Middle Lobe
The most important hormone secreted by the middle lobe (pars intermedia) of the pituitary is melanocyte-stimulating hormone (MSH), which is stimulated by CRH from the hypothalamus. MSH influences skin pigmentation and is chemically similar to ACTH (produced in the anterior lobe). The hypothalamus inhibits secretion of MSH by secreting melanocyte-inhibiting factor (MIF).
Posterior Lobe
The posterior lobe of the pituitary, also called the neurohypophysis, is actually an outgrowth of the hypothalamus and is embryonically derived from the nervous system. Hormones are not secreted there but are stored and released. The hypothalamus and pituitary gland are in close proximity to each other. The two hormones released by the posterior lobe, oxytocin and vasopressin, are secreted in the hypothalamus by neurosecretory cells, and then released by the neurohypophysis (see Fig. 20-2).
Oxytocin (from neurosecretory cells) stimulates the uterus to contract during delivery and helps to keep it contracted after delivery (to prevent hemorrhage). It also stimulates the release of milk from a new mother’s breasts. It is also involved in orgasm and circadian homeostasis (body temperature, wakefulness, and activity level).
Vasopressin or antidiuretic hormone (ADH or AVP) functions in several ways. It stimulates contraction of blood vessels to raise blood pressure; affects the uterus; and influences reabsorption (resorption) of water by the kidney tubules. Table 20-3 lists the actions of these two hormones.
Key Concept Although there are subtle differences in the definitions of reabsorption (the term used in this topic) and resorption, these terms are often used interchangeably to mean the reuse of materials, such as proteins, glucose, and electrolytes, to restore essential components to the body An example of this process is the selective reabsorption of extracellular fluid in the tubules of the kidney
Thyroid Gland
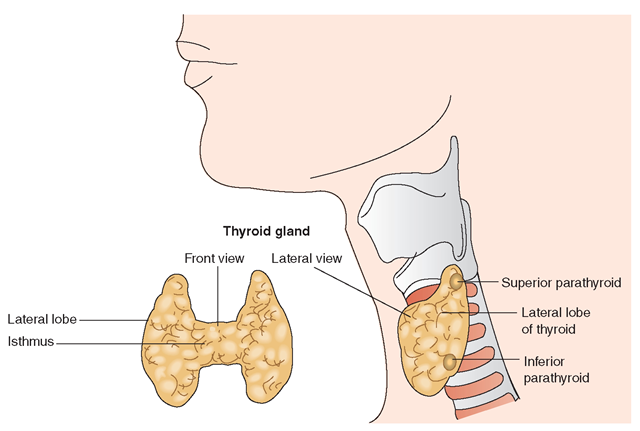
The thyroid gland, the largest of the endocrine glands, lies in front of the neck, just below the larynx, with a wing (lobe) on either side of the trachea (Fig. 20-3). The epithelial cells of the thyroid secrete two hormones: thyroxine (tetraiodothyronine or T4) and triiodothyronine (T3). These hormones are synthesized in the thyroid gland from iodine. T4 is the less potent form of thyroid hormone. More T4 (90%) is found in the blood, compared with T3 (10%). It is believed that T4 is converted to T3 before it can work in the body. These hormones regulate body metabolism, controlling the rate at which cells do their work. Protein synthesis relies on these hormones. In addition, they affect sensitivity to catecholamines and sympathetic amines, such as dopamine and epinephrine. The catecholamines are important in the body’s response to stress.
Because the thyroid removes iodine from the blood to make T4, a person’s diet must supply iodine.
Special Considerations :NUTRITION
Iodine food sources include shellfish and iodized salt. Residents of inland states are often advised to use iodized salt. A lack of iodine in the body could cause a decrease in thyroid function over a period of time. Common symptoms a healthcare provider could see in a client with decreased thyroid function are fatigue, weight gain, and complaints of being cold. Goiter is often a later consequence of insufficient iodine.
FIGURE 20-3 · The thyroid gland as viewed frontally and laterally. The lateral view also shows the location of the parathyroid glands. The thyroid gland is made up of follicles, each containing an outer wall of follicular cells, with colloid material inside.
If there is insufficient dietary intake of iodine, a disorder called a goiter (an enlarged thyroid gland) may result. In this case, the hypothalamus secretes a hormone called thyroid-stimulating hormone (TSH). When excess TSH is secreted, it causes the thyroid gland to enlarge.
Another hormone, secreted in the parafollicular cells of the thyroid, is calcitonin or thyrocalcitonin. It is involved in the maintenance of the body’s calcium levels. When circulating calcium levels are high, calcitonin responds by promoting increased storage of calcium in bones and increased renal excretion of calcium, resulting in lowered serum calcium levels.
Parathyroids
The parathyroids are small glands, each about the size of a pea, that lie on either side of the undersurface of the thyroid gland (see Fig. 20-3). Usually, there are four, in two pairs; despite their relatively small size, the parathyroids are essential to health and to life itself.
The chief cells of the parathyroids secrete a hormone, parathormone or parathyroid hormone (PTH), that regulates the amounts of calcium and phosphorus in the blood, which in turn affect nerve and muscle irritability. When the blood calcium level is too low, parathormone is secreted. This secretion increases the number and size of osteoclasts (large cells associated with reabsorption of bone). Therefore, parathormone causes calcium to leave the bones. PTH also enhances reabsorption of calcium and magnesium and excretion of phosphorus in the kidneys.
Parathormone has an additional effect on the kidneys in that it promotes the formation of calcitriol, a hormone synthesized from vitamin D. Calcitriol increases the rate of calcium, magnesium, and phosphorus absorption from the gastrointestinal tract into the blood. Therefore, PTH has the opposite action of calcitonin.
Nursing Alert A client with severe calcium deficiency may exhibit muscle twitching and spasms, and possibly seizures. These signs are called tetany.
Adrenal Glands
The two adrenal glands, also known as the suprarenal glands, sit like hats, one atop each kidney (see Fig. 20-1). As with the pituitary gland, the adrenal glands each have two parts; each part produces different hormones.
Adrenal Medulla
The central portion of the adrenal gland, called the medulla, secretes hormones called catecholamines, which are made from amino acids. Epinephrine and norepinephrine are produced in the chromaffin cells and are catecholamines. Epinephrine (adrenaline) constitutes about 80% of the medulla’s total secretion. Its actions are to make the heart beat faster, contract blood vessels, raise blood pressure, and increase muscle power by causing the liver to release glucose for energy. The hormone norepinephrine has some— but not all—the actions of epinephrine. These two hormones mimic the action of the sympathetic nervous system.
However, the adrenal medulla is not necessary for life, because the sympathetic nervous system can take over its activities. These hormones are active in emergencies; fright, anger, love, and grief stimulate them. They are said to prepare people for “fight or flight.” The functions of the adrenal medulla are important in management of and adaptation to stress.
Key Concept Epinephrine and norepinephrine are major catecholamines and are involved in “fight or flight."
Dopamine, also produced in the chromaffin cells, acts to increase heart rate and blood pressure. Another type of substance from the same cells, the enkephalins, helps to regulate pain. These substances also function as neurotransmitters, are involved in movement, mood, and behavior, and are found in a number of locations in the body.
Adrenal Cortex
The zona fasciculata, reticularis, and glomerulosa, which are cells of the outer part of the adrenal glands (the adrenal cortex), secrete many compounds called corticosteroids or corticoids. Three types of corticosteroids exist: mineralocor-ticoids, glucocorticoids, and the sex hormones (male: androgens—testosterone and dehydroepiandrosterone (DHEA); female: estrogens). All these compounds derive from cholesterol.
Mineralocorticoids regulate the amount of electrolytes in the body. Aldosterone, the most important mineralocorti-coid, stimulates reabsorption of sodium into the plasma and secretion of potassium and hydrogen in the kidney. This action results in increased water reabsorption and, therefore, an increase in blood volume.
Glucocorticoids have an important influence on the synthesis of glucose, amino acids, and fats during metabolism. They also depress the immune response and decrease the inflammatory response. Corticosteroid production is normally increased during times of stress. Hydrocortisone (cortisol) is the predominant glucocorticoid.
Nursing Alert Clients taking glucocorticoids often experience lengthened healing times and may have a decreased response to infections owing to the drug’s antiinflammatory and immunosuppressive response. Therefore, consider a small rise in temperature a significant finding in these clients.
The sex hormones of the adrenal cortex (androgens, estrogens, and progestins) supplement the sex hormones of the gonads. The adrenals primarily produce androgens, with only minute amounts of estrogen and progesterone secretion. Table 20-3 identifies selected steroids and their functions. In recent years, the abuse of anabolic steroids (synthetic derivatives of testosterone) has been increasingly reported, particularly in relation to sports.
Nursing Alert Look for the classic signs in clients taking glucocorticoids. These signs are a result of redistribution of fat in the body giving the client an appearance of being overweight or obese. They include a round face ("moon face”), a large abdomen, and a hump on the person’s back ("buffalo hump”).
Pineal Gland
The pineal gland (pineal body) is a small, cone-shaped structure located at the top portion of the brain’s third ventricle (see Fig. 20-1). It produces melatonin in cells called pinealocytes. Melatonin production is not completely understood, but is related to the amount of exposure to environmental light. Melatonin is an antioxidant and is thought to participate in the maintenance of the sleep-wake cycle. In sunlight, sympathetic nerve fibers release norepinephrine, which inhibits the secretion of melatonin and results in wakefulness. In darkness, the lack of norepinephrine stimulates the secretion of melatonin, resulting in sleepiness.
Melatonin or another pineal hormone may also regulate the release of substances from the hypothalamus that stimulate and affect the secretion of gonadotropin. Therefore, the pineal gland may influence reproductive functions. Theorists speculate that the amount of daylight animals receive regulates their pineal secretions, influencing their breeding seasons. The effect of daylight on humans is not well understood, but is believed to affect the brain and to influence the rate of gonad (ovary and testis) maturation.
Gonads
The gonads are the glands of reproduction: the testes of the male and the ovaries of the female (see Fig. 20-1). In addition to producing sperm, the Leydig cells of the testes produce testosterone, the male sex hormone. Other steroid hormones produce masculinizing effects; as a group, they are called androgens.
The female ovaries produce estrogen (primarily estradion) and progesterone, which, in addition to regulating female sex characteristics, are responsible for menstruation; they also influence pregnancy, labor, and lactation. In addition, progesterone has an influence on the gall bladder, blood clotting mechanisms, thyroid function, nerve function, and many other body functions.
Pancreas
The pancreas lies behind the stomach, between the duodenum and the spleen. It is both an endocrine and an exocrine gland. As an exocrine gland, it releases digestive enzymes into the duct system leading to the small intestine.
The endocrine portion of the pancreas exists in the 1 to 2 million small islands (islets) scattered throughout its body and tail. Within these islets, called the islets of Langerhans (pancreatic islets), are special types of cells that secrete pancreatic hormones. These cells are known as alpha, beta, delta, and F cells. The types of hormones secreted are glucagon, insulin, somatostatin, and pancreatic polypeptide (see Table 20-3).
Approximately 20% of the cells in the islets of Langerhans are alpha cells. Alpha cells secrete the hormone glucagon, which acts in opposition to insulin. (Glucagon raises blood sugar; insulin lowers blood sugar.) Glucagon is needed to break down glycogen (stored sugar) into glucose, a process called glycogenolysis. It also stimulates the breakdown of fats and proteins for conversion in the liver into additional glucose. This conversion of excess amino acids and fatty acids into glycogen, which is later released as glucose, is called gluconeogenesis.
Approximately 70% of the islet cells are beta cells. They secrete the hormone insulin, which is a protein substance. Insulin is the key regulator of carbohydrate, protein, and fat metabolism and storage. The primary function of insulin is to control the blood’s glucose (sugar) level. Insulin accomplishes this task in several ways, as listed in Box 20-2. It has recently been discovered that the beta cells also secrete amylin, which responds to food intake and works with insulin and glucagons to help regulate glucose balance. Amylin acts especially during the few hours immediately after eating (postprandial period). It slows the production of glucose to the liver and serves to help the person feel full or satisfied (satiety) by sending a signal across the blood-brain barrier. (In type 1 diabetes, both insulin and amylin are not secreted. In type 2 diabetes, both hormones are produced, but in insufficient amounts.).
Approximately 5% of the cells within the islets are delta cells. Delta cells secrete somatostatin, which is identical to the growth hormone-inhibiting hormone (GHIH) secreted by the hypothalamus. Somatostatin inhibits the release of insulin and glucagon. The way this control mechanism operates is unknown. (Somatostatin is also secreted by the “D” cells of the stomach.) It suppresses the release of gastrin, cholecystokinin (CCK), secretin, motilin, vasoactive intestinal peptide (VIP), gastric inhibitory polypeptide (GIP), and enteroglucagon. Thus, it lowers the rate of gastric emptying and reduces smooth muscle contractions and blood flow in the intestines.
BOX 20-2.
Actions of Insulin to Control Glucose Level
♦ The major stimulus for synthesis and secretion of insulin is an elevated blood glucose level.
♦ Insulin increases the cell membrane’s permeability to glucose. After it is in the cell, glucose is used in cellular respiration to produce energy.
♦ Insulin stimulates the liver to convert extra glucose into glycogen (glycogenesis) and helps the liver and muscles to store glycogen. Glycogen is stored as body sugar, commonly referred to as animal starch.
♦ Insulin increases the transfer of amino acids across muscle membranes for synthesis into proteins.
♦ Insulin speeds fatty acid synthesis (lipogenesis) for fat storage.
♦ Insulin slows glycogenolysis (glycogen breakdown) and gluconeogenesis (formation of glucose from noncarbohydrate sources).
The remaining 5% of the islet cells are F cells or PP cells. F cells secrete pancreatic polypeptide, which is believed to inhibit the secretion of somatostatin and pancreatic digestive enzymes.
Key Concept Insulin is a hormone needed to transport glucose into cells to enable the cells to function. If there is a lack of insulin or if the insulin is not working as it should, an increased blood glucose level will result. A condition known as diabetes mellitus results when there is a disturbance in the oxidation or utilization of glucose (often the result of a malfunction of the beta cells of the pancreas). Because insulin is necessary for adequate functioning of the body medical intervention is necessary to manage diabetes mellitus.
Thymus
The thymus lies behind the sternum (breast bone). In infants and children, the thymus is relatively large. After puberty, the thymus becomes smaller, but little is known of the longterm effects of this phenomenon.
The thymus produces thymosin (thymic hormone), a protein that stimulates production of small lymphocytes called T cells (also called T lymphocytes, T helper cells, or thymus-dependent cells). The thymus also secretes other hormones believed to assist in the maturation of T cells. T cells are essential for the development of cellular immunity and the body’s response to invading organisms. If the T-cell count of a person is diminished, that person would have a diminished ability to fight off attacking pathogens. This type of diminished immune response may be seen in the person with acquired immunodeficiency syndrome (AIDS) or in the client undergoing cancer chemotherapy.
Other Sites That Secrete Hormones
Gastrointestinal Tract
The G cells of the stomach secrete a hormone called gastrin, and the ECL cells secrete histamine; both stimulate the gastric glands (parietal cells) to secrete gastric juice. Gastric juice contains gastric acid, which aids in digestion. Other cells in the stomach produce ghrelin and neuropeptide Y (NPY). Their effects are listed in Table 20-3. Somatostatin is secreted by the D cells, as previously discussed.
The lining of the upper part of the small intestine secretes hormones (pancreozymin, secretin) that stimulate the pancreas to release pancreatic juice and another hormone that regulates the release of bile from the gallbladder and causes the gallbladder to contract (cholecystokinin). The cells lining the ilium and colon also secrete the human incretin hormone, glucagon-like peptide-I (GLP-I), which encourages the pancreas to secrete insulin.
Liver
The hepatocytes of the liver produce several hormones. These include insulin-like growth factor (somatomedin, IGF), which has insulin-like effects in regulating cell growth and development. Two other hormones produced by these cells are angiotensinogen, which, on hydrolysis by renin, gives rise to angiotensin-converting enzyme (ACE). These two hormones cause vasoconstriction, rising blood pressure, and the release of aldosterone from the adrenal cortex. Yet another hormone produced by the hepatocytes is thrombopoietin, which stimulates the production of platelets. This hormone is also present in the kidneys and striated muscles.
Placenta and Uterus
The placenta is a temporary endocrine gland that secretes hormones to assist in maintaining pregnancy. These hormones include estrogen, progesterone, and human chorionic gonadotropin (HCG). The pregnant uterus also secretes prolactin, which influences the production of milk after delivery.
Key Concept The presence of elevated levels of HCG in a pregnant woman’s body provides the basis for commonly used tests to determine pregnancy
Kidneys
A structure within the kidney called the juxtaglomerular apparatus produces a hormone called renin (part of the renin-angiotensin-aldosterone [RAA] mechanism), which acts on the vascular system to assist in blood pressure control (see Fig. 27-5). Erythropoietin (renal erythropoietic factor) is a glycoprotein (protein and carbohydrate combination) hormone produced in the extraglomerular mesangial cells of the adult’s kidneys and in the child’s liver. Erythropoietin stimulates red blood cell production. Also secreted in the kidneys is calcitriol, an active form of vitamin D3, which influences absorption of calcium and phosphate.
Heart
Atrial natriuretic peptide (ANP), or atrial natriuretic factor (ANf), is a hormone produced in the cardiac myocytes in the atrium of the heart as a protective mechanism. (The term natriuretic refers to sodium excretion.) ANP helps to maintain fluid homeostasis and to regulate blood pressure. It does this by acting on the kidneys to inhibit renin secretion, which inhibits the production of angiotensin. ANP inhibits aldosterone secretion and also reduces vascular resistance in the body and lowers the content of fats in the blood. The result of these actions is to inhibit sodium reabsorption and to promote diuresis (the secretion of large amounts of urine). The result of this excretion of sodium and water is a lowering of blood pressure, which reduces the workload of the heart and lowers stress on the blood vessels.
Another hormone secreted in the same cells is brain natriuretic peptide (BNP), which also reduces blood pressure, but to a lesser degree than does ANP.
Other Specific Hormone Production
In addition to cells in the liver, myocytes in voluntary (striated) muscles secrete thrombopioetin, which stimulates the production of platelets. Adipocytes in fatty tissue produce leptin, which causes a decrease in appetite and increased metabolism.
Most Tissues
Leukotrienes. Hormones that are very involved in the body’s inflammatory process are called leukotrienes (LTs). The inflammatory process can result in bronchoconstriction and anaphylaxis (similar to histamine, except that leukotrienes are released at a slower rate). Drugs have been developed to decrease the amount of leukotrienes in the body in different ways. These drugs, called leukotriene inhibitors, are being used to prevent asthma attacks.
Prostaglandins. The prostaglandins are specialized fatty acids that were first isolated in the seminal fluid of the prostate, from which their name is derived. They are widespread in the body’s tissues. Prostaglandins are not hormones, but rather are hormone-like substances that share characteristics with hormones and neurotransmitters. The effects of prostaglandins are localized to the area in which they are produced. They can cause pain, they perform a role in platelet function, and stimulate either contraction or relaxation in the smooth muscle. The prostaglandins influence blood pressure, respiration, digestion, and reproduction— and in some cases, actually can have opposite effects on these functions. For example, one prostaglandin may cause dilation of the bronchioles, whereas another may cause constriction. Extensive research relating to prostaglandins is being conducted to determine their specific functions. The possibility exists that many disorders may be treated in the future by the administration of substances that control prostaglandin secretion. A current over-the-counter medication called ibuprofen is a prostaglandin inhibitor. It works primarily as an anti-inflammatory agent, by inhibiting production of prostaglandin.
SYSTEM PHYSIOLOGY
NCLEX Alert The NCLEX requires under standing of the interdependence of normal and abnormal functioning of the body’s systems. The correct option will most commonly reflect a priority of needs for the body as a whole.
System Relationships
The endocrine system is closely related to many other body systems. One prominent relationship is that with the nervous system. These two systems cannot be separated anatomically or functionally. Each needs the other for optimum performance. Therefore, these systems are interdependent (one system cannot work without the other). For example, certain parts of the nervous system stimulate or inhibit the release of hormones. Likewise, hormones promote or inhibit the generation of nerve impulses. These two systems are also similar in function because they both stimulate and control body actions. Generally, the effect of nerve stimuli is immediate and lasts only as long as the stimulation is present. The action of a hormone is slower, with more prolonged stimulation or regulation. Table 20-4 lists various modes of signaling within the endocrine system.
The endocrine and circulatory systems are also interdependent because hormones travel from the glands through blood and lymph. The endocrine and digestive systems also rely on one another. One example is the secretion of insulin by the endocrine system, which enables the digestive system to use glucose and glycogen from foods.
TABLE 20-4. Signaling Within the Endocrine System
|
TYPE OF SIGNALING |
EFFECT |
|
Endocrine |
Hormone carries the signal. |
|
Paracrine |
Hormone binds to nearby receptor— target cell—and affects their function. |
|
Autocrine |
Hormone affects the same cell that produced it; targets the same cell. |
|
Neuroendocrine |
Interaction occurs between nervous and endocrine systems in response to stimulus from both systems. |
|
Neurocrine |
Signaling occurs between neurons within the nervous system; endocrine influence on or by the nerves (neurosecretion). |
|
Juxtacrine |
Signals transmitted along cell membranes via proteins or lipids; can affect adjacent cell or same cell. |
Information Relay to Target Cells
The hypothalamus and anterior and middle pituitary are components of a unit that can be called an “information relay system.” Specialized cells in the hypothalamus respond to changes in the internal and external environments. Their response is to secrete hormones (see Table 20-2) that directly stimulate or block the release of hormones from the anterior pituitary (e.g., CRH stimulates the release of ACTH; MIF blocks the release of MSH). The hormones secreted by the hypothalamus and released from the anterior and middle lobes of the pituitary then travel through the bloodstream to certain target tissues. These hormones usually bind to receptors on the target tissues in a “lock-and-key” fashion. (There is only one location and only one way possible for them to fit together or bind.) The response of the target cells to the hormone then involves the acceleration or inhibition of certain biochemical processes.
Negative and Positive Feedback
The fine balance within the endocrine system called feedback regulates the rate and quantity of hormone secretion.
Negative feedback receptors (e.g., glands) require close monitoring by the cells of the body in order to maintain the desired amount of hormones. After the desired effect is achieved, information is sent to the gland to halt secretion of the hormone. This is a negative feedback system or negative feedback loop, because the body has again achieved homeostasis. This situation will now cause an inhibited glandular response because the previous imbalance has been resolved.
TABLE 20-5. Effects of Aging on the Endocrine System
|
FACTORS |
RESULT |
NURSING IMPLICATIONS |
|
Overall effects of aging are unknown. Decreased production of and receptivity to hormones |
Individualized changes |
Monitor changes in metabolism or blood sugar levels. Be alert to symptoms of diabetes. |
|
There are few known changes. |
Notify physician of abnormal laboratory values. |
|
|
No generalized decreases occur, except in estrogen and testosterone levels. |
Monitor for problems related to osteoporosis. Sexual counseling may be helpful. |
|
|
Reproductive hormones decrease. |
Onset of menopause in middle age Women lose their ability to become pregnant Hirsutism in women |
Monitor for heart disease, which increases in women after menopause, with loss of estrogens. |
|
Atrophy of subcutaneous breast tissue Decreased sperm production |
Advise about facial hair removal. |
|
|
Sexual tissue atrophies. |
Loss of pubic hair Longer time needed for sexual orgasm Lessened amount of vaginal secretion |
Explain that libido is essentially unchanged. Lubricant may aid in comfortable intercourse; estrogen cream may be prescribed. |
|
Decrease in thyroid hormones. |
Decreased metabolic rate Thinning hair; male pattern baldness Dry skin |
Be aware that it may take longer to do daily activities. Be alert for complaints of feeling cold. |
|
Decrease in pancreatic secretions. |
Decreased ability to metabolize glucose |
Monitor weight. Counsel on exercise and proper nutrition. |
A positive feedback system or loop can also occur. For example, if there is a need for a hormone to meet the body’s needs, a message is carried to the appropriate gland. (This step is similar to the negative feedback system.) The result is an increase in hormone production. The desired effect (response) by the body does not cause the hormone secretion to cease (as in the negative feedback system) but allows it to continue and intensify. An example of a positive feedback system is exemplified by the hormone oxytocin, which is produced during labor. Oxytocin intensifies the contractions of the uterus and enables the uterus to expel the fetus.
Most body systems utilize negative and positive feedback systems. The goal of feedback systems in the body is to help promote homeostasis.
EFFECTS OF AGING ON THE SYSTEM
The major hormonal changes that occur with aging are associated with decreased insulin sensitivity at the cellular level; decreased production of thyroid hormone and its metabolic clearance rate; reduced testosterone production by the testes; and reduced estrogen production by the ovaries. The results of aging include a risk for disorders, such as diabetes mellitus, hyper- or hypothyroidism, and osteoporosis (a disorder that causes brittle bones, owing to decreased bone mass and decalcification). Reduced hormone production by other glands may also be seen as a result of the normal aging process. Table 20-5 summarizes the major effects of aging on the endocrine system.
The decline of sex hormones produces the most obvious effects of aging. In women, menopause (cessation of menstruation) begins in middle age with a decrease in estrogen levels. As a result, breast tissue changes from glandular tissue to connective and adipose (fat) tissue. The elasticity of the tissue decreases, and the breasts begin to sag. The uterus, uterine tubes, and external genitalia shrink with age. Hirsutism (facial hair) may occur.
In men, testosterone levels gradually decline from levels seen in young adulthood. Sperm production decreases. The ability to achieve erection, orgasm, and ejaculation remain but may take longer than in earlier years. These decreases in function have a more gradual onset than do the hormonal changes that occur in women.
Both men and women lose pubic hair. Impotence in men and a lack of sexual response in women are not natural results of aging. The desire for companionship, tenderness, and love remain as basic human needs.
Endocrine disorders can occur at any age, but are often more common in older people. Endocrine disorders are related to:
• Unregulated release of hormones
• Inappropriate response to hormonal signals
• Damage to an endocrine gland; absence of a gland
• Hypofunction or hyperfunction of a gland
• Dysfunction of the hypothalamus (which controls secretion and release of many hormones)
• Malignancy
NCLEX Alert It will be important to understand the relationship of the endocrine system to a client’s status and treatment of specific diseases (especially diabetes mellitus), neoplasms, and injuries. The NCLEX may require knowledge of the infant, youth, adult, or older adult, all of whom may have specific, different needs.
KEY POINTS
• Endocrine glands secrete hormones directly into the bloodstream; exocrine glands secrete hormones into ducts.
• Hormones are chemicals that regulate, integrate, and coordinate body systems and functions.
• Many hormones are secreted in the hypothalamus; they, in turn, control the release of hormones by the pituitary gland.
• The many hormones released by the anterior, middle, and posterior pituitary have widespread effects on the body.
• The thyroid is responsible for controlling the body’s rate of metabolism; it affects calcium storage.
• The parathyroids regulate the amount of calcium and phosphorus in the blood; they activate vitamin D.
• The adrenal medulla secretes hormones that mimic the action of the sympathetic nervous system. Adrenal hormones are active in emergencies or in stressful situations.
• The adrenal cortex makes three types of steroid compounds from cholesterol: mineralocorticoids, glucocorticoids, and sex hormones. (These sex hormones supplement those secreted by the gonads, the glands of reproduction.)
• As an endocrine gland, the pancreas secretes insulin, which facilitates the lowering of blood sugar, and glucagon, which facilitates the raising of blood sugar. These substances also influence fat and protein metabolism.
• The thymus secretes hormones that play a role in cellular immunity.
• Melatonin, the hormone secreted by the pineal gland, helps regulate the sleep-wake cycle.
• Prostaglandins are hormone-like substances. Their effects are localized to the area in which they are produced. They influence blood pressure, respiration, digestion, and reproduction.
• The endocrine system has close interrelationships with other body systems.
• Negative and positive feedback mechanisms influence hormonal blood levels.
• Hormones are specific to target tissues and often act in a “lock-and-key” fashion.
• Other structures in the body, such as the heart, liver, kidneys, and digestive system, also produce specific hormones.
• During pregnancy, the placenta and uterus secrete hormones.
• Reduced hormonal production occurs as a part of the normal aging process.