Learning Objectives
1. Identify the three major classifications of hormones that influence the male reproductive system and the functions of each classification.
2. Describe the structures of the male reproductive system and their functions.
3. Discuss the specific roles of the epididymis, ductus deferens, and ejaculatory duct in the male.
4. Describe how sperm migrate through the reproductive system.
5. Describe the components of ejaculatory fluid and their sources.
6. Explain the process of the male sex act.
7. State three effects of aging on the male reproductive system.
|
IMPORTANT TERMINOLOGY |
||
|
androgen |
foreskin (prepuce) |
puberty (male) |
|
bulbourethral (Cowper’s) |
gamete |
scrotum |
|
gland |
glans penis |
semen |
|
circumcision |
gonad |
seminal vesicle |
|
climacteric |
interstitial cells |
seminiferous |
|
copulation |
nocturnal emission |
tubule |
|
ductus deferens |
orgasm |
spermatozoa |
|
ejaculation |
penis |
testes |
|
epididymis |
perineum |
testosterone |
|
erection |
prostate |
|
The previous systems studied in this unit have focused on sustaining the individual. The reproductive systems work distinctly to continue the species and to pass genetic information from parents to child. Unlike other body systems that are generally similar for both sexes, the reproductive systems in adult males and females are different. This topic examines the male reproductive system.
Sexual reproduction involves the combined effort of both internal and external structures. Keep in mind that sexual reproduction is a dependent process that involves the reproductive systems of both the man and the woman.
Structure and Function
The organs of the male reproductive system function to produce and transport sperm (Box 28-1). A man’s reproductive capacity is directly associated with sexual excitement,penile erection, and ejaculation. A woman’s ability to reproduce does not depend on sexual excitement, and conception can occur through mechanical means (e.g., artificial insemination). Sexual pleasure, however, is equally important for both men and women.
The male reproductive system consists of the testes (produce sperm), ductal system and seminal vesicles (store and transport sperm), scrotum (holds testes and regulates their temperature), penis (required for sperm deposit in female), and accessory glands (produce male hormones and other secretions). The area between the scrotum and anus is the perineum. Figure 28-1 illustrates male reproductive structures.
TESTES
The paired testes (singular: testis) are also known as testicles, reproductory organs or sex organs (Fig. 28-2). They produce spermatozoa (sperm cells), through a process called spermatogenesis, briefly described later. The testes also secrete sex hormones. (The combining forms for testis in medical terms are orcho/o-, orchi/o-, and orchid/o-.)
BOX 28-1.
Functions of the Male Reproductive System
Development of Sexual Characteristics
♦ Secretes hormones that initiate puberty
♦ Maintains specific male characteristics
♦ Secretes mucus, spermatic fluid, and other substances
Reproduction
♦ Produces sperm
♦ Passes genetic information to offspring
♦ Participates in copulation and fertilization
Special Considerations :LIFESPAN
Nocturnal Emissions
Pubescent boys may experience penile erection and spontaneous ejaculation of semen during sleep. These nocturnal emissions are normal and are thought to be caused by hormonal changes.
In the adult man, the testes are two almond-shaped glands, one on each side of the scrotum (described later in this topic). The testes are small, approximately 1.5-2 inches (3.7-5 cm) long and 1 inch (2.5 cm) wide and thick. Usually one testis hangs lower than the other, probably to keep them from hitting each other. The testis is suspended from the ductus deferens, which is the beginning portion of the spermatic cord. Tissue layers, one of which partitions the testis into 250-300 wedge-shaped lobules, cover each testis.
Each lobule contains the functional units of the testis, which are called the seminiferous tubules. Most of the seminiferous tubule is tightly convoluted, although one portion is straight (see Fig. 28-2.) The combined length of a man’s seminiferous tubules is about half a mile! Within these tubules, the sperm cells are produced and mature almost completely. Between the tubules are small clusters of specialized endocrine cells, called interstitial cells, which secrete testosterone and other androgens (male hormones). The cells lining the tubules produce sperm also.
THE DUCTAL SYSTEM
The male reproductive organs have a system of ducts that store and transport sperm from the testicles to the urethra. These ducts include the paired epididymides (singular: epididymis), the ductus deferentia (singular: ductus deferens), and the ejaculatory ducts.
Epididymis
The epididymis is a long, comma-shaped organ attached to the posterior surface of the testis. This tightly coiled tube is approximately 20 feet (6 m) long, but is so tiny that it can barely be seen with the naked eye. It stores sperm cells. Also, within the epididymis, millions of sperm cells are in their final stages of maturation. Here, they develop a tail and gain motility (ability to move). (Sperm cells are unable to fertilize an egg unless they mature in the epididymis.) Smooth muscles propel sperm into the ductus deferens.
Ductus Deferens
The sperm continue their journey through a tube called the vas deferens or ductus deferens (Latin: “carrying-away vessel”; plural: ductus deferentia), which is about 11.5-18 inches (30-45 cm) long.
FIGURE 28-1 · Organs of the male reproductive system, showing one testis. The arrows indicate the course of sperm cells through the system.
FIGURE 28-2 · The testis is the site of sperm production in the male. The rete testis (network of channels formed by the seminiferous tubules) contains concentrated sperm and fluid. It helps the epididymis to absorb this fluid; otherwise, the man would be infertile.
These paired tubes transport sperm from the epididymis to the ejaculatory duct. Each ductus deferens passes upward posterior to the testis, then into the abdominal cavity, and continues over the top and down the posterior surface of the urinary bladder, into the pelvic cavity. Peristaltic contractions propel sperm cells through the ductus. Each ductus deferens joins a duct from the seminal vesicles. These ducts, together with blood vessels, lymphatic vessels, nerves, and connective tissue coverings, make up the spermatic cord. The spermatic cord is covered with connective tissue. The spermatic cord passes through an opening in the muscular abdominal wall called the inguinal canal. Normally, the inguinal canal firmly encloses the spermatic cord as it passes through the abdominal wall. It is a weak spot, however, and a common site for herniation in men (inguinal hernia). It is also the site where the testicles descend into the scrotum before birth.
Key Concept The two vas deferens or ductus deferentia are ligated (tied) and cut in the male sterilization procedure, called vasectomy This operation does not affect erection or ejaculation; it just prevents sperm from passing.
Ejaculatory Ducts
The ejaculatory ducts are about 1 inch (2 cm) long. Each one originates where the ampulla of the ductus deferens joins the duct from the seminal vesicle (see Fig. 28-1). The ejaculatory ducts empty into the urethra. The ejaculatory ducts also receive secretions from the prostate gland, to make up semen. (The semen, mixed with various secretions, is called ejaculatory fluid.)
SCROTUM
The two testes are enclosed in a sac-like structure called the scrotum, which is suspended behind the base of the penis. The scrotum supports and protects the testes. The external appearance of the scrotum varies, depending on environmental conditions and the contraction of its muscles. The scrotum regulates the temperature of the testes. The cremasteric muscles involuntarily contract and tighten the spermatic cord to bring the testicles closer to the body as external temperature lowers (the cremasteric reflex). The temperature of the testes (35°C or 95°F) is lower than internal body temperature (which is normally 37°C or 98.6°F). This temperature is maintained to facilitate sperm production.
Nursing Alert Exposure to increased temperature over a period of time can impair spermatogenesis (sperm production) in the testes. It is also thought that wearing tight-fitting undergarments might contribute to infertility and decreased numbers of sperm, because of the close contact of the scrotum with the rest of the body
Key Concept in addition to reacting to temperature changes, the cremasteric reflex also pulls the testicles closer to the body during severe danger or a fight, in order to protect them.This reflex also occurs during sexual intercourse.
Special Considerations :LIFESPAN
Undescended Testes
Undescended testes (cryptorchidism) can occur in infants. This is a situation in which the testes do not move down into the scrotal sac. It occurs more often in premature infants, but also occurs in as many as 4% of term infants. Undescended testes can increase the temperature in the testes, which could result in decreased sperm produc-tion.Therefore, documentation of the presence of undescended or descended testes is important for all male infants. Corrective surgery may be required.
PENIS
The penis is a cylindrical organ located between the upper thighs immediately in front of the scrotum. It is composed of three masses of cavernous (erectile) tissue, each of which contains smooth muscle, connective tissue, and blood sinuses (large vascular channels). The corpus cavernosum is on either side, with the corpus spongiosum in the center. When blood flow through these sinuses is minimal, the penis is soft and flaccid. At the time of sexual excitement, blood fills the sinuses and the penis becomes firm and raises up, an erection. The erect penis is capable of penetrating the vagina to deposit sperm. During sexual intercourse, the semen is propelled into the vagina.
Key Concept Route of sperm: testes [seminiferous tubules] (produce sperm and male hormones, begin maturation of sperm cells) S epididymis (storage of sperm, final maturation of sperm, sperm become motile) S ductus deferens (up past testis, into abdomen; up front, over top, and down back of urinary bladder) S joins seminal vesicle S ejaculatory duct S through prostate S through inguinal canal S urethra S expelled to outside.
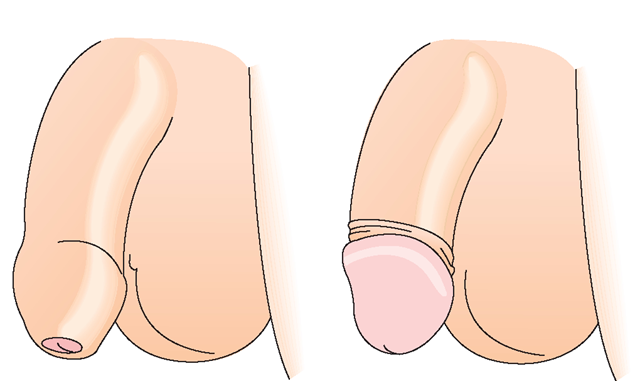
The smooth cap of the penis surrounding the corpus spongiosum is sensitive and is called the glans penis or head of the penis. It is covered by a fold of loose skin that forms the hood-like foreskin (prepuce)—Fig. 28-3. The foreskin provides protection for the penis and helps keep the glans moist. The outside of the foreskin looks like other external skin, whereas the inside is a membrane like the inside of the eyelid. The foreskin is attached to the penis by a sensitive, stretchy band, the frenulum (frenulum preputii penis), which extends under the glans penis and connects to the mucosa of the shaft of the penis. The frenulum helps contract the prepuce over the glans and prevents the prepuce from being retracted too far. Surgical removal of the foreskin, called circumcision, is sometimes performed on male babies.
FIGURE 28-3 · The foreskin or prepuce of an uncircumcised male covers and protects the glans penis. The frenulum underneath helps contract the foreskin around the glans.The foreskin can be manually retracted to expose the glans.
The urethra within the penis serves as a common passageway for both the urinary and reproductive systems. The opening is at the distal tip of the penis. (Urine and ejacula-tory fluid do not pass through the urethra simultaneously.) An involuntary sphincter located at the base of the bladder and the prostate gland automatically inhibits micturition (voiding) during semen ejaculation.
NCLEX Alert The close proximity of the urinary and reproductive systems may be relevant for your consideration in client teaching, preparing a client for a procedure, or for the client’s self-care after the procedure.