System Physiology
Although the integumentary system’s functions are many, protection is one of the very most important.
PROTECTION
The skin and its accessory structures guard the body from pathogens and other foreign substances, preventing invasion into the internal environment. The skin further protects the body by retarding the loss of body fluid, assisting in heat regulation, and by excreting waste products. The Langerhans’ cells are part of the adaptive immune system.
THERMOREGULATION
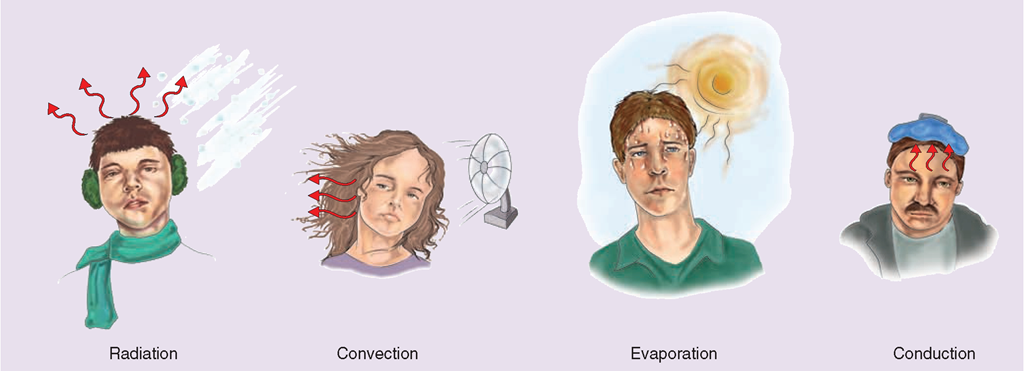
The integumentary system, in combination with the lungs, is also responsible for regulating and balancing the body’s internal temperature through a process called thermoregulation. The body’s temperature must remain fairly constant (around 98.6°F, 37 °C) for all other systems to function properly. Body temperature is an indicator of physiologic changes occurring in a person’s body. One important nursing technique is the measurement of accurate body temperature. The body loses heat through four processes: radiation, convection, evaporation, and conduction (Table 16-2). The skin conserves heat through shivering and “goose flesh” and gives off heat via the sweat glands.
Special Considerations: LIFESPAN
Preventing Heat Loss in Infants and Newborns
Very young infants do not have the ability to shiver in order to produce heat. They are also susceptible to heat loss via all four mechanisms of heat transfer, particularly evaporation, because of their large body surface area in proportion to size. This is most true immediately after birth.
To prevent excessive heat loss in the newborn, keep the infant away from drafts and place him or her in a temperature-regulated environment. Keep the infant dry and add clothing, especially a hat.
TABLE 16-2. Mechanisms of Heat Transfer
Mechanisms of Heat Loss
If the body becomes too warm, a message is sent from the hypothalamus in the brain. The dermal capillaries dilate (widen), and more blood flows to the skin surface. Because more blood is brought to the surface, body heat is lost to the surrounding air by radiation, convection, evaporation, or conduction.
Radiation. People and animals give off infrared heat rays through radiation. A large percentage of a person’s body heat is lost through the head because it functions in a manner similar to that of a chimney.
Convection. In convection, heat is transferred and given off from a surface (the skin) to the surrounding gases (the air). For example, an air current (e.g., a fan) can move warm air away from the skin’s surface.
Evaporation. Evaporation is the returning of water to the air through vapor. Water on the body’s surface can be perspiration (sweat) or water from an outside source, such as a shower. Water evaporation causes a cooling effect. The body normally loses about 500 milliliters of water per day due to insensible (unnoticed) evaporation. Too much water loss can lead to dehydration.
Key Concept In a burn, the skin’s control of evaporation is lost, causing excessive fluid loss.
Conduction. Conduction is the transfer of heat from one object to another by direct contact. It is the least important mechanism in the transfer of heat away from the body; however, within the body, a large amount of internal heat is transmitted by conduction to the skin via the blood vessels. When the body comes in contact with a cooler object, the body transfers heat away from itself. For example, a cool cloth on the forehead or a tepid bath can help a person feel cooler on a hot day. Table 16-2 summarizes the mechanisms of heat transfer discussed here.
Mechanisms of Heat Production and Conservation
Blood vessel constriction, shivering, and “goose flesh” are thermoregulation processes that help to warm the body. When the body becomes too cool, dermal capillaries constrict (narrow), reducing the amount of heat lost through the skin. This constriction of superficial capillaries also causes the skin color to change from its normal color to a more pale color. The reflex action of shivering helps produce added heat and goose flesh raises the hairs in the skin to provide insulation (see Fig. 16-1). The more subcutaneous fat a person has, the better the body’s ability to insulate itself.
Nursing Alert Vasoconstriction in the extremities can cause pallor (whiteness) and coolness of the skin. Cyanosis (red-blue coloring) is a condition caused by hypoxia (lack of oxygen in the tissues) or hypothermia (severe decrease in body temperature).
VITAMIN D PRODUCTION
The skin plays a role in the body’s production of vitamin D, which is important for the growth and repair of bones. It facilitates the absorption of calcium and phosphorus from the small intestine. Vitamin D is produced in the skin when stimulated by sunlight (UV light); then, via enzymes in the body, it is changed into a substance known as cal-citrol or calciferol. Calciferol plays a role in absorbing calcium from the body’s gastrointestinal tract.Vitamin D also assists in the retention of certain other vitamins.
Special Considerations: LIFESPAN
Vitamin D Deficiency
Lactase, the enzyme needed to break down the milk sugar lactose, decreases with advancing age, resulting in milk intolerance (lactose intolerance) for some older adults. Decreased intake of irradiated milk accompanied by limited sun exposure (secondary to confined bed rest or nursing home living) doubles the risk of vitamin D deficiency in older adults. (Incarcerated persons may also experience this deficiency.) Bone loss (due to the inability to metabolize calcium) is one consequence of vitamin D deficiency.
COMMUNICATION AND SENSORY AWARENESS
The skin receives stimuli from the outside world, providing a dynamic interaction between external and internal environments (sensory awareness). This is part of the skin’s role in protection. Nerve endings in the dermis register pain and pleasure. The nerve receptors in the skin also sense hot and cold, vibration, and pressure, and provide these stimuli to the brain. Some areas are more sensitive than others, such as the fingertips. The body may react with a reflex response, for example by withdrawing the hand from a hot stove or a frozen piece of metal.
The skin can also detect comfortable sensations. It registers the loving touch of a friend. The skin and blood vessels are involved in foreplay, lovemaking, and sexual response. Much of the communication between a newborn and its parents comes through the sense of touch. Nurses also use touch in therapeutic ways in the care of clients. Communication also occurs through facial movements and changes in skin color. For example, blushing usually changes the skin color to a redder or darker hue. A smile is understood by all people.
Disorders of the skin and other structures of the integumentary system are discussed.
Key Concept The average square inch of skin contains about 1,000 sweat glands, 20 blood vessels, 60,000 melanocytes, and more than 1,000 nerve endings.
NCLEX Alert You should be aware of the primary functions of the integumentary system as they commonly relate to nursing care or actions, client safety and infection control. The NCLEX may include scenarios related to the hazards of immobility, illness, or injury of one or more anatomical systems.
EFFECTS OF AGING ON THE INTEGUMENTARY SYSTEM
Table 16-3 summarizes the major effects of aging on the system. Normal changes are influenced by heredity, dietary habits, sun exposure, smoking, hydration level, and general health.
With age, skin tends to become dry and often appears scaly. It takes on a transparent or translucent appearance and, with the loss of subcutaneous (under the skin) fat, the skin may sag and become wrinkled. Skin turgor (tone) is reduced; a pinched area does not return immediately into position. The glands in the skin decrease their secretions; therefore, the older person has less perspiration and less oily skin. Hair becomes coarser and increases in areas such as the nose, ears, and eyebrows. Male pattern baldness is common. Women may develop hirsutism (facial hair).
The skin of the older person is more fragile (friable) and more subject to breakdown than the skin of the young person. The skin loses its elasticity, partly because of impaired circulation. In general, aged skin becomes thinner, epidermal turnover decreases, and the number of protective cells diminishes. As a result, many older adults heal poorly and are at increased risk for pressure ulcers, fungal or viral skin infections, and skin cancer. The loss of subcutaneous fat removes some of the skin’s insulating function; heat is lost more rapidly. For this reason, older people often have difficulty keeping warm.
NCLEX Alert Be alert to normal differences in the integumentary system. Changes throughout the lifespan will relate to the actions you take regarding safe and effective care.
MAINTENANCE OF HEALTHY SKIN
The various functions of the skin (and related structures) make it a very important organ of the body. The skin requires nutrients and hydration to keep it functioning well. Sun exposure can be dangerous; excess exposure can cause burns, premature aging of the skin, or skin cancer. Recommendations for limiting exposure are given in the display below. Sunscreen with an SPF (sun protection factor) of at least 15 is helpful (Educating the Client 16-1).
Key Concept Skin is the first line of defense against infection.Therefore, maintenance of skin integrity is a high priority Skin disorders include abrasions, blisters, rashes, infection, cancer fungal infections (e.g., athlete’s foot), and sunburn.
TABLE 16-3. Effects of Aging on the Integumentary System
|
FACTORS |
EXAMPLES OF RESULTS |
NURSING IMPLICATIONS |
|
Melanin is either lost or migrates and clusters in the epidermal layer |
"Age spots” or "liver spots” result. White areas (vitiligo) may appear |
Reinforce self-esteem. Discuss available makeup. |
|
Epidermal and dermal layers flatten. |
Skin tends to tear ("fragile” or friable skin). |
Assess for skin tears. Use caution in handling the older person. |
|
Capillary bed in dermis becomes more friable (fragile)—blood can ooze into dermis. |
Dark red patches in the skin (purpura) are commonly seen on arms of older adults. Person may bruise easily. |
Be careful when handling the arms of clients with purpura. Protect from bruising. |
|
Capillaries leak small amounts of blood into tissues. |
Petechiae occur (small red dots on skin). |
Explain to the person that makeup may be used. |
|
Individual may have loss of sensation and loss of abilities. |
Person is unable to detect or treat cause of ulcerated areas; pressure ulcers may develop more quickly. May be more susceptible to falls. |
Inspect skin frequently, especially bony prominences, arms, and feet. Protect from falling. Teach protective measures. |
|
There is loss of elasticity in dermis, loss of subcutaneous layer of fat, and loss of collagen fibers. |
Wrinkles. Decreased strength of skin layer |
Discourage smoking and exposure to the sun. Reinforce self-esteem. |
|
Turgor is lost. |
Wrinkles. "Tenting” on some areas can give false-positive (for dehydration) results. |
Avoid using areas of skin that normally develop wrinkles for assessing turgor (Do not use back of hand; OK to use arm or leg.) |
|
Some insulating function is lost with loss of subcutaneous fat. |
Heat is lost more rapidly. The older person may be chilly |
Provide extra blankets or sweater Avoid chilling during treatments. |
|
Dermal layer thins. |
Skin becomes transparent. |
Explain to client. |
|
Changes occur in hair distribution, influenced by heredity and other factors. General loss of body hair occurs. |
Axillary, pubic, and scalp hair thins. Men may develop thicker hair in nose, ears, and eyebrows; hair on head becomes thinner |
Be careful when giving hair care. Excess hair in nose or ears may be clipped carefully |
|
Female hormones are lost. |
Women may develop facial hair (hirsutism). |
Assist in removal of facial hair: Prevent injury. |
|
Nails grow more slowly and become thicker |
Nails, especially toenails, become thick and brittle. |
Refer to podiatrist as needed. Foot soaks may be needed. |
|
The glands in the skin decrease their secretions. |
Less perspiration and less oily skin than before cause skin to become very dry (may appear scaly). |
Advise that daily shower or bath may not be needed (bath may dry skin more). Be sure skin is clean because skin is more fragile and more subject to breakdown. Use lotion as needed. |
|
Thermoregulation abilities are lost. |
More susceptible to heatstroke or chilling. |
Teach individual to avoid overheating. Observe in hot weather; encourage intake of adequate fluids. |
|
Circulation is reduced. |
Wound healing takes longer—old or damaged cells are not readily replaced. |
Provide careful wound care. Prevent further injury. Refer to physician as needed. |
Special Considerations: LIFESTYLE
♦ It is important to protect your skin.
♦ Keep skin clean, to prevent growth of pathogens.
♦ Clean and cover cuts and open wounds.
♦ Use cosmetics sparingly; remove daily.
♦ Dress appropriately for the weather
♦ Eat a balanced diet; drink plenty of water and other fluids.
♦ Skin cancer has been related to excessive UV exposure. Protect your skin from excessive sun; use sunscreen, wear long-sleeved clothing and a hat, stay in the shade. Be extremely careful if using a tanning bed.
Nursing Alert The use of sunscreens is not advisable for infants under 6 months of age.
IN PRACTICE :EDUCATING THE CLIENT 16-1
SUNSCREENS
Sunscreens are used to protect the skin from the sun’s UV rays. They can assist in prevention of skin cancers caused by sun exposure. The SPF (sun protection factor) determines the amount of UV rays that reaches the skin. Most often, SPF 15 or 30 is used. Apply sunscreen thoroughly and evenly; cover completely Reapply after sweating or swimming. Remember even if the SPF factor is high, the amount of exposure time to the sun should be limited to prevent sunburn. Read and follow the directions.
Consider allergies to the sunscreen ingredients and adverse reactions with certain medications. Sunscreens may cause problems for people with skin conditions, such as skin cancer psoriasis, or lupus; for people taking certain medications; or for people undergoing radiation or chemotherapy
It is important not to block all UV rays; cases of vitamin D deficiency have been reported in people who have no exposure to the sun at all.
KEY POINTS
• The skin and its accessory structures (hair, nails, and glands) make up the integumentary system.
• The primary functions of the integumentary system are protection, thermoregulation, metabolism, sensation, and communication.
• The skin, the largest organ in the body, is vital for survival. The principal layers of the skin are the superficial epidermis and the deep dermis.
• The subcutaneous tissue (hypodermis) lies below the dermis and binds the skin to underlying muscle tissue. It is made up mostly of fat cells that insulate and protect underlying tissue.
• The epidermis is the outermost protective skin layer. It contains keratin, which protects the body from excessive water loss or gain, and melanin, which protects the body from ultraviolet rays and influences skin tone.
• The dermis underlies the epidermis and contains nerves, hair follicles, blood and lymph vessels, and glands. It is composed of tough connective tissue containing collagen, which contributes to the skin’s elasticity.
• Skin color is due to the presence or absence of melanin, carotene, and hemoglobin.
• Glands are unicellular or multicellular structures of epithelial tissue that produce secretions. The functions of glands in the integumentary system are protection and thermoregulation.
• The skin regulates and balances the body’s temperature via radiation, convection, evaporation, conduction, shivering, dilation or contraction of blood vessels, and “goose flesh.”
• Infants and the elderly have a higher risk of heat loss than do other age groups, for many reasons.
• Through sensory awareness, the skin provides a dynamic interaction between the external and internal environments.
• The effects of aging include wrinkling, loss of subcutaneous fat, atrophy of glands, and a decreased number of protective cells. Skin problems are often more common for older adults.
• To protect the skin, one should eat a healthy diet and drink an adequate amount of daily fluids. Additional protection is required when in the sun.