedal pulses cannot be detected, documentation also should include what was done, such as elevating the involved foot (feet). The nurse should also document findings such as “capillary refill less than 3 seconds (or more), skin color pink (or otherwise), and foot warm to touch (or not).” This situation should be reported immediately.
Popliteal Pulse
The popliteal pulse is located posterior to the knee. It is palpated by placing the fingers in the space behind the knee. Use this site to assess the status of circulation to the lower leg or as an alternative means of assessing blood pressure with a large leg cuff.
Carotid Pulse
The carotid pulse, on either side of the neck, can be located directly over the carotid artery. Palpate this pulse along the medial edge of the sternocleidomastoid muscle above the cricoid notch (see Fig. 47-36). The carotid artery is easily accessible for checking the peripheral pulse. Individuals who must do self-checks often use this method. It is also used in cases of shock when other pulses are not palpable and to determine the need for cardiopulmonary resuscitation (CPR).
The pulse is counted on either side of the neck. The client’s head is positioned midline to the body. Rationale: Such positioning provides easier access to the pulse, which is obliterated when the head is turned to one side or the other.
Nursing Alert Never check carotid pulse on both sides of the neck at the same time. Rationale: Doing so could cut off circulation to the brain, possibly causing a cerebrovascular accident (CVA, stroke). Use the fingertips to palpate the carotid pulse. Do not reach across the person’s neck to count carotid pulse. Rationale: The client’s airway could be occluded by the pressure of the examiner’s arm. Count the carotid pulses in the client’s neck on the side closest to you.
ASSESSING RESPIRATION
Oxygen keeps body cells alive; accumulated carbon dioxide kills cells. Respiration is the process that brings oxygen into the body and removes carbon dioxide. This exchange takes place in the lungs.Observing respiration closely is necessary to detect signs of interference with the breathing process.
Regulation of Respiration
Respiratory Control
The brain’s respiratory center, stimulated by the proportion of carbon dioxide in the blood, controls and regulates respiration. Injury to the respiratory center or to the nerves connecting it with the lungs affects respiration; too little or too much carbon dioxide in the blood also affects breathing. Respiratory functioning may also be impaired by conditions (e.g., fractured ribs or thoracic surgery), causing pain on breathing, or by obstruction of the airway.
The organs that accomplish breathing include the lungs, the chest muscles, and the diaphragm; injuries to these parts of the body affect respiratory functioning. Respiration is automatic; people breathe without thinking about it. You can control your breathing to some extent by taking deeper or shallower breaths or even by holding your breath for a limited time. When the limit is reached, automatic control takes over, and your chest muscles relax despite your efforts. If this automatic resumption of breathing does not occur, a breathing disorder exists. An example is apnea (cessation of breathing), which occurs in sudden infant death syndrome (SIDS), sleep apnea, and other conditions.
Rate and Depth
The normal respiration rate for an adult is 12 to 18 breaths per minute. Women have a more rapid rate than do men. For newborns, the average rate is approximately 40 breaths per minute; for children, the average rate varies from 25 to 35 breaths per minute (Table 46-2).
TABLE 46-2. Normal Respiratory Rates at Various Ages
|
AGE |
AVERAGE RANGE OF RESPIRATION (per minute) |
|
Newborn |
30-80 |
|
Early childhood |
20-40 |
|
Late childhood |
15-25 |
|
Adulthood |
|
|
Men |
12-18 |
|
Women |
I6-20 |
Nursing Alert In the adult, a respiration rate below 10 or above 24 breaths per minute is a sign of respiratory
impairment. Report this situation promptly.
Normal breathing is called eupnea. When respirations are abnormally rapid (20–24 breaths per minute), tachypnea is present. When respirations are abnormally slow and fall below 10 breaths per minute, bradypnea occurs. Table 46-3 discusses abnormal breathing patterns.
Excitement, exercise, pain, and fever increase respiratory rate. Rapid respiration is characteristic of lung diseases such as pneumonia and emphysema. Heart disease, hemorrhage, and nephritis also increase the rate, as do some drugs. Rapid respiration indicates that the body is making an increased effort to maintain the correct balance of oxygen and carbon dioxide. The body is also trying to adjust the balance by taking deeper breaths. Note that all people sigh or yawn occasionally to cleanse the lungs and physiologically expand the small airways and alveoli that are not used during ordinary respiration. This also helps to equalize the pressure between the outside atmosphere and the middle ear, via the eustachian or auditory tube. Do not confuse sighing with abnormal or difficult breathing.
Pressure on the brain’s respiratory center decreases the respiration rate; cerebral hemorrhage also has this effect. Some drugs, such as opium preparations, depress the respiratory center. Poisons that accumulate in the body in uremia and diabetic coma increase the depth of respirations. Known as Kussmaul’s respirations, this breathing pattern is characterized by labored breathing. Respirations are abnormally deep and gasping. Diabetic acidosis and diabetic ketoacidosis increase the total acid in the body, and the body compensates by trying to rid the body of the excess acid through deeper and faster respirations.
Respiration Sounds
Snoring occurs when the air passageway is partially blocked. It is common during sleep, when the person’s tongue falls back due to relaxation, particularly if the person is sleeping on the back. Stertorous breathing occurs when air passes through secretions present in the air passages. These bubbling noises or rattles are characteristic before death, when air passages fill with mucus. Sometimes, very loud snoring is referred to as stertorous breathing. Obstruction near the glottis causes a hissing, crowing sound.
|
TYPE |
DESCRIPTION |
PATTERN/CLINICAL INDICATION |
|
Normal |
12-20/min and regular |
Normal breathing pattern |
|
Tachypnea |
>24/min and shallow |
May be a normal response to fever, anxiety, or exercise Can occur with respiratory insufficiency, alkalosis, pneumonia, or pleurisy |
|
Bradypnea |
< 10/min and regular |
May be normal in well-conditioned athletes Can occur with medication-induced depression of the respiratory center, diabetic coma, neurologic damage |
|
Hyperventilation |
Increased rate and increased depth |
Usually occurs with extreme exercise, fear; or anxiety Kussmaul’s respirations are a type of hyperventilation associated with diabetic ketoacidosis. Other causes of hyperventilation include disorders of the central nervous system, an overdose of a salicylate drug, or severe anxiety. |
|
Hypoventilation |
Decreased rate, decreased depth, irregular pattern |
Usually associated with overdose of narcotics or anesthetics |
|
Cheyne-Stokes respiration |
Regular pattern characterized by alternating periods of deep, rapid breathing followed by periods of apnea |
May result from severe congestive heart failure, drug overdose, increased intracranial pressure, or renal failure. May be a sign of impending death. May be noted in elderly persons during sleep, not related to any disease process |
|
Biot’s respiration |
Irregular pattern characterized by varying depth and rate of respirations followed by periods of apnea |
May be seen with meningitis or severe brain damage |