Measuring Body Temperature
Several locations are used to measure body temperature. They are:
• Oral (O)—mouth
• Rectal (R)—anus
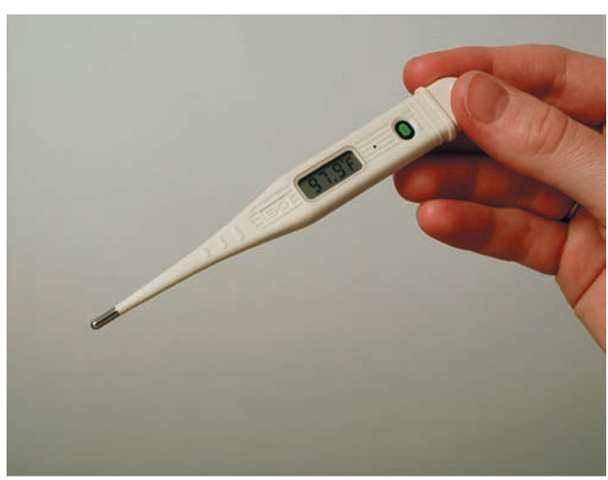
FIGURE 46-3 · This battery-operated temperature sensor is discarded when no longer needed or when the battery is depleted. The temperature shown here (97.9°F) is displayed digitally on the screen.
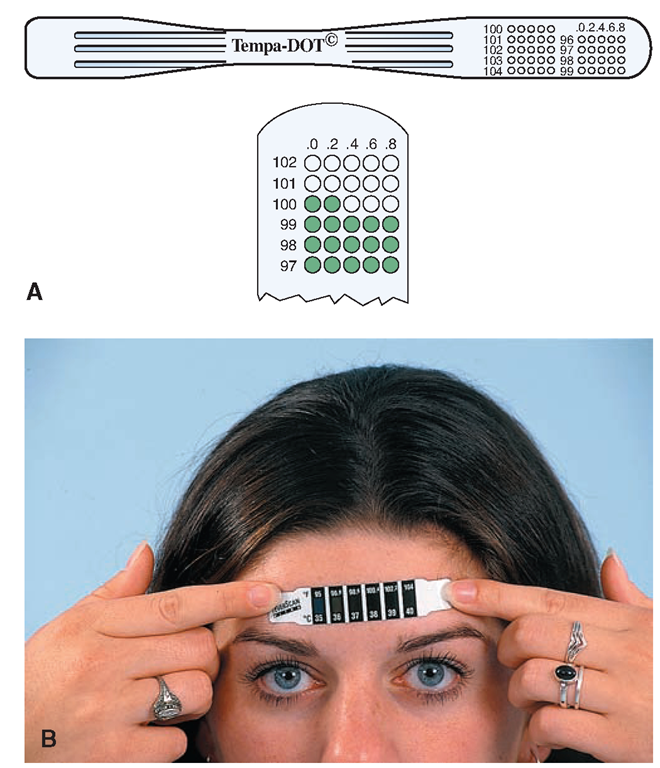
FIGURE 46-4 · (A) Chemical thermometer, showing a temperature reading of I00.2°F. (B) Applying a disposable chemical thermometer with heat-sensitive liquid crystals.
• Axillary (Ax)—armpit
• Tympanic, aural, or otic (TM—tympanic membrane)—ear canal
• Temporal artery (TA)—forehead
For all these locations (except the temporal artery), the thermometer probe is covered with a paper or plastic cover, which is discarded after each use, or, in the case of single-use thermometers, the entire device is discarded. The tip of the probe is surrounded by body tissues in these cases. The temporal artery temperature indicator is simply held over the forehead and discarded after use. Thermometer probes should be cleaned after use, according to the manufacturer’s instructions. All these devices measure temperature quickly and indicate the reading in digital numbers. In Practice: Nursing Procedure 46-1 presents the methods for taking oral, rectal, axillary, tympanic, and temporal artery temperatures.
Certain rules apply to using all types of thermometers and body areas:
• Every healthcare agency has an established routine for measuring the client’s temperature. Follow guidelines accordingly.
• Wash your hands between clients.
• Place the bulb or probe so that body tissues completely surround it, except for temporal artery.
• When using the tympanic probe, surround it with the skin of the outer ear, rather than the mucous membrane, to minimize the risk of spreading infection.
• Cover temperature probes and multi-use thermometers during use. Slip the cover tightly over the thermometer, take the temperature, and then remove and discard the cover according to facility protocol.
• Pre-lubricated covers are available for rectal thermometers.
• Record the temperature on the client’s graphic record. The electronic thermometer provides a digital readout to one-tenth of a degree. Some special electronic thermometers read the temperature to a more exact measurement.
Oral Temperature
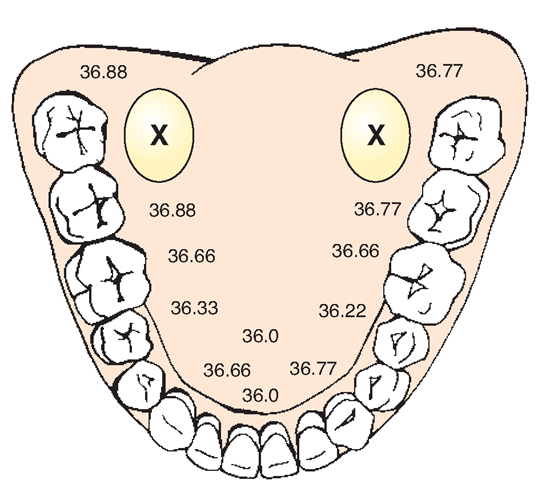
The oral temperature measurement method is fairly easy and comfortable for the client and is frequently used. It measures the temperature within the lingual arteries under the tongue (sublingual) (Fig. 46.5). It is more accurate than axillary and less accurate than rectal measurement.
If a client has had a hot or cold drink or has been smoking, wait 15 minutes before taking an oral temperature. Use of gum and smokeless tobacco can also affect oral temperature. Do not use the oral method for clients who are unconscious, confused, uncooperative, or otherwise not responsible for their actions or those who have an active seizure disorder. This method is also not used with infants or young children. Rationale: All of these clients may accidentally bite the thermometer.
The oral method is also contraindicated in actively suicidal clients; those who have had oral surgery or injury to the nose or mouth; those with conditions in which they must breathe through the mouth; or those who are receiving oxygen. Rationale: The person must be able to keep the sublingual space sealed while the temperature is measured. Use another method to measure the temperature in clients who cannot have oral temperature measurement.
NCLEX Alert During the examination you need to be aware of different ways to obtain VS, as well as the differences in normal/abnormal values and ranges. These will vary for infants, children, adults, and the elderly as well as for different diseases or chronic conditions and injuries.
FIGURE 46-5 · Oral temperature measurements vary with the placement of the probe. Placement in the rear sublingual pocket (shown by the "X”) provides the most accurate measurement. (Measurements shown here are in Celsius.)
Rectal Temperature
The rectal temperature is highly accurate because the probe is placed in an enclosed cavity. If any question arises about the accuracy of an oral temperature, it can be checked against a rectal temperature. Some healthcare agencies have a policy to recheck temperature by the rectal or temporal artery method when the oral reading is above a certain level. A rectal temperature may be used for the client who is unconscious or after mouth surgery. However, tympanic or temporal artery measurements are used more often. The rectal temperature is contraindicated after rectal surgery (and often after vaginal surgery) and in conditions such as diarrhea, colitis, or cancer of the rectum.
Axillary Temperature
The axillary (Ax) temperature is the least accurate measurement because the skin surfaces in the axillary space may not come together to form a tightly closed cavity around the probe tip. Hold the device tightly in place in the client’s armpit when using this method. The axillary method is used frequently for taking the temperature of newborns.For other clients, take axillary temperatures only when conditions make the use of any other method impossible or undesirable.
Tympanic Temperature
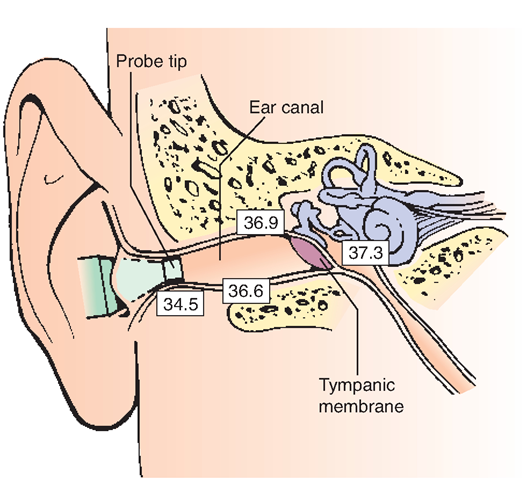
The tympanic thermometer is placed snugly into the client’s outer ear canal. It measures the thermal radiation given off by the tympanic membrane (TM; eardrum) and the ear canal. Because the temperature of the TM’s blood supply is similar to that of the blood surrounding the thalamus (the body’s thermoregulation center), this is an ideal site for measuring the body’s core temperature (Fig. 46-6). The tympanic thermometer records temperature in 1 to 2 seconds. Many pediatric and intensive care units use this type of thermometer because it records a temperature so rapidly. Charge and care for this equipment as you would other electronic thermometers.
FIGURE 46-6 • Obtain the most accurate tympanic temperature by aiming the probe toward the anterior inferior third of the ear canal (toward the jaw line). (Readings here are shown in Celsius.)
Key Concept Crying, ear infections, and ear-wax do not seem to affect tympanic temperature readings.
Nursing Alert When determining body temperature, the technique must be correct to get accurate, reliable results. This is especially true of tympanic temperatures.
Temporal Artery Temperature
A newer method of temperature measurement is the use of the temporal artery (TA) temperature scanner. The TA scanner is moved across the forehead and calculates core body temperature or peak body temperature. This is done by measuring the temperature of the blood in the temporal artery via infrared technology. Figure 46-7 illustrates the temporal artery thermometer. This method is the quickest (almost instant) and most noninvasive method available because the device is not inserted into the body in any way. The TA method can be used in many situations, such as with a sleeping child, an unconscious person, or a person with a hearing aid or an ear infection. It is very helpful when working with clients with special needs or those who are assaultive or tactile defensive (unwilling to be touched). The TA method is being increasingly used in hospitals and is said to be more accurate than the tympanic method and at least as accurate as the rectal method. It is better tolerated than other methods. A probe cover is not necessary, although the device should be cleaned on a regular basis.
FIGURE 46-7 · The temporal artery temperature sensor uses a special scanner to determine body temperature, using the temporal artery in the forehead.
Use of the Glass Thermometer
You may find a glass mercury-containing thermometer in a client’s home. However, as of January 1, 2006, it has been illegal in the United States to sell or distribute thermometers, sphygmomanometers (for measuring blood pressure), or other items containing mercury. In light of this ban, the nurse should take the opportunity for patient education and encourage individuals to dispose properly of any mercury-containing items in their homes.
Key Concept Some pharmacies will allow clients to trade mercury-containing thermometers for safer types. If this service is not available, each mercury-containing item should be sealed in a separate airtight plastic bag, securely wrapped in bubble wrap or another shock-absorbent material, and taken to a hazardous waste collection facility (Call 1-800-RECYCLE to locate the nearest facility.)
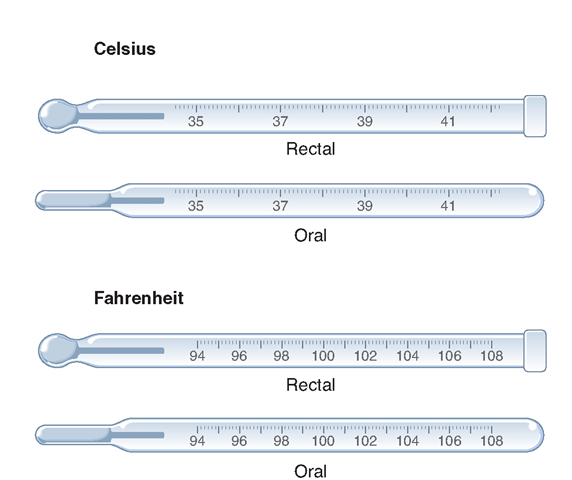
You may also encounter another type of glass thermometer in a healthcare facility, perhaps an extended-care facility. These thermometers contain alcohol, rather than mercury. They are marked with a scale showing whole numbers from 93°F or 94°F to approximately 106°F (or Celsius equivalents), scaled in increments of two tenths (Fig. 46-8). These thermometers may be for oral use (with a slender-tipped end) or rectal use (with a bulb-shaped end).
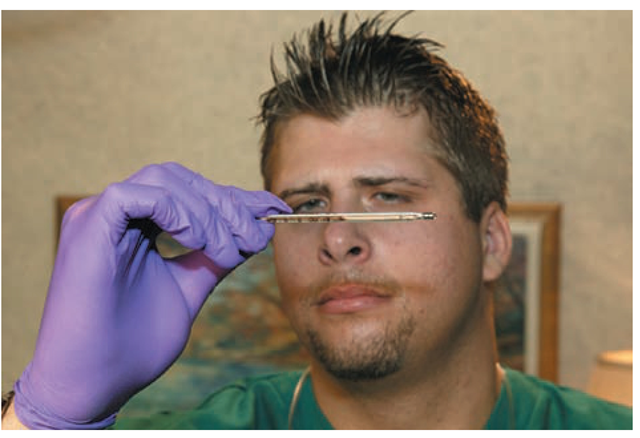
The glass thermometer is fairly difficult to read (Fig. 469). The fluid must be briskly shaken down after each reading. The use and care of glass thermometers is described in In Practice: Nursing Procedure 46-1 and In Practice: Educating the Client 46-1.
FIGURE 46-8 · The glass thermometer may use alcohol to gauge temperature. Shown here are rectal and oral versions of the glass thermometer; calibrated in Celsius and Fahrenheit measurements.
FIGURE 46-9 · To read a glass thermometer, hold it horizontally by the stem at your eye level. Turn it slowly until the alcohol comes into view and you can see the numbers. This thermometer must be shaken down after each measurement.
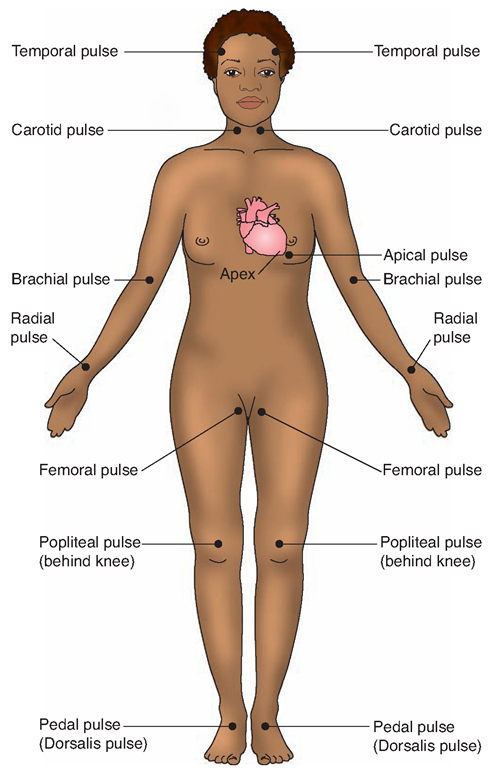
DETERMINING PULSE
Every heartbeat produces a wave of blood that causes pulsations through the arteries. This wave or vibration is called the pulse. The pulse can be felt through the nerves in the fingertips if the fingers are placed over one of the large arteries that lies close to the skin, especially if the artery runs across a bone and has very little soft tissue around it.
The pulse can be felt most distinctly over the:
• Temporal artery just in front of the ear
• Mandibular artery on the lower jawbone
IN PRACTICE: EDUCATING THE CLIENT 46-1
CLEANING AND DISINFECTING THE GLASS THERMOMETER
• Wash your hands and use gloves.
• Wash the thermometer in cold water Rationale: Hot water will break the thermometer.
• Use detergent to remove lubricant from a rectal thermometer before disinfecting. Rub any thermometer with a soap or detergent solution and rinse under cold running water Rationale: Lubricant interferes with disinfectant. Rubbing and soap loosen debris and organisms. Running water helps to rinse away soap residue, which would interfere with disinfection and taste unpleasant. Water also rinses away many microorganisms.
• Dry the thermometer and place it in prescribed disinfectant for the designated length of time. In some cases, thermometers are stored in the disinfecting solution. Be sure to rinse before using. Rationale: Disinfectants have an unpleasant taste.
• Encourage clients to use disposable, plastic thermometer covers, which eliminates the need for disinfection in many situations.
• Sanitize your hands. Properly dispose of gloves.
FIGURE 46-10 · When counting a person’s pulse, it is common to place your fingers on the radial artery (in the wrist). An apical pulse can be counted by placing a stethoscope on the person’s chest, over the apex of the heart.
• Carotid artery on either side of the neck in front
• Femoral artery in the groin
• Radial artery in the wrist at the base of the thumb
Pulses counted in these areas may be stated as temporal pulse, mandibular pulse, carotid pulse, or femoral pulse (Fig. 46-10). If none of these are stated, it is assumed that the pulse was a radial pulse (see Figs. 43-5 and 47-36).
Regulation of Pulse
Pulse Rate
The pulse rate tells how often a person’s heart beats per minute (heart rate, HR). Pulse rate varies with the client’s age, size, and weight. The normal adult pulse rate is 60 to 80 beats per minute (BPM). Women have a slightly higher average rate than men. The pulse of a newborn ranges from 120 to 140 BPM. Rates for children fall between those for adults and newborns, according to each child’s size and age.
Activity affects pulse rate. The heart does not work as hard when a person sleeps; thus, pulse rate decreases. After running, vigorous exercise, or strenuous physical work and during disease, the heart beats faster; thus, the pulse rate increases. Excitement, anger, and fear increase the rate, as do some drugs. The pulse rate is faster in persons with a fever or an overactive thyroid gland. It increases in proportion to the body’s temperature: pulse rate rises about 10 beats for every 1°F (0.56°C) increase in body temperature.
A condition in which the pulse rate is consistently above normal (>100 BPM) is called tachycardia. Many of the previously mentioned conditions cause a temporarily rapid rate. An abnormally rapid rate that persists may signify heart disease, heart failure, hemorrhage, or some other serious disturbance.
Sometimes the pulse rate is continuously slow (<55-60 BPM). This condition is called bradycardia. Well-conditioned athletes often have a pulse rate that is lower than normal, but otherwise, bradycardia often suggests an abnormality. Bradycardia may occur during convalescence from a long feverish illness. It can be a sign of cerebral hemorrhage, indicating increased pressure on the brain. It may also be a sign of complete heart block.Certain medications also lower pulse rate.
Pulse Volume
Pulse volume varies with the blood volume in the arteries, the strength of the heart contractions, and the elasticity of blood vessels. When every beat is full and strong, a normal pulse can be felt with moderate finger pressure (stronger finger pressure obliterates the beats). If a pulse is difficult to obliterate, it is strong and is called full or bounding. In hemorrhage, when a considerable amount of blood has been lost, every pulse beat may be weak or thready and the pulse is easy to obliterate and difficult to feel.
Pulse Rhythm
Pulse rhythm is the spacing of the beats. With normal or regular rhythm, intervals between beats are the same. When the pulse occasionally skips a beat, this irregularity is described as an intermittent or irregular pulse. A pulse may be regular in rhythm, but irregular in force; that is, every other beat is weak. These beats may be so weak that they are not felt in the radial (wrist) pulse at all. This finding is serious because it means the heart is actually beating twice as fast as the radial pulse rate indicates. This condition can be detected by measurement of the apical-radial pulse (simultaneous measurement of the apical and the radial pulse), discussed later in this topic. Pulse may be irregular in force and rhythm (dysrhythmia), a sign of some forms of heart disease or of an overactive thyroid gland.
Methods and Equipment
Palpation
Palpation (feeling with the fingers) is used to assess the radial, temporal, mandibular, carotid, and femoral pulses. To locate the area of strongest pulsation, palpate the client’s pulse with your first, second, and third fingers of one hand. (Do not use the thumb, which has its own pulse.) Count the initial pulsation as zero. The pulse rate is expressed in beats per minute.
Auscultation With a Stethoscope
Auscultation (listening to sounds) and counting the apical pulse, normally heard at the heart’s apex, will usually give the most accurate assessment of pulse rate. For this assessment, use an instrument called a stethoscope, which amplifies sounds received in the head of the instrument as they pass through the earpieces (Fig. 46-11). Most stethoscopes have two heads: the diaphragm and the bell. The flat diaphragm is pressed against the skin to test high-frequency sounds: breath, normal heart, and bowel sounds. The cup-shaped bell is pressed lightly on the skin to collect low-frequency sounds, such as abnormal heart sounds. (To change from one head to the other, turn the head until it clicks into place.)
The diaphragm of the stethoscope is placed over the heart’s apex to assess apical pulse. (The apical pulse can be palpated with the fingers in about 50% of adults.) The apex of the heart is the point of maximal impulse (PMI) and is the location where the apical pulse is best heard. Each heartbeat consists of two sounds. S1, the first sound, is caused by closure of the mitral and bicuspid valves, which separate the atria from the ventricles. S2, the second sound, is caused by the closure of the pulmonic and aortic valves. The result is a muffled “lub-dub” sound, which constitutes one heartbeat.