Learning Objectives
1. Describe the structures and main functions of the skin.
2. Explain the functions of keratin and melanin.
3. Identify the structures and functions of a fingernail or toenail.
4. Compare and contrast the functions of the sudoriferous glands and the sebaceous glands.
5. Define radiation, convection, evaporation, and conduction and give an example of each.
6. Explain the purpose of “goose bumps” or “goose flesh.”
7. Discuss the skin’s role in sensory awareness.
8. Name five changes that occur in aging skin.
9. Describe four ways to protect skin from damage.
|
IMPORTANT TERMINOLOGY |
||
|
alopecia |
epidermis |
pores |
|
carotene |
evaporation |
radiation |
|
cerumen |
freckles |
sebaceous glands |
|
ceruminal glands |
friable |
sebum |
|
collagen |
hair follicle |
skin turgor |
|
conduction |
hemoglobin |
squamous |
|
convection |
hypodermis |
subcutaneous tissue |
|
corium |
integument |
sudoriferous glands |
|
dermis |
keratin |
thermoregulation |
|
desquamation |
melanin |
transdermal |
|
diaphoresis |
nevus |
vitiligo |
|
Acronyms |
|
Hb or Hgb |
|
SPF |
|
UV |
The skin and its accessory structures form the body’s integumentary system. Integument means covering. Because skin covers the entire outside of the body, it is the body’s largest organ. The skin of an average adult covers 1.5 to 2.0 square meters (16.1-21.5 sq. ft.) and is about 2 to 3 mm (0.1 inch) thick. The skin is called an organ because it is composed of a variety of tissues, each of which has a specific purpose.
The skin contains several types of epithelial tissue that are partially responsible for the skin’s protective and absorptive functions. Glands provide secretions from the body’s internal environment to the external world. Connective tissues attach skin to underlying muscle. Nervous tissue is integrated throughout the skin to help the body react to the world around it (sensations of heat, cold, pain, touch, vibration, and pressure). In addition, the integumentary system depends on other tissues, organs, and systems. The skin and its accessory structures create a dynamic surface for communication between internal and external forces.
Key Concept The integumentary system is composed of the skin and its accessory structures: hair; nails, and glands. Integument means covering.
Structure and Function
Primary functions of the integumentary system are protection, thermoregulation (temperature regulation), metabolism, sensation, communication, and storage (Box 16-1). The skin produces substances that aid in protection and metabolism. Secreted oil acts as a waterproofing material, while protecting the skin from drying and cracking. Perspiration helps rid the body of waste products. The skin has some absorptive powers, which is the basis for applying medications trans-dermally (through the skin). Certain skin cells are also important components of the immune system, which helps fight off foreign invaders.
BOX 16-1.
Functions of the Integumentary System
Protection
♦ Provides a physical barrier against microorganisms and foreign materials
♦ Helps prevent absorption of harmful substances from outside the body
♦ Defends against many chemicals
♦ Protects against water loss or gain
♦ Protects underlying structures, such as fragile organs
♦ Protects against excessive sun exposure (ultraviolet rays)
♦ Cushions internal organs against trauma
♦ Produces secretions for protection and water regulation
♦ Absorbs helpful medicines
♦ Prevents nutrients from being washed out of the body Thermoregulation
♦ Controls body temperature by convection, evaporation, conduction, and radiation
♦ Helps body adjust to external changes in temperature
♦ Helps dissipate heat during exercise
♦ Produces shivering and “goose flesh” to keep body warm in cool temperatures
♦ Cools the body through evaporation
Metabolism
♦ Provides insulation (skin hairs, subcutaneous fat)
♦ Helps produce and use vitamin D
♦ Helps the body eliminate certain waste products
♦ Absorbs medication
♦ Contributes to changes in cardiac output and blood pressure
♦ Absorbs gases; some oxygen, nitrogen
Sensation
♦ Perceives stimuli: heat, cold, pain, pressure, touch, vibration, injury
♦ Provides social and sexual communication
♦ Allows for physical intimacy
Communication
♦ Communicates feelings and moods through facial expressions
♦ Portrays feelings of anger; embarrassment, or fear (e.g., flushing, sweating, pallor)
♦ Communicates cultural and sexual differences through skin and hair color
♦ Portrays body image via skin’s general appearance
Storage
♦ Stores water
♦ Stores fat
♦ Stores vitamin D
SKIN
The skin is divided into layers. The epidermis makes up the skin’s thin, superficial outer layer. Below the epidermis lies a thicker layer, the dermis, which contains important structures of hair, glands, blood vessels, and nerves. The hypo-dermis (subcutaneous tissue, fatty layer) is not actually part of the skin, but is discussed here because it cushions, supports, nourishes, and insulates the skin and it anchors skin to underlying tissues and organs. It is a single layer of fat tissue below the dermis (Fig. 16-1). (A skin specialist is called a dermatologist.) The term, cutaneous, means “of the skin.”
The Epidermis
The epidermis is the outermost protective layer of the skin (“epi-” means over or upon). It is composed of squamous (scaly) epithelium, stratified into several layers (see Table 15-4 and 16-1). These layers (from bottom up) include the basale (germinativum), spinosum, granulosum, and corneum (horny layer), with the lucidum mostly in the palms and soles.
The innermost layer of the epidermis, which is composed of living cells, is called the basal layer, stratum basale, or stratum germinativum, indicating its role in germinating new cells. Here in the deepest level of the epidermis, mitosis (division and replication of cells) occurs. Most of the cells in the epidermis are keratinocytes (Table 16-1). These cells divide in the basal layer (basale) and push older cells toward the body’s surface. Thus, the living inner cells of the epidermis continually replace the outer cells. It takes between 2 and 4 weeks for the inner cells to totally replace the outer layer. (Other cells in the epidermis are Merkel cells [Merkel discs], which are involved in the sense of touch, as well as melanocytes and Langerhans’ cells, both of which are discussed below.)
The outer layer of the epidermis, the stratum corneum or horny layer, is relatively waterproof and provides a barrier against light, heat, bacteria, and other foreign substances. This layer is much thicker in some parts of the body, such as the soles of the feet, and thinnest in the eyelids. It contains all the dead cells from layers below. These cells are rubbed off constantly through washing and friction. This process is called desquamation.
Key Concept Every minute the human body loses 30,000 to 40,000 cells (about 9 pounds per year)!
All that is left of the cells after desquamation is a protein called keratin, which is the body’s true protector. It creates a waterproof barrier. Most microorganisms cannot penetrate unbroken skin because of keratin.
TABLE 16-1. Principal Cells of the Epidermis
|
TYPE |
FUNCTION |
|
Keratinocyte |
Produces keratin, which waterproofs and protects skin |
|
Melanocyte |
Produces the pigment melanin |
|
Langerhans’ (also called nonpigmented granular dendrocyte) |
Provides immune response |
|
Participates in allergy response |
|
|
Merkel |
Promotes sensation of touch |
FIGURE 16-1 · Cross section of skin structures.
Key Concept Damage through the base layer of the epidermis to the dermis (such as in a second- or third-degree burn) takes longer to heal because the damaged skin has lost its mitotic (reproductive) structures.
Melanocytes are cells within the epidermis that, through a complex process, create the pigment melanin. Melanin gives color to the hair, skin, and other structures in the body. Also within the epidermis are Langerhans’ cells, part of the skin’s immune system. They help detect foreign substances, in order to defend against infection. They are also involved in skin allergies.
The epidermis has no nerves or blood supply and does not receive nourishment directly from the circulatory system, but is nourished by diffusion from the underlying dermis. Normally, the epidermis and the dermis do not lie flat on one another. The dermis reaches up into the epidermis, causing ripples or ridges on the skin surface that are particularly visible on the tips of the fingers, which are known as fingerprints. These ridges provide some friction, helping to grasp objects.
Sometimes external friction causes a separation of the epidermis and dermis, leading to tissue fluid accumulation (blister). Areas of greater friction, such as the soles of the feet and the palms of the hands, cause the epidermis there to thicken and to develop calluses.
Special Considerations: LIFESPAN
Wrinkling of Skin
Wrinkles occur due to the loss of elastic fibers and collagen in the skin. The dermis also thins. The loss of oil (sebum) also contributes to wrinkling, with oilier skin wrinkling less. (Cigarette smoking has been linked to a more rapid destruction of elastic fibers, and can lead to the development of wrinkles at a younger age. Exposure to sun and genetics can also play a part in wrinkling.)
The Dermis
The dermis, also known as the corium, is the “true skin.” It is the thickest skin layer, composed entirely of live cells. The dermis nourishes, cushions, and protects the ever-changing epidermis. The dermis also functions to protect the delicate nerve endings and blood vessels within it. Like the epidermis, the dermis is also layered, with the upper or papillary layer containing blood and lymph vessels, nerve endings, apocrine glands, hair follicles, sweat (sudoriferous) glands, and oil (sebaceous) glands. It also contains elastic tissue, elastin, as well as collagen and fibrin. The reticular layer, deep within the dermis, is much thicker and is attached to the subcutaneous tissue.
Key Concept Mechanoreceptor nerve endings provide the senses of touch and heat.
Several types of connective tissue are found in the dermis. The major one is collagen (“colla” means glue), a tough, resistant, and flexible fibrous protein. In youth, collagen is loose and elastic. Collagen hardens and loses elasticity with age.
The Subcutaneous Tissue
The subcutaneous tissue (or hypodermis, fatty layer) is the layer beneath the dermis and on top of a layer of muscle. Its purpose is to attach the epidermal and dermal layers to underlying organs and help to cushion, protect, and hold these structures in place. It specializes in the formation and storage of lipocytes (fat cells). It also serves as a heat insulator. The amount of fat stored depends on the body region and an individual’s age, sex, and nutritional state.
Skin Color
A combination of three pigments produces normal coloration of the skin: melanin, carotene, and hemoglobin.
Melanin is a brown-black pigment produced by melano -cytes, found mostly in the stratum basale. People of all races have the same number of melanocytes. Individual differences in skin color depend on the amount of pigment the melanocytes produce. The amount of melanin produced is a reflection of genetics and exposure to ultraviolet (UV) light. Exposure to the sun causes production of extra melanin, which helps protect the body from damaging effects of UV light and causes the skin to darken (tan). The skin also contains DNA-repair enzymes that help reverse UV damage. If the genes for these enzymes are absent, or if the DNA is damaged, the person is more susceptible to skin cancer, the most dangerous form of which is malignant melanoma.
Albino individuals are born without the ability to produce melanin. A true albino person has totally white hair and skin. This person’s eyes look red because of the lack of pigment in the iris and because of the reflection of the blood vessels in the eyes.
Special Considerations: CULTURE & ETHNICITY
The skin of Black people has more variation from one part of the body to the other than does the skin of people of other racial groups. This is partially due to variations in skin thickness. In addition, darker skin can hinder penetration of UV rays and may lead to a deficiency of vitamins, including vitamin D.
Freckles are patches of melanin clustered together. “Liver spots” (age spots) are also clusters of melanin, forming flat, brown-to-black, freckle-like patches as a person ages. Vitiligo is a skin condition in which the melanocytes stop making melanin, causing distinct, localized areas of white. A mole (nevus) is a circumscribed area on the skin that may be raised. Moles may be dark or flesh-colored. Moles usually do not represent an abnormality, but any changes that occur to an existing mole should be brought to the attention of a healthcare professional.
Key Concept Damaged skin often forms a scar This area is often depigmented or discolored.
Carotene is a yellowish pigment found in parts of the epidermis and dermis. Carotene is the precursor to vitamin A, which helps to maintain epithelial tissues. Vitamin A is important in proper growth of skeletal and soft tissues and necessary for night vision. Carotene tends to be more abundant in the skin of Asian people.
Hemoglobin is a pigment found in red blood cells. Oxygen binds to the hemoglobin (Hb, Hgb) molecule and is carried by the red blood cells. Although hemoglobin is not a pigment in the skin, the bright-red color of oxygenated blood flowing throughout the dermis gives a pinkish tone to the skin, which is more noticeable in light-skinned people.
ACCESSORY STRUCTURES
The hair, nails, sebaceous (oil) glands, sudoriferous (sweat) glands, and ceruminal glands are the main accessory structures (appendages) of the skin.
Hair
Hair derives from the subcutaneous fatty layer and covers almost all the skin except for a few areas, such as the lips, palms, soles of the feet, and penis. Dense hair covers the scalp, axilla, and pubis in adults. Male hormones are responsible for the greater density of hair on men’s entire bodies and influence their ability to grow facial and chest hair.
Hair is composed of keratinized cells. The visible, but dead, portion of hair above the skin is the shaft. The part lying below the skin is the root. Each hair grows from a tiny sac or bulb within a hair follicle (see Fig. 16-1). The dermal skin layer provides nutrients for growing hair. Sebaceous glands provide a substance, sebum, which gives hair its shine and provides some waterproofing. (Topical hair care products do not affect hair growth, only the general appearance of visible hair.) Hair grows slowly (approximately 1 mm every 3 days). Each follicle contains a single hair root, which, as long as it is alive, will continue to grow a hair. Normally, there are about 100,000 hair follicles on the adult human head.
Baldness (alopecia) is related to disease, high fever, emotional stress, surgery, pregnancy, starvation, chemotherapy, radiation, or hereditary factors. The male hormone, testosterone, contributes to male pattern baldness in men. Healthy women rarely become totally bald, although they may experience thinning hair with age. (Hair loss in cancer chemotherapy is related to hormonal influences and interference with DNA synthesis.)
Key Concept The adult human has about 5 million hairs, about the same number as a gorilla. Human hair is finer and shorter, however All humans lose about 50 to 100 hairs daily Each hair is pushed out by the growth of a new hair
Hair color is due to the type and amount of melanin in a layer of hair. The greater the amount of melanin, the darker the hair. Red hair is due to a pigment with an iron base (tri-chosiderin). Curliness of hair is dependent on the shape of the hair follicle. Straight hair is round, growing out of a round follicle. Curly hair bends—its cross-section is oval and it grows out of an oval follicle.
Surrounding each hair follicle are small, smooth muscles called the arrector pili (singular: arrectores pilorum). Stimulated by cold or fear, these involuntary muscles contract, making the hairs stand erect. This phenomenon gives the skin the appearance of “goose flesh” or “goose bumps”—the pilomotor reflex. These erect hairs provide an “air cushion” for the skin—a protective, insulating body mechanism. (In animals, this makes the animal look larger and more threatening.)
Special Considerations: LIFESPAN
Melanin in Hair
As people age, they lose melanin, and their hair appears gray; with a total loss of melanin, hair appears white.
The primary function of hair is protection (Box 16-2). Scalp hair protects against sunlight and insulates against cold. Eyelashes and eyebrows have the distinctive purpose of keeping dust particles and perspiration out of the eyes. Nostril hair protects against inhaling objects, such as foreign particles or insects. Hair in the ear canal serves a similar purpose.
Clinically, hair can reveal several adverse conditions. A hair sample can reveal environmental exposure to heavy metals, some drugs, or poisons much more accurately than a blood specimen. Hair texture can also reveal an individual’s nutritional status. A sample containing hair follicles or roots yields DNA and therefore can be used for identification purposes.
Special Considerations : CULTURE & ETHNICITY
There are ethnic variations in the normal amount of body hair a person has, with people of Mediterranean descent, for example, having more body hair and people of Asian descent having less.
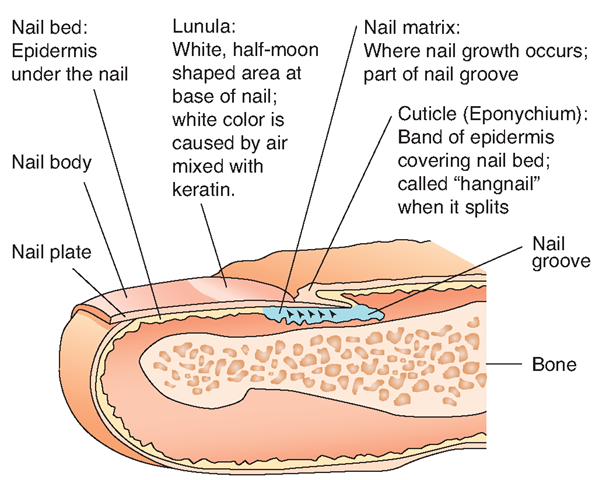
Nails
Nails protect the sensitive tips of fingers and toes. They help a person grab and pick up objects. Nails are tightly packed cells of the stratum corneum of the epidermis. The nail itself, as depicted in Figure 16-2, is made up of keratinized dead cells.
BOX 16-2. Functions of Hair
♦ Helps regulate body temperature
♦ Provides protection in various areas
♦ Enhances sensation
♦ Contributes to regrowing damaged epidermis through stem cells in a portion of the hair follicle
♦ Can reveal facts about the condition of the body
♦ Can be used for identification: the DNA in hair is unique to an individual
FIGURE 16-2 · Parts of a fingernail.
Nail growth occurs in the nail matrix. The new cells push the older cells away from the nail bed at a rate of approximately 1 millimeter per week. A fingernail lost through trauma takes about 3 to 5 months to regrow, and a toenail takes about 12 to 18 months to regrow. A nail will continue to regrow as long as the live cells in the nail bed remain undamaged.
Special Considerations : NUTRITION
Effects of Diet on Skin, Hair, and Nails
Healthy skin, hair, and nails depend on a well-balanced diet. Protein and vitamin deficiencies leave skin and hair dull, dry, and flaky. Minerals such as iron, copper, and zinc are necessary for the prevention of abnormal skin pigmentation and for the changes in hair and nails (Craven & Hirnle, 2004). Starvation can cause excessive hair loss and nail deformities.
Nails normally reflect a pinkish tone because of rich vascular areas in the fingers. When gentle pressure is applied and released, the nail becomes lighter white, but quickly returns to a pink color. Unhealthy nails may point to poor circulatory status, several nutritional deficiencies, and emotional conditions.
Nursing Alert Nail biting is often a nervous habit. Caution clients against nail biting because it can lead to serious infections.
Sebaceous or Oil Glands
The sebaceous glands (oil glands) lie close to the hair follicles, into which they usually drain (see Fig. 16-1). Sebum is the oily secretion of these glands; it travels to the surface of the skin through the hair follicles. Sebum helps make the skin soft and the hair glossy. As a defense mechanism, sebum prevents drying of the skin, thereby protecting it from cracking. Cracked areas in the skin are an invitation to invasion by microorganisms and other substances. Sebum also helps to waterproof the top layer of the epidermis (the stratum corneum). The activity of the sebaceous glands increases at puberty. Sebum may trap bacteria in the skin’s pores, causing inflamed or infected glands, commonly known as pimples or acne.
Special Considerations: LIFESPAN
Sebaceous Glands
Aging decreases the activities of the sebaceous glands; therefore, older skin is transparent, more dry than youthful skin, and more fragile (friable). This occurrence is due to a flattening of the epidermal and dermal skin layers and a thinning of the dermal layers, which predisposes an older adult to skin tears. A decrease in glandular secretions also causes drying of the skin.
Sudoriferous or Sweat Glands
The sudoriferous glands (sweat glands) are located in the dermis. One inch of skin contains 750 to 2,000 sweat glands. There are three types of glands: apocrine, eccrine, and mammary glands. The first two types respond to heat and stress. Your body is sweating constantly, often in minute amounts.
Apocrine sweat glands become active during puberty, secreting a thick, oily, milky sweat into the hair follicle. The apocrine glands are most numerous in the axillae, pubic region, areolae of the breasts, external ear canals, and eyelids. The nominal odor from these glands gives each person an individual scent. Skin surface bacteria cause the apocrine sweat to become odoriferous. A “cold sweat” occurs when emotional stressors, such as anxiety or fear, stimulate these glands.
The second type, eccrine sweat glands, are glands distributed widely over the body, but are especially numerous on the upper lip, forehead, back, palms, and soles. Eccrine glands secrete sweat into numerous ducts that empty into pores (tiny holes in the skin) and respond to external and internal heat. Perspiration (sweat) is nearly 100% water, with trace amounts of urea, uric acid, salts, and other elements. The primary function of perspiration is to assist in the regulation of body temperature by providing a cooling effect. Perspiration also moisturizes the skin’s surface and excretes waste products through the skin’s pores. In some disease states, the skin increases its capacity as an excretory organ, which may be a sign of pathology. (Diaphoresis refers to excessive perspiration.)
Key Concept When sweat joins with sebum, the secretion is a thick, sticky, protective film.This film on the fingers helps a person to pick up items with the fingers.
Mammary glands are a third, specialized type of sudoriferous gland. They secrete milk.
Ceruminal Glands
Ceruminal glands are specialized glands found only in the skin of the external auditory meatus, a passage that leads into the ear. The function of these glands is to protect the tympanic membrane (eardrum), which is essential to hearing. Cerumen (ear wax) that accumulates excessively may impair hearing and promote infection in the ear canal. The moisture content of cerumen varies somewhat among people of differing ethnic backgrounds.
Special Considerations : CULTURE & ETHNICITY
Cerumen
Dry cerumen (gray, brittle, and flaky) occurs most often in Native Americans (84%), Alaska Natives, and people of Asian descent. The remaining 16% have wet cerumen. Wet cerumen (dark brown, moist, and sticky) occurs most often in African Americans (99%) and whites (97%). Do not confuse these differences with physical disorders. For example, flakes of cerumen can be mistaken for the dry lesions of eczema or psoriasis.