Learning Objectives
1. Identify the organs of the urinary system on an anatomical chart or model.
2. Describe the anatomy and physiology of the nephron.
3. Explain how the urinary system influences homeostasis.
4. Describe the functions of the two hormones secreted by the kidneys.
5. Explain how the kidney, ANP, and the RAA system impact red blood cells, blood pressure, water and electrolyte balance, acid-base balance, and vitamin D synthesis.
6. Describe blood supply to, within, and from the kidneys.
7. Illustrate the pathway of waste products from the blood to the external environment.
8. Describe the formation of urine. Include the concepts of glomerular filtration, tubular reabsorption, and tubular secretion.
9. Describe the chemical differences between plasma, glomerular filtrate, and urine.
10. Compare and contrast micturition and incontinence.
11. List the characteristics and usual components of normal urine.
12. Describe three effects of aging on the urinary system and the nursing implications related to these effects.
|
IMPORTANT TERMINOLOGY |
||
|
bladder |
loop of Henle |
renin |
|
Bowman’s capsule |
micturition |
ureter |
|
calyx |
nephron |
urethra |
|
convoluted tubule |
nocturia |
urination |
|
erythropoietin |
renal cortex |
urology |
|
glomerulus |
renal medulla |
void |
|
kidney |
renal threshold |
|
|
Acronyms |
|
|
DCT |
PCT |
|
GFR |
TM |
|
JGA |
As the body builds and repairs tissues and produces energy for life processes, waste products form that must be removed. Through the activities of perspiring and breathing, the integumentary and respiratory systems remove some water, carbon dioxide, and nitrogenous wastes. Through defecation, the digestive system removes the bulk of food wastes.
Another system, the urinary or excretory system, is also involved in waste removal. (This system is sometimes combined with the male reproductive system and known as the genitourinary system—GUS.) Circulating blood carries wastes from the cells to the kidneys for urinary elimination. Consequently, the urinary system is sometimes called the body’s “filtration and removal plant.” Much of the material removed by the kidneys is water, although many solid wastes are dissolved or are in suspension in urine. Uro- is the word element referring to urine. A specialist who deals with the female urinary system and the male genitourinary system is the urologist; the related science is urology. Although the anatomy of the urinary system is relatively simple, its action and influence on the body’s total wellbeing are complex. The urinary system greatly influences the body’s homeostasis.
Key Concept The urinary system plays a vital part in the maintenance of homeostasis in the body. It produces, stores, and eliminates urine and wastes.
Structure and Function
The major structures of the urinary system are:
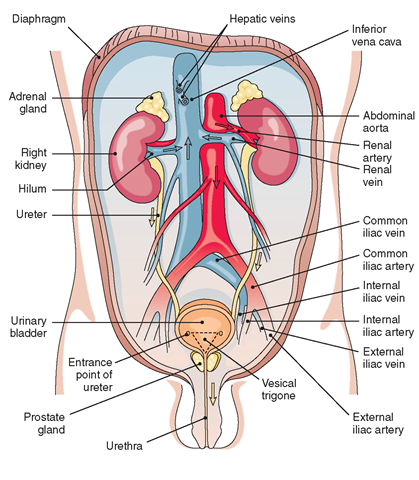
• Two kidneys extract wastes from the blood, balance body fluids, and form urine.
• Two ureters conduct urine from the kidneys to the urinary bladder.
• The urinary bladder serves as a reservoir for urine.
• The urethra conducts urine from the bladder to the outside of the body for elimination.
The urinary system is able to adapt to wide variations in dietary and fluid intake. It also adjusts and maintains the composition of blood, tissue fluids, and interstitial fluids. The volume of circulating fluids in the bloodstream affects blood pressure. The urinary system helps control blood volume by excreting or conserving water. (An accumulation of water in tissues is known as edema (see Fig. 76-2); an abnormal decrease is known as dehydration). By excreting or conserving minerals (especially sodium and chlorine) as necessary, the urinary system regulates specific levels of electrolytes in body tissues and fluids. Box 27-1 summarizes the functions of the urinary system.
KIDNEYS
The kidneys are two reddish-brown, bean-shaped organs located in the small of the back at the lower edge of the ribs on either side of the vertebral column (Fig. 27-1). They are about the size of a human fist (about 4 inches [10 cm] long, 2 inches [5 cm] wide, and 1 inch [2.5 cm] thick. On top of each kidney is an adrenal gland (ad = near).
BOX 27-1.
Functions of the Urinary System
Maintenance of Homeostasis
♦ Controls water and blood volume
♦ Maintains blood pressure
♦ Regulates electrolyte levels; reabsorbs some electrolytes
♦ Maintains pH balance
♦ Activates vitamin D (for bone calcification)
Manufacture
♦ Secretes renin and erythropoietin
Processing of Wastes
♦ Forms urine (kidneys)
♦ Stores urine (bladder)
Elimination
♦ Eliminates protein wastes, excess salts, and toxic materials
The kidneys are said to be retroperitoneal because they lie behind the peritoneum. Kidney location is important because it enables kidney surgery to be performed from the back, without entrance into the abdominal cavity. The right kidney is slightly lower than the left, because the liver takes up space on the body’s right side.
FIGURE 27-1 · The male urinary system, with blood vessels, as viewed from the front. Yellow arrows indicate direction of urine flow. Red and blue arrows indicate direction of blood flow into and out of the kidney.The renal artery branches directly off the aorta.
A person can easily live with one kidney. Ren- is the prefix related to kidneys; renal is the descriptive term used. The word element referring to the kidney is nephr(o-).
The kidneys are extremely vascular (heavily supplied with blood vessels). Blood supply is necessary so the kidneys can do the essential work of waste removal. Every day, approximately 10% of circulating blood in the entire body circulates through the kidneys. Each kidney is surrounded by peri-nephric (around the kidney) fat, and is surrounded by a fibrous capsule. The fibrous capsule continues downward, forming the outer layer of the ureter covering. The fatty pads, plus renal fascia, which is anchored to surrounding tissues, help hold the kidneys in place. On the medial surface of each kidney (toward the middle of the body) is an indented area called the hilum, a notch through which the blood vessels, nerves, and ureter enter.
The kidneys can precisely regulate and adjust electrolyte levels. By regulating sodium chloride (NaCl) levels, they control the volume of body fluids. They balance pH in the blood, body fluids, and within body tissues. The kidneys do this by eliminating acids directly into the urine or by excreting acids bound to chemical buffers. These buffers change strong acids into weaker acids, which enables the kidneys to excrete large amounts of acid without dramatically altering (or lowering) urine pH. However, urine is 1,000 times more acidic than blood. Other major functions of the kidneys include hormonal secretion of renin and erythropoietin, and activation of vitamin D.
Special Considerations :NUTRITION
Urine Acidity and Alkalinity
Urine is normally acidic, with a pH of about 6 (pH range: 4.5-8). Foods ingested can alter the acidity or alkalinity of urine. Foods that will acidify urine are: cranberries, meat, and a high-protein diet. Foods that will alkalinize urine are: citrus fruits, dairy products, and legumes. Foods ingested can also alter the odor of urine. Certain foods and medications alter the color of urine.
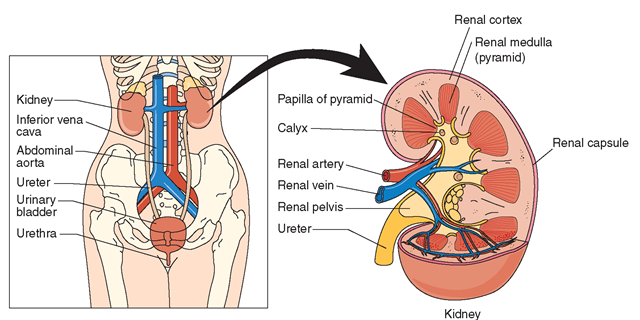
If the kidney is cut in half longitudinally, you can see that it is divided into two parts: the outside called the cortex and the inner portion called the medulla (“middle”). The renal cortex is the outer reddish-brown part of the kidney that extends from the outside of the kidney (renal capsule) to the bases of the renal pyramids and into the spaces between them (Fig. 27-2). The renal corpuscles (glomeruli and Bowman’s capsules) and the proximal and distal portions of the convoluted tubules make up the major portion of the renal cortex (see “Nephrons” section and Fig. 27-3).
The renal medulla contains the remainder of the renal tubules, loops of Henle, and collecting tubules. These tubules form a number of cone-shaped structures called renal pyramids. These pyramids are arranged so their bases are on the outside near the renal cortex. The tips (renal papillae) of the renal pyramids point medially toward the renal pelvis, which is a funnel-shaped basin at the upper end of the ureter. Urine flows from the collecting tubules through the pyramids and into cup-like extensions of the renal pelvis. These extensions are called calyces (singular: calyx).
Table 27-1 summarizes the key information about the renal cortex and the renal medulla, for easy reference.
Nephrons
The major role of the kidneys is to filter water-soluble wastes out of the blood. Nephrons (from Greek: nephros = kidney) are the functional units of the kidney. They are the cells that form urine; the rest of the urinary system expels urine. More than 1 million microscopic nephrons are in each kidney. Human beings can survive using only one third of their nephrons.
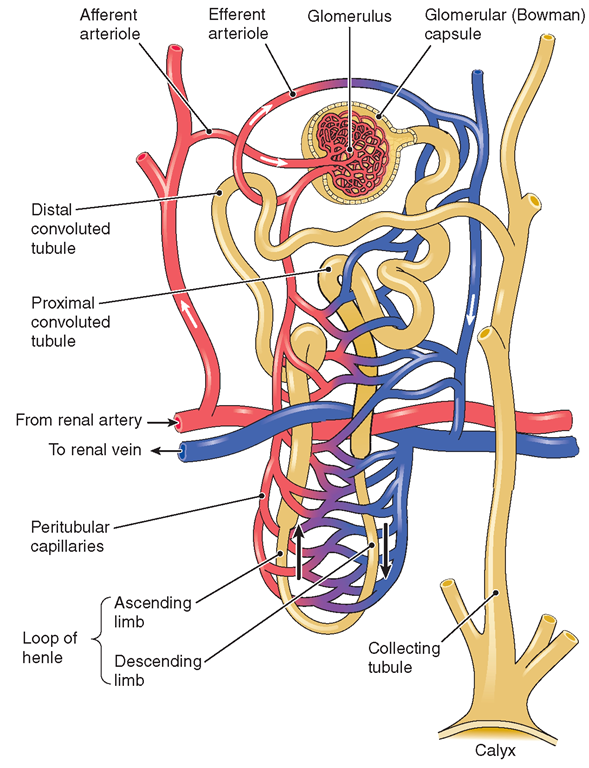
The largest portion of each nephron is located in the renal cortex (superficial and midcortical nephrons), except for a small tube located in the medulla. Juxtamedullary nephrons are those near the medulla. At one end of each microscopic nephron is a knotted cluster or tuft of capillaries called the glomerulus (plural: glomeruli; from Latin glomus = ball).
FIGURE 27-2 · Internal structure of the kidney and blood vessels, and location in the female body.
FIGURE 27-3 · A nephron. Each kidney has about 1 million nephrons, which take two forms: cortical and jux-tamedullary Cortical nephrons are located in the cortex of the kidney; juxtamedullary nephrons are adjacent to the medulla.
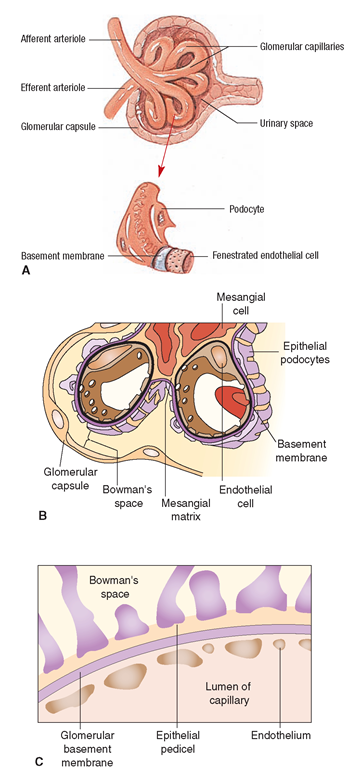
These capillary loops are supported by a thin membrane called the mesangium (see Fig. 27-4B). The glomerulus is partially enclosed in a funnel-shaped structure called Bowman’s capsule (Bowman’s space, glomerular capsule) (see Fig. 27-3), which pressure-filters large solutes out of the blood through small pores. The glomerulus and Bowman’s capsule together are known as the renal corpuscle (or malpighian corpuscle). This renal corpuscle is the beginning of the nephron. Because the efferent arteriole (the one leaving the glomerulus) is smaller in diameter than the afferent arteriole, the pressure in the glomerulus is increased. This assists in the pressure filtration of molecules out of plasma.
The walls of the glomeruli have three layers that filter blood (Fig. 27-4B,C). The outside layer of the glomerular membrane is the epithelium.
TABLE 27-1. Renal Cortex and Renal Medulla
|
RENAL CORTEX |
RENAL MEDULLA |
|
♦ Bowman’s capsule |
♦ Remainder of the renal tubules |
|
♦ Glomerulus |
♦ Loop of Henle |
|
♦ PCT (proximal convoluted tubule) |
♦ Collecting tubules (ducts) |
|
♦ DCT (distal convoluted tubule) |
o \ J (make up renal pyramids) |
|
♦ Largest part of each nephron |
♦ Renal pyramids |
This layer has large openings (pores) that allow all blood components, except RBCs, to pass through until they reach the middle layer, called the basement membrane. The basement membrane prevents the passage of large proteins through it by filtration. From there, the filtered substances go to the inner layer of the glomerular membrane, the endothelium. A peri-tubular (around the tubes) capillary network surrounds the nephron and supplies it with blood (see Fig. 27-3). Glucose and oxygen are brought in and reabsorbed nutrients and water are removed.
The epithelium (outside layer), also called the capsular membrane, is a thin and porous membrane, which covers the basement membrane. This epithelial membrane is made up of specialized cells called podocytes, which have “extensions” branching out on the basement membrane surface. These extensions are called pedicels. Spaces between the pedicels restrict medium-sized proteins from entering the glomerular filtrate. Several disease processes—such as glomerulonephritis and diabetic nephropathy—can cause alteration in the basement membrane, thereby reducing the filtering ability of the kidneys.
Blood, with its filterable wastes and food products, enters the glomerulus through the afferent arteriole, which divides to form the capillary loop (Fig. 27-4A). Water, wastes, glucose, and salts filter through the thin walls of the glomerulus as described above, and then enter Bowman’s capsule in a dilute solution. The capillaries of the glomerulus unite to form the efferent arteriole, which carries away the remaining blood.
FIGURE 27-4 · Renal corpuscle. (A) Structures of the glomerulus. (Source: Atlas of Human Anatomy, 2001.) (B) Position of the mesangial cells in relation to the capillary loops and Bowman’s capsule. (C) Cross-section of the glomerular membrane, showing the position of the epithelium (with epithelial pedicels), basement membrane, and endothelium.
Extending from Bowman’s capsule is a long twisted tube called the convoluted tubule (or renal tubule) (see Fig. 27-3).
TABLE 27-2. Nephron Structures and Their Functions
|
STRUCTURE |
FUNCTION |
|
Glomerulus and Bowman’s capsule |
Filters water, wastes (urea), glucose, and salts (electrolytes) out of blood (filtrate consists of water plus all non-protein components of the plasma) |
|
Convoluted tubules Proximal convoluted tubule |
Reabsorbs some needed electrolytes (potassium, chlorine), water, and glucose, as well as some amino acids and bicarbonate |
|
Loop of Henle Distal convoluted tubule |
Reabsorbs water and additional electrolytes Reabsorbs sodium, water, and remainder of glucose |
The first portion is the proximal convoluted tubule (PCT). Here, glucose, amino acids, and salts are actively transported across membranes and returned to the blood. This tubule accomplishes the process of selective reabsorption because it contains a brush border with many villi. Adenosine triphosphate (ATP) is also produced by mitochondria here, to assist in the active transport. The next portion of the convoluted tubule is the loop of Henle (nephron loop), the major function of which is to concentrate salts by reabsorbing water (by osmosis). The final portion (which is the end of the nephron unit) is the distal convoluted tubule (DCT). This is the site of tubular secretion. Molecules secreted here include creatinine and hydrogen ions. Fluids filtered through the glomerulus, with their dissolved contents, travel the length of these renal tubules.
The juxtaglomerular apparatus (JGA) or juxtaglomerulus, which consists of specialized glandular cells responsible for maintaining blood pressure, lies at the point where the distal convoluted tubule contacts the afferent arteriole. (Blood pressure regulation is discussed later in this topic.)
After the blood leaves the DCT, it moves to the collecting tubule or duct system (medullary collecting duct or collecting duct), where the antidiuretic hormone (ADH) exerts its effects to allow the tubule to become more or less permeable to water. (The actions of this hormone are described in the next section.) Therefore, the collecting tubule is an important regulator in concentration or dilution of urine. The peritubular capillaries reabsorb much of the water and salts and all of the glucose. The urine, with its waste products, then continues through the renal pyramid to the renal pelvis and onward to the ureter and bladder. Table 27-2 summarizes nephron structures and their functions.
Key Concept Pathway of urine in the kidney:
Afferent arteriole S glomerulus and Bowman’s capsule S proximal convoluted tubule S loop of Henle (descending limb—permeable to water; impermeable to salts, and ascending limb—impermeable to water, pumps sodium out of filtrate) S distal convoluted tubule (with parathyroid hormone, reabsorbs calcium, excretes phosphate; with aldosterone, reabsorbs sodium, excretes potassium; also regulates pH with hydrogen and ammonium) S juxtaglomerular apparatus (end of nephron) S collecting duct system.
Role of Hormones and Other Substances
The kidneys secrete two hormones: renin and erythropoietin.