White Blood Cells
About 1% of blood volume in the healthy adult consists of WBCs, also known as leukocytes (leuko = white; cyte = cell), because they do not contain hemoglobin. All leukocytes are derived from a cell in the bone marrow known as a hematopoietic stem cell. They are widespread throughout the body, including the blood and lymphatic system. WBCs defend the body against disease organisms, toxins, irritants, and other foreign materials. They differ greatly from RBCs. WBCs are larger than RBCs, contain nuclei, and can move independently in an ameboid fashion. WBCs also assist in repairing damaged tissues. Sometimes they die during this activity and collect with bacteria to form pus. Other characteristics of WBCs are presented in Box 23-3. The two types of WBCs are granular and agranular.
NCLEX Alert Basic knowledge of the hematologic and lymphatic systems will facilitate your understanding of diagnostic tests and lab values that may be included throughout the NCLEX.
Granular Leukocytes (Granulocytes). Granular leukocytes are also called polymorphonuclear leukocytes (PMNs) or segmented neutrophils (segs) because their nuclei have so many lobes or the lobes are so divided as to look like more than one nucleus. In granulocytes, membrane-bound enzymes aid in digestion of foreign particles in a process called endo-cytosis (phagocytosis) (Fig. 23-2). Granulocytes are divided into three subgroups: basophils, eosinophils, and neutrophils,based on their staining properties.
BOX 23-3.
White Blood Cells
♦ An abnormal number or character of leukocytes often indicates disease. For example, in leukemia, there is an increase in leukocytes or they are immature.
♦ The pus which forms in wounds contains an abnormally large number of leukocytes.
♦ A reduced number of leukocytes is called leucopenia (leukocytopenia). This may be caused by a disease process or as an unwanted side effect of certain medications, such as chemotherapy for cancer and clozapine.
♦ Some leukocytes migrate to specific tissues and remain there; they are called fixed leukocytes. Some of these are Kupffer cells (in the hepatic [liver] system), histiocytes (large macrophages), mast cells (in connective tissue), and microglia (which attack waste products in the nervous system).
FIGURE 23-2 • Phagocytosis. (A) Leukocytes squeeze out of blood vessels and rush to the site of an invading organism. (B) When foreign matter (e.g., bacteria or dead tissue [shown here as a streptococcus]) comes in contact with the cell membrane of the neutrophil, the cell membrane surrounds and pinches off the area, leaving the membrane intact. (C) Consequently, the engulfed material is enclosed in a membranous vesicle within the neutrophil, where enzymes within the cell destroy the foreign material.
• Basophils are involved in allergic and inflammatory reactions. They contain heparin (an anticoagulant) and release histamine. Histamine, along with other substances, acts on foreign invaders in the body. These substances cause an inflammatory or hypersensitivity reaction, resulting in vasodilation and edema, itching, and possibly bronchial constriction. This is an allergic or inflammatory response.
• Eosinophils are characterized by speckled or grainy cytoplasm and survive only about 12 hours to 3 days. They increase in number during allergic reactions and parasitic infections and are believed to release chemicals to assist the body in detoxifying foreign proteins or engulfing and devouring invaders. The term endocytosis involves both phagocytosis (engulfing of particulate matter) and pinocyto-sis (engulfing of extracellular fluid materials). Eosinophils may also have a role in decreasing the release of chemical mediators during allergic reactions.
• Neutrophils are the most numerous WBCs. These are the granulocytes most commonly called PMNs (polymorphonu-cleocytes). Because they are segmented (containing multiple lobes), they are also called segs. Neutrophils are colorless, unless they are stained to be visible under a microscope. They are considered to be first in the line of defense against bacteria. They also defend against fungi, in some measure. Because of their ability to move away from blood vessels, neutrophils can move directly to sites of infection or damaged tissues, as a result of their attraction to specific chemicals (chemotaxis). They push or squeeze through the capillary wall and rush to the threatened spot. There, they increase in number and engulf and devour invaders (endocytosis). Neutrophils increase in number during bacterial infections, burns, or inflammation. Because they have a short lifespan (approximately 10 hours), they need to be replaced frequently. When an infection occurs, more neutrophils are released from bone marrow. When the demand for these granulocytes is very high, the bone marrow releases immature neutrophils called bands. When looking at WBC counts, an increased number of bands signifies an infection. This increase in bands may also be described as a “shift to the left.”
Key Concept Blood cells have a short lifespan and are constantly being manufactured in the body The average lifespan for specific cells is:
• Red blood cells: 120 days
• Eosinophils: 12 hours to 3 days
• Neutrophils: 10 hours
• Monocytes and lymphocytes: 100-300 days
Agranular Leukocytes (Agranulocytes). These are divided into two subgroups: lymphocytes and monocytes (mononuclear leukocytes). Under normal conditions, agranular leukocytes are functional for about 100-300 days. They are produced in the lymphatic tissue of the spleen, lymph nodes, and thymus, and in the hemopoietic tissues in red bone marrow.
• Lymphocytes mature in the bone marrow and can be differentiated into various types. The most important of these are B-lymphocytes (B-cells) and T-lymphocytes (T-cells). B-cells make antibodies that bind to pathogens so they can be destroyed. T-cells are of several types. CD4, or “T-helper cells,” coordinate the immune response. CD8 cells are cytotoxic (cell-destroying) and can kill viruses, infected cells, and tumor cells. Natural killer cells can kill special cells which are Lymphocytes increase in number during infectious processes, particularly those caused by viral infections or immune diseases.
• Monocytes are characterized by the absence of granules in their cytoplasm, except for lysosomes. They play a role in acute and chronic inflammatory processes. They move from the bloodstream to other tissues, where they are transformed into macrophages or dendritic cells. (Dendritic cells function to activate T-lymphocytes.) The monocytes also “clean up” after phagocytosis, as well as present fragments of pathogens to the T-cells so they can be killed or so antibodies can be formed. A high monocyte count may be caused by a viral or fungal infection, tuberculosis, or certain chronic diseases.
• Macrophages are phagocytic cells, as are the neutrophils. They engulf and digest cellular debris and pathogens after phagocytosis. They also stimulate lymphocytes and other immune cells to perform their functions.
Platelets
Platelets, also called thrombocytes (thrombo = clot; cyte = cell), are the smallest of the elements formed by the blood and they are essential in blood clotting. They are not whole cells, but rather are fragments of larger cells. They lack nuclei, but are capable of ameboid movement. They are formed in red bone marrow.
Blood Clotting and Hemorrhage
Hemostasis refers to the cessation of bleeding (heme is commonly used to denote blood; stasi = stopping). When damage or rupture occurs to blood vessels, the hemostatic response must be quick and carefully controlled, to stop excessive blood loss. The hemostatic initial response includes vascular spasm (vasoconstriction), platelet plug formation, and blood clotting (i.e., the coagulation process that forms a fibrin clot) (Porth, 2004).
Clotting
Blood clotting protects the body from losing vital plasma fluid and blood cells by sealing off broken blood vessels. Without this action, individuals would not survive even minor cuts and wounds. The process of clot formation involves a number of complex activities within the blood, some of which are not totally understood.
When a blood vessel is disrupted, the subendothelium proteins (mostly collagen) are exposed, causing circulating platelets to break down almost instantly and release the chemical, thromboplastin. Thromboplastin binds collagen with specific glycoprotein receptors and other circulating proteins and calcium ions to form prothrombin activator. When this activates the platelets, granules of adenosine diphosphate (ADP), serotonin, platelet-activating-factor (PAF) and other substances are released into the plasma. This activates more platelets and causes a chain reaction, the coagulation cascade of secondary hemostasis. During this process, calcium ions are introduced and the plasma protein prothrombin is converted to thrombin. Thrombin then activates various amino acid factors involved in clotting and specifically converts the soluble plasma protein fibrinogen into insoluble threads of fibrin (the “building block” of the hemostatic plug). The threads of fibrin form a net to entrap RBCs and platelets to form a clot. This clot acts like a plug in a hole and tends to draw injured edges together. As the clot shrinks, a clear yellow liquid called serum is squeezed out. Serum is like plasma, except that fibrinogen and other clotting elements needed in the coagulation process are now absent.
Coagulation is a complicated mechanism that cannot occur if any necessary elements are missing. Vitamin K is necessary for the formation of prothrombin and other clotting factors. (Bacteria in the colon produce most vitamin K.) Figure 23-3 briefly introduces the human clotting mechanism.
A thrombus is a stationary clot. An embolus is a clot that circulates. Both of these clots can lead to death if they plug arteries to the heart, lungs, or brain. Several medications are available to treat blood clots and they are discussed in Unit 9.
Key Concept The initial response to a disruption in a blood vessel includes vascular spasm (vasospasm), platelet plug formation, and the coagulation process that forms a fibrin clot. Platelets, calcium ions, and vitamin K are important elements in this complex coagulation process.
Hemorrhage
The literal definition of hemorrhage is escape of blood from blood vessels; however, hemorrhage is usually thought of as the loss of a considerable amount of blood from a cut or torn vessel. Hemostatic mechanisms, such as clotting, help to prevent hemorrhage in smaller vessels, but extensive hemorrhage from larger vessels requires medical intervention. In severe hemorrhage, the body loses so much fluid and oxygen-carrying RBCs that death could result. Inability to clot in extensive hemorrhage may be caused by a variety of factors: force behind the flow of blood, size of the wound, volume of blood lost, or a deficiency in any of the coagulant components. Severe hemorrhage must be stopped and the person often receives blood replacement, using blood or blood components from another person. This is called a transfusion.
Key Concept Often, more blood is lost froma torn or nicked blood vessel than from a vessel that is cleanly cut through. The muscles in a blood vessel contract as a protective measure. If these muscles are cut unevenly they cannot effectively close the vessel.
Hemorrhage from an artery comes in spurts. Hemorrhage from a vein comes in a steady flow
Blood Groups
Human blood falls into one of four groups (blood types): A, B, AB, and O (Table 23-2). These blood types are inherited (genetic) combinations of antigens and antibodies found on the membranes of RBCs. The type and crossmatch test compares donor and recipient cells to check for agglutination (clumping of cells). If an incompatible type of blood is given to a person, a fatal transfusion reaction may result. Except for blood types, no differences exist in the blood of healthy people of different races or genders. Blood does not carry or transmit mental, emotional, or physical characteristics.
Key Concept Glycoproteins, including glycophorin C, exist on the surface of RBCs. Blood types are due to variations in these surface glycoproteins.
FIGURE 23-3 • The coagulation cascade of secondary hemostasis (blood clot formation). Most coagulation factors are enzymes; some are glycoproteins (e.g., transglutaminase).
TABLE 23-2. Blood Groups and Compatibilities
|
BLOOD GROUP |
PERCENT OF POPULATION |
ANTIGEN ON ERYTHROCYTES |
ANTIBODY IN PLASMA |
CAN DONATE RED BLOOD CELLS TO |
CAN RECEIVE RED BLOOD CELLS FROM |
|
A |
41% |
A |
Anti-B (reacts against B antigen) |
A or AB |
A or O |
|
B |
10% |
B |
Anti-A (reacts against A antigen) |
B or AB |
B or O |
|
AB ("universal recipient”) |
4% |
A and B |
None |
AB |
A, B, AB, or O* |
|
O ("universal donor”) |
45% |
None |
Anti-A and Anti-B (reacts against both A and B factors) |
A, B, AB, or O^ |
O |
*Blood group AB is known as the universal recipient, because people of this group may receive red blood cells from donors of any ABO group in an extreme emergency
^Blooc group O is known as the universal donor because these red blood cells may be given to people of any ABO group in an extreme emergency
Rh Factors
Just as with a blood group, Rh factors are inherited antigens. (The Rh system is named after the Rhesus monkey used in early experiments.) Of the several types of antigens that may be found on the surface of RBCs, more than 90 are loosely connected to the Rh system. The most commonly found Rh factor and the one most likely to cause a transfusion reaction is abbreviated D (Duffy). Blood is tested for the presence of D antigen. If the blood contains D factor, the person is said to be Rh-positive (Rh+ or D + ); if this factor is absent, the person is Rh-negative (Rh-). The percentage of Rh-negative people is lower within some ethnic groups; approximately 2%-7% of African Americans and 1% of Asians and Native Americans are Rh-negative, whereas more than 10% of Caucasians are Rh-negative. When an Rh-negative person receives Rh-positive blood, he or she develops antibodies that could cause a severe reaction to subsequent blood transfusions. This can also occur with an Rh-positive pregnancy in an Rh-negative mother. (Unit 10 discusses in more detail the Rh factor and its effects on pregnancy.)
LYMPH
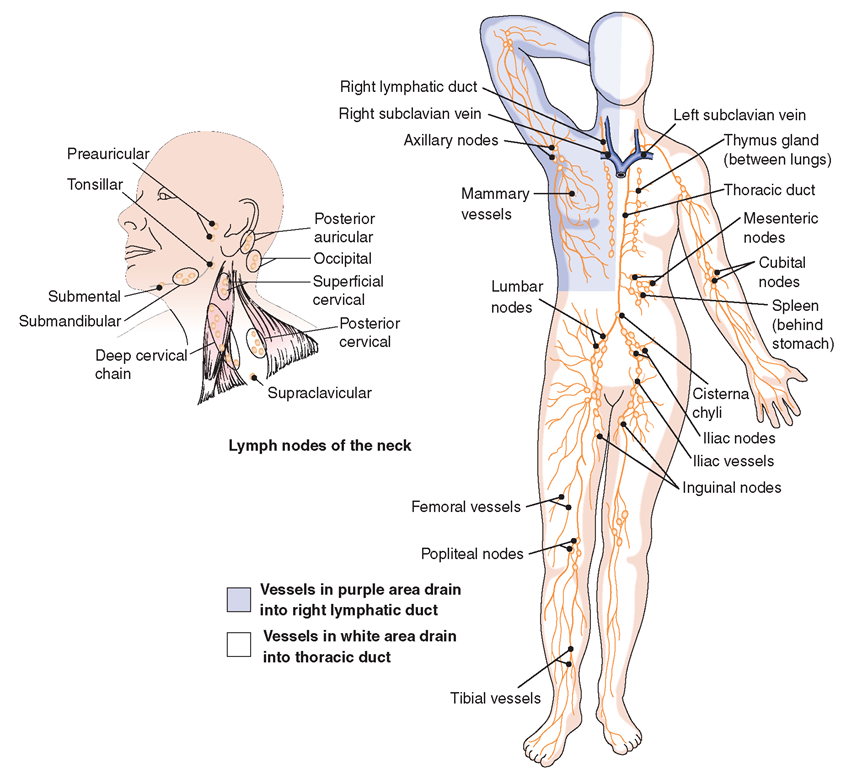
The lymphatic system is related to, yet separate from, the hematologic system (Fig. 23-4). The lymphatic system is sometimes referred to as the secondary circulatory system. It includes the lymphatic conduits and specialized lymphoid tissue. Lymphoid follicles are regions of specialized lymphoid tissue densely packed with lymphocytes and some other white blood cells, enmeshed in connective tissue. (As lymph passes through this tissue, damaged cells and waste materials are filtered out.) Lymphoid tissue may be organized into lymph nodes or may be loosely organized tissue known as mucosa-associated lymphoid tissue (MALT).
The primary lymphatic system consists of the thymus gland and the bone marrow (involved in production and early selection of lymphocytes). The secondary lymphatic system consists of encapsulated tissue (the spleen and lymph nodes covered with connective tissue) and non-encapsulated tissue (intestinal lymphoid tissue and tonsils). The lymph nodes and lymphoid follicles of the tonsils provide an environment for antigens to interact with lymphocytes. Peyer’s patches are MALT areas in the digestive system. Some researchers have identified a tertiary lymphoid system which only functions when antigens cause inflammation. It must import lymphocytes to function in this manner.
FIGURE 23-4 · The lymphatic system.
Functions of the lymphatic system include:
• Immune response—defense against infection and prevention of metastasis of malignant tumors
• Removal of excess interstitial fluid from tissues
• Absorption and transport of fatty acids and fats (as chyle) to the circulatory system
• Transport of antigen-presenting cells (APC), such as dendritic cells, to lymph nodes, to activate an immune response.
![Phagocytosis. (A) Leukocytes squeeze out of blood vessels and rush to the site of an invading organism. (B) When foreign matter (e.g., bacteria or dead tissue [shown here as a streptococcus]) comes in contact with the cell membrane of the neutrophil, the cell membrane surrounds and pinches off the area, leaving the membrane intact. (C) Consequently, the engulfed material is enclosed in a membranous vesicle within the neutrophil, where enzymes within the cell destroy the foreign material. Phagocytosis. (A) Leukocytes squeeze out of blood vessels and rush to the site of an invading organism. (B) When foreign matter (e.g., bacteria or dead tissue [shown here as a streptococcus]) comes in contact with the cell membrane of the neutrophil, the cell membrane surrounds and pinches off the area, leaving the membrane intact. (C) Consequently, the engulfed material is enclosed in a membranous vesicle within the neutrophil, where enzymes within the cell destroy the foreign material.](http://what-when-how.com/wp-content/uploads/2012/08/tmp696761_thumb.png)