LOWER RESPIRATORY TRACT
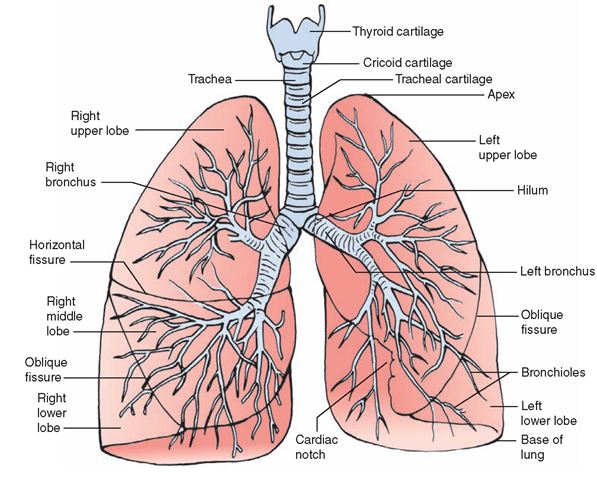
Figure 25-3 illustrates the lower respiratory tract. It consists of the bronchi and lungs.
Bronchi
As the trachea enters the chest cavity, it divides into two smaller tubes called the bronchi. There is an indented area, called the hilum, where each bronchus enters the lung and branches off. The arteries, veins, and nerves enter the lungs at the hilum as well. One (primary) bronchus enters each lung. The right bronchus is shorter, straighter, and wider than the left bronchus. The cartilage in the small bronchi within the lungs exists as interspersed plates, rather than rings. There is more elastic tissue here as well. The bronchi and bronchioles are encircled by smooth muscles.
Nursing Alert Because the right bronchus is shorter straighter down, and wider than the left, it is more easily accessible. Therefore, the right bronchus is more susceptible to aspiration of fluids or foreign objects.
The Tracheobronchial Tree
Each bronchus continues to divide into smaller branches to form what commonly is called the bronchial tree or tracheobronchial tree. This bronchial tree spreads throughout the lung tissue. As the bronchi become smaller, their walls become thinner, the amount of cartilage decreases, and they become known as bronchioles. The bronchi and bronchioles continue to be lined with ciliated mucous membrane. The bronchioles branch first into alveolar ducts, which look like stems, and end in many alveolar sacs, which look like clusters of grapes (see Fig. 25-1). Each lung contains millions of these alveoli. These microscopic “balloons” give the lungs their spongy appearance. The walls of the alveoli are composed of a single layer of cells and are lined with a chemical called surfactant, which helps to prevent the alveolar walls from collapsing between breaths.
FIGURE 25-3 · The lower respiratory tract viewed from the front. The lungs consist of five lobes.The right lung has three lobes (upper, middle, lower); the left has two (upper and lower). The left lung has an indentation called the cardiac notch, which provides space for the heart.The pulmonary lobes are further subdivided by fissures. The bronchial tree inflates with air to fill the lobes.
Surfactant
Surfactant is a substance secreted by the great alveolar cells (type II cells) of the lungs and is a mixture of phospholipids (a special type of fat that also contains phosphorus). The main phospholipids in surfactant are lecithin and sphingomyelin. The surfactant in the lungs acts to break up the surface tension in the pulmonary (lung) fluids, much like laundry detergent breaks up dirt and grease particles. This reduces friction and preserves the elastic property of lung tissue, thus preventing collapse of the alveolar walls between breaths.
Special Considerations : LIFESPAN
Surfactant
Surfactant does not form until after the seventh gestational month. Premature newborns may have insufficient surfactant, which results in collapse of the alveoli. A newborn with this problem (called respiratory distress syndrome—RDS or hyaline membrane disease) must exert tremendous energy to breathe. As a result, the infant may die owing to fatigue of the respiratory muscles and inadequate ventila-tion.Treatment involves the use of mechanical ventilation and administration of synthetic surfactant.
Lungs
Humans have two cone-shaped lungs that fill the chest cavity. They are the stations where oxygen is delivered from the outside air and carbon dioxide is removed. The top of each triangular cone is called the apex. The lower, wide portion that fits over the diaphragm is called the base. Each lung has an area called the cardiac notch or cardiac impression,much larger and deeper on the left because of the position of the heart. The lungs are spongy tissue filled with alveoli, nerves, and blood and lymph vessels. They are separated by the heart, the large blood vessels, the esophagus, and other contents of the mediastinum, the area lying between the lungs in the thorax (chest). The lungs are divided into sections called lobes. The right lung has three lobes, and the left has two (see Fig. 25-3).
Pleura
The lower respiratory tract contains a smooth doublelayered sac of serous membrane called pleura (see Fig. 25-1). The inner layer covers the lungs (the visceral pleura), and the outer layer (the parietal pleura) lines the chest cavity. Their surfaces are in constant contact and are moist because they secrete serous lubricating fluid. The pleura allow the lungs to move without causing pain or friction against the chest wall. The space between the two layers of the pleura is called the pleural cavity or pleural space. A vacuum normally exists within this space. This vacuum changes in intensity during breathing.
Key Concept Pleurisy is an inflammation of the pleura, causing a "sticking" pain on inspiration. It can be caused by conditions such as a lung tumor, tuberculosis, lung abscess, or pneumonia.
The respiratory tract is lined with epithelium, the type of which depends on location. Most of the tube system, from the nose to the bronchi, is covered by pseudostratified columnar ciliated epithelium (respiratory epithelium). In the bronchioles, the cells become more cuboidal in shape, but continue to be ciliated.
Nursing Alert Air or fluid accumulation in the pleural space can cause lung collapse, an airless situation (atelectasis). The collapse may involve all or part of a lobe or an entire lung; atelectasis may be acute or chronic.
System Physiology
BREATHING
Ventilation (breathing) is the mechanical process of respiration that moves air to and from the alveoli. Ventilation is divided into inhalation and exhalation. Breathing air in is called inhalation or inspiration; breathing out is called exhalation or expiration. One ventilation or respiration takes about 2 seconds. Adults usually average between 12 and 20 respirations per minute; the rate is higher in children, lowering as the child becomes older. Normal respiration is called eupnea; difficult breathing is known as dyspnea. Orthopnea denotes dyspnea that is relieved when the person sits up.
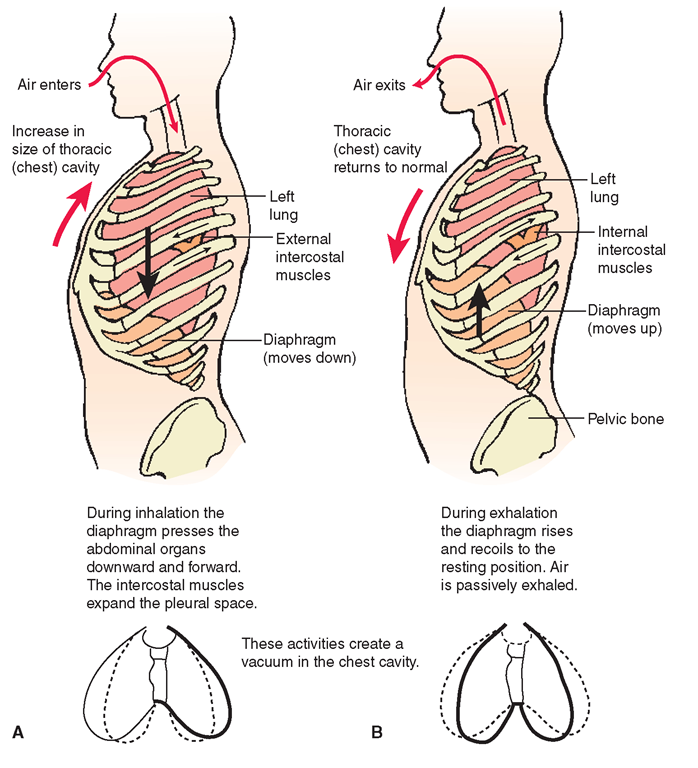
Normal breathing occurs as a result of nervous stimulation of the respiratory center in the brain’s medulla. Because the lungs cannot move by themselves, the actions of the muscles surrounding them inflate and deflate them. The medulla sends impulses to the diaphragm and the intercostal muscles. The diaphragm is a dome-shaped muscle separating the thoracic and abdominal cavities. It contracts and flattens to increase both the chest (pleural) space and the pleural vacuum (Fig. 25-4). The intercostal muscles are located between the ribs; they contract to lift and spread the ribs during inhalation, adding to the vacuum.
The actual movement of air from the external to the internal environment occurs as a result of differences in existing pressures between the atmosphere and the chest cavity. On inspiration, the chest cavity increases in size, creating an internal vacuum. Air goes into the lungs when the intratho-racic (within the thoracic cavity) pressure is below that of the surrounding atmosphere (subatmospheric pressure).
Nursing Alert Any interruption in the closed chest can be immediately life-threatening because it disrupts the vacuum necessary for inspiration. Therefore, a puncture wound or other opening into the chest must be immediately plugged, to prevent death.
FIGURE 25-4 · Pulmonary ventilation. (A) Inhalation (inspiration). (B) Exhalation (expiration).
Key Concept If breathing becomes difficult,accessory muscles (e.g., the sternocleidomastoid and neck muscles) are used to assist. Movement of these muscles can be visualized and is particularly diagnostic of respiratory distress in infants and small children.
Expiration is a passive process. On expiration, the muscles of the chest wall and lungs relax. Movements of the diaphragm and the intercostal muscles cause the volume of the thoracic cavity to become smaller. Air rushes out when the pressures within the thoracic cavity rise above that of the atmosphere. In addition, the reduced size of the thoracic cavity and natural elasticity of the lungs force the air out.
Key Concept During forced exhalation, such as when blowing up a balloon or playing a musical instrument, abdominal and thoracic pressure is consciously generated by muscle movement, forcing air out of the lungs.
Regulation of Respirations
The medulla’s respiratory center automatically controls the depth and rate of respirations without requiring a person’s conscious thought. The pons has centers that work with the medulla to produce a normal breathing rhythm. The cerebral cortex allows some voluntary control over breathing when talking, singing, eating, or changing the rate of breathing. You can even stop breathing for a minute or two by holding your breath. The medulla, however, will take over control eventually. Chemoreceptors in the medulla stimulate the muscles of respiration primarily in response to changes in carbon dioxide levels. Therefore, carbon dioxide—not oxygen—is the major regulator of respiration.
Key Concept An excess of carbon dioxide in the blood of a healthy person lowers the pH of the blood.This drop in pH leads to stimulation of the medulla to increase respirations, which provides a means for blowing off excess carbon dioxide.
Nursing Alert Certain portions of the brain stem are particularly sensitive during infancy; neurons can be destroyed if the child is shaken violently or dropped. This results in "shaken baby syndrome” and can lead to death. A spinal cord injury at the level of the brain stem is often fatal at any age.
Lung Volumes and Capacities
Lung capacity varies with sex, size, physical condition, and age. Pulmonary diseases and other diseases that limit expansion of the chest cavity greatly influence a person’s comfort and ability to survive. The ability of the lungs and thorax to expand also influences lung volumes and capacities. Table 25-1 contains key terms, descriptions, and normal values for a healthy male adult. (The values for women are 20%-25% lower.)
Key Concept It is important to note that,even after expiration, some air (residual) remains in the lungs. This is the basis for the Heimlich maneuver used in choking victims.
INTERNAL (TISSUE) AND EXTERNAL (PULMONARY) RESPIRATION
The two types of respiration are external and internal. The exchange of oxygen (O2) for carbon dioxide (CO2) within the alveoli of the lungs is called external respiration (pulmonary respiration) because it is the part of the respiratory cycle involved with the external environment (Figure 17-3 illustrates this gas exchange. Notice the difference in pressures between the non-oxygenated blood and the oxygenated blood.) After oxygen is brought into the body, it attaches to hemoglobin for transport to tissues and cells. The exchange of oxygen (O2) for carbon dioxide (CO2) within the cells is called internal respiration or cellular respiration (cell breathing). An increase in carbon dioxide levels stimulates respiration. Carbon dioxide and water are the waste products of respiration. Some water is excreted as waste; some is recycled for use in the body.
* Key Concept Respiration is the exchange of gases between a person’s external environment and internal cells.
External respiration is gas exchange at the lung level. Internal respiration is gas exchange at the cellular level.
For the respiratory system to function, it must remain moist (to dissolve gases), its cells must be thin (to allow for gas transfer), there must be a source of oxygen, and the respiratory system must communicate with the circulatory system.
Gas Exchange
Non-oxygenated blood from the right ventricle of the heart flows into the pulmonary artery, which branches into right and left segments. Further branching leads to pulmonary and bronchial capillaries in the lungs where an exchange of gases (oxygen and carbon dioxide) occurs via diffusion through the alveoli, the functional structures of the lungs.The walls of the alveoli are made up of one cell-layer of epithelial cells (approximately 0.2 μm). The alveoli are surrounded by equally thin capillaries, a single endothelial cell thick. The extensive branching of pulmonary blood vessels leads to a low pressure within the vessels, facilitating the exchange of gases.
TABLE 25-1. Lung Volumes and Lung Capacities
|
TERM |
SYMBOL |
DESCRIPTION |
NORMAL VALUE* |
SIGNIFICANCE |
|
Lung Volumes Tidal volume |
Vt or TV |
The volume of air inhaled and exhaled with each breath |
500 mL or 5-10 mM<g |
The tidal volume may not vary, even with severe disease. |
|
Inspiratory reserve volume |
IRV |
The maximum volume of air that can be inhaled after a normal inhalation |
3,000 mL |
A sigh takes advantage of the IRV potential. |
|
Expiratory reserve volume |
ERV |
The maximum volume of air that can be exhaled forcibly after a normal exhalation |
1,100 mL |
Expiratory reserve volume is decreased in restrictive disorders, such as obesity, ascites, and pregnancy. |
|
Residual volume |
RV |
The volume of air remaining in the lungs after a maximum exhalation |
1,200 mL |
Residual volume may be increased in obstructive disease. |
|
Lung Capacities Vital capacity |
VC |
The maximum volume of air exhaled from the point of maximum inspiration VC = TV + IRV + ERV |
4,600 mL |
A decrease in vital capacity may be found in neuromuscular disease, generalized fatigue, atelectasis, pulmonary edema, and COPD. |
|
Inspiratory capacity |
IC |
The maximum volume of air inhaled after normal expiration IC = TV + IRV |
3,500 mL |
A decrease in inspiratory capacity may indicate restrictive disease. |
|
Functional residual capacity |
FRC |
The volume of air remaining in the lungs after a normal expiration FRC = ERV + RV |
2,300 mL |
Functional residual capacity may be increased in COPD and decreased in ARDS. |
|
Total lung capacity |
TLC |
The volume of air in the lungs after a maximum inspiration TLC = TV + IRV + ERV + RV |
5,800 mL |
Total lung capacity may be decreased in restrictive disease (atelectasis, pneumonia) and increased in COPD. |
COPD, chronic obstructive pulmonary disease; ARDS, acute respiratory distress syndrome.
*Values for healthy men; values for women are 20%-25% less.
When oxygen enters the lungs, it travels through the walls of the alveoli into the capillaries in the lungs (see Fig. 25-1). At the capillary level, oxygen diffuses into the capillaries and is bound to hemoglobin (in red blood cells) in capillary blood. Small veins collect the now-oxygenated blood from the lung capillaries. These veins combine eventually into four pulmonary veins (two left, two right), which pour oxygenated blood into the left atrium of the heart. (The blood in the left atrium is pumped through the left ventricle and through the aorta out to the rest of the body. This oxygenated blood then travels to tissues where the oxygen-hemoglobin bond is broken easily and oxygen is released into tissues.)
In the lungs, at the same time oxygen is diffusing from the outside air via the alveoli into the capillaries, the capillaries are giving up carbon dioxide (received from body tissues) back into the alveoli. Carbon dioxide is a waste product of metabolism or work the body is performing. It is transported by the blood from the body’s cells to pulmonary capillaries in three main forms: dissolution in plasma, in combination with proteins, or by formation into bicarbonate (HCO3) ions in the blood. The bicarbonate ions undergo a chemical change which yields carbon dioxide (CO2) and water (H2O). During exhalation, this carbon dioxide and some of the water is released from the lungs into the air. This cycle then begins again and continues to maintain homeostasis and electrolyte balance in the body.
* Key Concept In the average resting adult, 250 mL of oxygen is taken in per minute; about 200 mL of carbon dioxide is expelled.
Chemical messengers, such as hormones, are also deleted and added in the lungs. Small blood clots are removed by the fine capillaries in the lungs.
Nearly all the blood in the body travels through the lungs every minute.
Nursing Alert Many factors can cause a decrease in gas exchange, including immobility thoracic/pulmonary surgery or pneumonia. Encouraging frequent coughing and deep breathing exercises should assist in improving oxygen delivery to the lungs and tissues. Supplemental oxygen may also be ordered to improve arterial oxygen levels (O2 saturation).