ACCESSORY GLANDS
Seminal Vesicles
The two seminal vesicles are convoluted, sac-shaped glands about 2 inches (5 cm) long, which are located posterior to the urinary bladder. They secrete a sticky, alkaline, yellowish substance, called semen, which serves as a fluid medium for sperm. Seminal vesicles secrete about 60% of all of a man’s semen. The content of semen is described later.
Prostate Gland
The prostate is a doughnut-shaped muscular structure just larger than a walnut, lying just below the bladder. It surrounds the neck of the urethra as the urethra emerges from the bladder (see Fig. 28-1). Glandular prostate tissue adds an alkaline secretion to semen, which increases sperm motility. The muscular portion of the prostate contracts during ejaculation to expel semen from the urethra.
Special Considerations :LIFESPAN
Prostate Removal
Some men are unable to have an erection or to ejaculate after prostate removal because of tissue and nerve damage or because too much muscle tissue had to be removed. A “nerve-sparing” surgical procedure is sometimes successful in maintaining potency after surgery. Medications are sometimes helpful as well.
NCLEX Alert Several changes in the reproductive system are normal as the individual ages. You should be aware of both normal and abnormal conditions of the reproductive system, which may be integrated into a clinical scenario on the NCLEX.
Bulbourethral Glands
The bulbourethral (Cowper’s) glands are located between two layers of fascia just below the prostate glands. Approximately the size of a pea, they are composed of several lobules held together by fibers. They secrete an alkaline mucus into tiny ducts, which empty into the urethra. This mucus coats the urethra to neutralize the pH of urine residue; it also lubricates the penis. Sperm survive better in an alkaline medium than in acid; alkalinity helps maintain sperm motility. A woman’s vagina is acidic because of its normal flora (natural bacterial population). The alkaline environment of seminal fluid helps to neutralize the acidic vaginal pH and to maintain sperm motility and viability.
HORMONAL INFLUENCES
The male reproductive system develops during childhood and adolescence. It does not become functional until hormones are secreted during puberty (pubescence), the stage of life during which the reproductive organs become fully functional.In boys, puberty usually occurs between 12 and 16 years of age. Hormones from the hypothalamus, pituitary gland, and gonads influence the reproductive system. Before puberty (prepubescence), the blood concentrations of androgens (male hormones) and estrogens (female hormones) are the same in every person.
The fetal precursor of specific male gonads is the Wolffian duct, which develops into the epididymis, vas deferens, ductus deferens, ejaculatory duct, and seminal vesicles. Endocrine hormones control the differences between the male and female reproductive systems. When a boy reaches puberty, the hypothalamus stimulates the secretion of both interstitial cell-stimulating hormone (ICSH) and follicle-stimulating hormone (FSH) from the anterior pituitary;both are gonadotropic hormones. In the man, these hormones have two main effects:
• They stimulate the gonads (sex glands) to secrete specific male hormones (androgens).
• FSH stimulates the formation of sperm.
The major androgen is testosterone. ICSH stimulates the production of testosterone. During puberty, male glandular development becomes very active and influences development of secondary sexual characteristics. These include the typical male beard, pubic, and axillary hair, as well as increased body hair. Unique musculature develops. The shoulders become broader; the hips remain narrow. The voice deepens and the “Adam’s apple” develops in the anterior throat. (The “Adam’s apple” is unique to the male.) Testosterone also maintains the functioning of male accessory organs and stimulates protein anabolism. As a result, a man has larger and stronger musculature than a woman.
Key Concept If a man receives testosterone replacement therapy the testes will shrink because they are no longer required to manufacture testosterone. Pituitary gonadotropin drugs will cause the testes to enlarge. Disorders of the testes include undescended testicles, injury orchitis (inflammation), cancer hydrocele (fluid around the testis), and spermatic cord torsion (twisting). Any of these can influence sperm production and fertility. Removal or failure of both testes is called castration, which renders the man sterile and will require external testosterone to maintain male characteristics.
System Physiology
SPERM CELLS AND SPERMATOGENESIS
Beginning when a male is about 12-13 years of age and continuing throughout life, the seminiferous tubules of the testes (the male gonads), stimulated by testosterone, form sperm cells. The sperm cell (plural is also sperm) is the male gamete, one of two cells that must unite to initiate development of a new individual. This formation of mature and functional spermatozoa is called spermatogenesis. Normal spermatogenesis does not occur if the testes are too warm or too cold (above or below 35°C [95°F]), as described above.
Nursing Alert Certain illnesses, notably mumps, can cause reproductive difficulties in males. About one third of males who contract mumps after puberty develop orchitis (inflammation of the testes). This often results in sterility emphasizing the need for immunization of infants against mumps.
The stem cells of sperm cell development are called spermatogonia (singular: spermatogonium). A “mother cell” helps to create these stem cells and a specific cell, the Sertoli cell, facilitates spermatogenesis. Spermatogonia divide by mitosis and then meiosis to form spermatocytes.The next form is called spermatids, which eventually develop into spermatozoa (singular: spermata-zoon). (Each primary spermatocyte forms four functional gametes.) The testes produce millions of spermatozoa each day. It takes about 2 months for sperm cells to mature until they are stored in the ductus deferens.
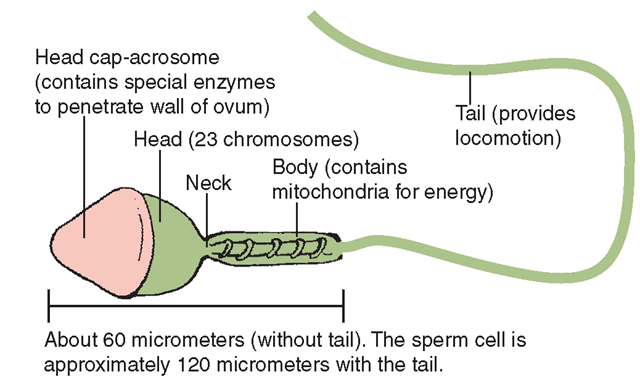
Sperm cells are highly specialized and are made up of several divisions (Fig. 28-4). The head contains 23 chromosomes (half of the human genetic material). The tip of the head, the acrosome, contains enzymes that can dissolve the tough cell wall of the ovum (the female sex cell). The body (middle piece) contains mitochondria, which provide the energy necessary for locomotion. The whip-like tail is a flagellum that propels the sperm with a lashing motion.After sperm and semen combine in the ejaculatory duct,semen (now also known as ejaculatory fluid) contains about 60–100 million sperm cells per milliliter. Semen with a sperm count of less than 10–20 million per milliliter may have difficulty fertilizing an ovum. The amount of semen each man ejaculates (expels from the body) varies from 2–5 mL. After ejaculation into a woman’s vagina, a sperm cell can survive up to 3 days. Of the average 250 million sperm cells ejaculated, only about 100 survive to contact the ovum in the oviduct.
Key Concept Sperm have 23 chromosomes. Sperm can live for a maximum of 3 days after ejaculation. Under normal conditions, only one sperm fertilizes the ovum.
FIGURE 28-4 ● A human sperm cell.
COPULATION
Sexual intercourse or sexual union between a man and a woman is called copulation, intercourse, or coitus. The man inserts his erect penis into the vaginal canal and deposits semen containing sperm when he ejaculates. Other substances in semen include citric acid, fructose, enzymes, coagulation proteins, lipids (fats), prostaglandins, and other secretions from the seminal vesicles and prostate. During sexual arousal, the bulbourethral glands secrete a clear liquid, pre-ejaculate, which helps to lubricate the urethra so sperm can pass; it also cleans out any urine or foreign matter. The male sex act is a complex series of reflexes consisting of several components: erection, secretion, emission, and ejaculation. Erection occurs when nervous impulses from the spinal cord and brain cause vasodilation of the arteries of the penis. When the arteries dilate, venous return is obstructed and the cavernous tissue in the penis becomes engorged with blood. This blood can only leave via a system of veins around the outside of the corpus cavernosum. The expanding tissue constricts these veins and contains the blood until orgasm is achieved. (Inability to achieve erection is called impotence.) Emission is the accumulation of sperm cells and secretions in the urethra. Ejaculation is the forceful expulsion of semen from the ejaculatory ducts, through the urethra. Orgasm is the physical, emotional, and pleasurable sensation that occurs at the climax of sexual intercourse; in men it is accompanied by the ejaculation of semen.
Difficulty in achieving orgasm is called anorgasmia. Low sperm count is called oligospermia. Disorders of the male reproductive system are discussed.Sexually transmitted infections and infertility are described.
EFFECTS OF AGING ON THE SYSTEM
As men age, they may experience changes (sometimes called andropause or male climacteric), but at a much slower rate than women (Table 28-1). No sharp demarcation of the beginning or end of sexual activity or reproductive ability is found in the male reproductive system. Men never stop producing sperm, but their rate of sperm production decreases because their level of testosterone secretion declines with age. Men also may gain weight and become more susceptible to atherosclerosis and osteoporosis. Many men experience benign or malignant hypertrophy or hyperplasia (enlarging) of the prostate gland. Prostatic hyperplasia may cause difficulty in urination, retention of urine, and incontinence, or it may interfere with the ability to have an erection. Older men experience a longer refractory period between orgasm and the ability to achieve another erection. The bulbourethral glands get smaller and reduce secretions; external lubrication may make intercourse more comfortable.
TABLE 28-1. Effects of Aging on the Male Reproductive System
|
FACTOR |
RESULT |
NURSING IMPLICATIONS |
|
Testosterone levels decrease. |
Degeneration of testicles; reduction in size Decrease in sperm production Difficulty in achieving and maintaining an erection Frequency of erection decreases |
Educate client that these changes are normal. Refer client to counseling, if needed. |
|
Enlargement of prostate gland |
May be benign or malignant (prostate cancer); may have difficulty voiding |
Encourage testicular self-examination. Encourage medical examination and PSA test to catch early prostate cancer. |
|
Fibrosis, sclerosis, and vascular changes occur in penis. |
Decrease in frequency of erection |
Encourage medical examination. Refer client to counseling, if needed. Medications may be helpful; surgical procedures are available. |
KEY POINTS
• Internal organs of the male reproductive system include the testes (containing the seminiferous tubules), ducts, and glands (seminal vesicles, prostate, bulbourethral).
• External structures of the male reproductive system are the scrotum (a sac that supports and protects the testes) and the penis, which serves as a common passageway for the urinary and reproductive systems.
• The ducts of the male reproductive system include the epididymis, ductus deferens, and ejaculatory duct. Sperm mature in the epididymis, travel through the ductus deferens, and join other secretions in the ejaculatory duct before exiting the body.
• The male reproductive system is under the influence of hormones from the hypothalamus, pituitary, and gonads.
• Male hormones are called androgens. Testosterone is the major male androgen.
• In men, gonadotropic hormones stimulate the formation of sperm and the secretion of hormones from the sex glands.
• Ejaculatory fluid contains semen from the seminal vesicles, sperm from the vas deferens, alkaline secretions from the prostate, nutrients, and mucus from the bulbourethral glands.
• Sperm cells are called spermatozoa and are stored in the ductus deferens.
• During copulation, the penis becomes firm in order to penetrate the vagina. The urethra within the penis serves as a passageway for sperm and semen during ejaculation. (No urine is able to pass during sexual intercourse.)