ACCESSORY ORGANS
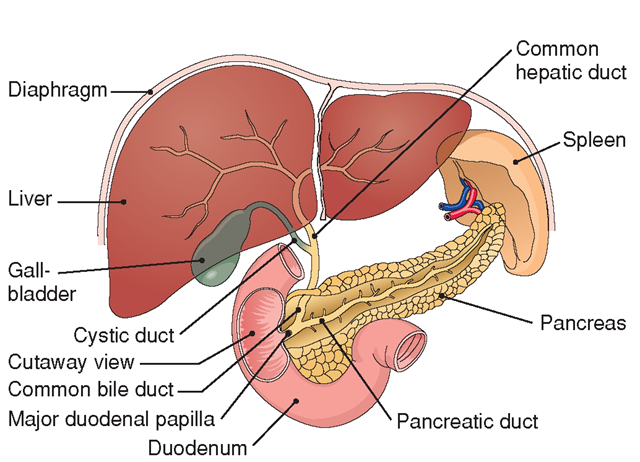
Accessory organs of the digestive system include the liver, gallbladder, pancreas, and peritoneum. Figure 26-6 shows the accessory organs of digestion.
Liver
The liver, the body’s largest glandular organ, lies just below the diaphragm in the upper right quadrant of the abdominal cavity. It receives its blood supply from the hepatic artery and is divided into two major and two minor lobes. (The prefix referring to the liver is hepat[o]-.) In humans, the liver weighs about 3 pounds (1.36 kg) and resembles calf liver in color and texture.
The liver plays such an important part in overall bodily functions that a person cannot live long if it is severely diseased or injured. Only the brain is capable of more functions than the liver. Some of the liver’s major functions include:
FIGURE 26-6 · Accessory organs of digestion.
• Absorption of bilirubin from the destruction of old red blood cells (RBCs)
• Detoxification of blood (removal of toxins or poisons)
• Storage of fat-soluble vitamins (vitamins A, D, E, K) and iron
• Formation of vitamin A; storage of vitamin B complex
• Formation of plasma proteins (albumin, prothrombin, globulins)
• Synthesis of urea, a waste product from protein anabolism
• Storage of glucose as glycogen
• Synthesis of clotting factors (fibrinogen; prothrombin; factors V, VII, IX, X)
• Formation of triglycerides and cholesterol
• Secretion of bile
• Secretion of heparin (anticoagulant)
• Synthesis of immunoglobulins
• Breaking down of fats (lipids)
• Storage of fats and carbohydrates
• Regulation of amino acids
• Production of body heat
• Storage of minerals
Table 26-3 outlines the accessory organs of the digestive system and their selected functions. The main digestive function of the liver is the production of bile. Bile aids in fat digestion and absorption of fat and fat-soluble vitamins from the small intestine. The salts in bile emulsify fat (break fat into small droplets, like a detergent) so that digestive enzymes can act on fat more effectively.
NCLEX Alert The digestive system has many structures and a variety of functions. To correctly respond to an NCLEX situation, you may need to identify correct nursing actions, appropriate medications, or normal laboratory values.
Gallbladder
The gallbladder is a muscular sac 3-4 inches long (7.5-10 cm). It resembles a small pear and is located on the liver’s undersurface. Some authorities regard it as an enlargement of the cystic duct through which it drains. (The prefix relating to the gallbladder is chole-.) The gallbladder’s main functions are to store and release bile as needed in the small intestine for fat emulsification.
Key Concept Removal of the gallbladder (cholecystectomy) is a common surgical procedure. After its removal, other structures, particularly the liver take over its functions.
The system of passageways for the transport of bile from the liver to the gallbladder to the intestine is complex and is known as the biliary apparatus. First, cells within the liver manufacture bile. Small ducts from these cells emerge and join to form the hepatic duct. As bile is produced in the liver, it flows down the hepatic duct and up into the cystic duct to the gallbladder for storage.
As part of digestion in the small intestine, cholecystokinin activates the gallbladder to release bile. Bile flows from the gallbladder through the cystic duct. The cystic duct then joins the hepatic duct to create the common bile duct. The common bile duct, in combination with the pancreatic duct, then empties into the duodenum at the major duodenal papilla (a small distance beyond the pyloric portion of the stomach).
TABLE 26-3. Accessory Organs of the Digestive System and Their Functions
|
ORGAN |
SECRETIONS |
FUNCTIONS |
|
Liver |
Bile |
Emulsifies fats |
|
Stores glucose (as glycogen) |
||
|
Heparin Plasma proteins |
Anticoagulant |
|
|
Albumin |
Provides osmotic pressure for blood pressure |
|
|
Fibrinogen |
Necessary for blood clotting |
|
|
Prothrombin |
Necessary for blood clotting |
|
|
Globulins |
Forms immunoglobulins (antibodies) |
|
|
Other Functions of the Liver |
||
|
Filters blood; removes toxins |
||
|
Breaks down fat and protein |
||
|
Stores protein, fat, carbohydrates, and minerals, including iron |
||
|
Prepares waste (urea); absorbs bilirubin |
||
|
Regulates amino acids |
||
|
Produces body heat |
||
|
Detoxifies poisons |
||
|
Forms vitamin A; stores vitamins A, D, E, K, and B complex |
||
|
Forms triglycerides and cholesterol |
||
|
Gallbladder |
Stores and releases bile |
|
|
Pancreas (exocrine function) |
Bicarbonate ions |
Helps neutralize HCl (hydrochloric acid) |
|
Acinar cells |
Pancreatic juice (pancreatic amylase) |
Digests starch (carbohydrates) |
|
Trypsin |
Digests protein |
|
|
Pancreatic peptase |
Digests fats (triglycerides) |
|
|
Pancreas (endocrine function)— |
Alpha cells—glucagon |
Helps regulate blood glucose levels |
|
(islets of Langerhans) |
Beta cells—insulin |
Helps regulate blood glucose levels |
|
Delta cells—somatostatin |
Helps control release of glucagon and insulin |
Pancreas
The pancreas is a long, fish-shaped glandular organ about 6 inches (15 cm) long located behind the stomach. This organ functions as both an endocrine gland and an exocrine gland. As an endocrine gland, it secretes the hormones insulin, glucagon, and somatostatin into the bloodstream to help regulate blood sugar levels.Its exocrine function is to produce pancreatic juice, which is accomplished by the acinar cells. The acinar cells secrete three main enzymes which assist in digestion of specific nutrients:
• (Pancreatic) amylase: starch
• Trypsin: protein
• (Pancreatic) lipase: fats—lipids (into triglycerides)
Most pancreatic enzymes are produced in inactive forms and are activated in the small intestine. (The inactive forms help to minimize the risk of pancreatic self-digestion.) In addition to the wide variety of digestive enzymes found in pancreatic juice, bicarbonate and water are also present. Bicarbonate ions (HCO3) are secreted from small ductules in the pancreas. As stated previously, HCO3~ combines with hydrogen ions to neutralize the hydrochloric acid in chyme. (Enzymes work best in a solution with a pH between 5 and 8.) Pancreatic juice enters the duodenum through the pancreatic duct. Pancreatic juice is potent and necessary for life. Adequate digestion cannot occur without it.
Peritoneum
The peritoneum is a large sheet of serous membrane that covers and protects many abdominal organs. It also secretes a thin fluid (peritoneal fluid) that provides lubrication between its visceral (next to organs) and parietal (next to the abdominal wall) layers. Folds of the peritoneum that provide support and protection to the intestines are called mesenteries. The mesenteries are sheets of connective tissue; some have names (e.g., the greater and lesser omentum). Some body structures, such as the kidneys, lie behind the peritoneum and are said to be retroperitoneal. (This allows kidney surgery to be performed from the back, eliminating the need to enter the abdomen.)
System Physiology
PROCESSES OF DIGESTION
For nutrients to reach individual cells, food first must be broken down into small compounds. After food is broken down, absorption can occur.The body performs two types of digestion: mechanical and chemical. Table 26-4 summarizes the digestive process.
• Mechanical digestion is the physical breakdown of food caused by chewing and the movement of food in the digestive tract. Breaking food into smaller pieces exposes more of food’s surface area to the effects of enzymes, acids, and other chemicals.
• Chemical digestion is the breakdown of the chemical bonds in food with the addition of enzymes, acids, and water. Therefore, some digestive processes begin in the mouth, pharynx, and stomach, but most digestion occurs in the duodenum.
TABLE 26-4. Human Digestive Process
|
Chewing of food |
5-10 seconds |
|
Swallowing |
10-15 seconds |
|
Food mixing in stomach |
3-5 hours |
|
Movement through small intestine |
3-4 hours |
|
Movement through large intestine |
18-48 hours |
Enzymes
As described previously, enzymes are the driving force behind chemical digestion. They are secreted by the salivary glands, stomach, small and large intestines, liver, and pancreas. Enzymes often derive their names from the substances on which they act. Each enzyme is effective only on a specific nutrient (see Table 26-2).
Mucus and Water
The GI tract uses other fluids to lubricate, liquefy, and digest food. Mucus, formulated by the mucous membrane lining of the GI tract, lubricates food and protects the GI tract’s lining from mechanical or chemical injury (from stomach acids). Water liquefies food, making it easier to digest and absorb. Water participates in chemical reactions and is also the solvent that follows electrolytes (osmosis) across the intestinal wall in either direction.
Digestion in the Stomach
The fundus and body of the stomach act mostly as storage areas; the pylorus is the area that is primarily responsible for stomach digestion. Both mechanical and chemical digestion occur in the stomach. Saliva from the oral cavity continues starch digestion in the stomach, but carbohydrates are not fully digested there. Fat digestion continues in the stomach owing to lingual lipase, but only a very small amount is broken down in the stomach. Pepsin begins protein digestion in the stomach, but it is not completed there either.
The stomach is lined with mucous membrane; its mucus coats and protects the stomach lining. The stomach lining also contains secretory cells called chief cells and parietal cells.
• Chief cells secrete pepsinogen and gastric lipase. Pepsinogen is a precursor of pepsin, the enzyme needed to break down proteins. Gastric lipase breaks down triglycerides in butterfat (found in milk and some other dairy products).
• Parietal cells secrete hydrochloric acid, the functions of which are to activate pepsinogen and to kill most microorganisms in the stomach. When activated by hydrochloric acid, pepsinogen changes into the enzyme pepsin, which begins to break down proteins. Another secretion of the parietal cells is intrinsic factor, which is essential for life. This substance is necessary for absorption of vitamin B12, required for the development of red blood cells in bone marrow.
Key Concept Intrinsic factor produced by the parietal cells in the gastric mucosa is required for absorption of vitamin B|2. A deficiency of vitamin B|2 will result in pernicious anemia.
The stomach also produces regulatory hormones, such as gastrin. Gastrin stimulates the secretion of hydrochloric acid and pepsinogen. It also weakly stimulates the pancreas to secrete enzymes and the gallbladder to release some bile.
Digestion in the Small Intestine
As stated previously, most digestion takes place in the small intestine. Here, cholecystokinin (CCK), a hormone, is secreted by the duodenum and jejunum in response to the presence of fat in the duodenum. CCK activates the gallbladder to release bile. Bile flows through the cystic duct into the common bile duct and is deposited in the duodenum. There, the action of bile breaks fat droplets into smaller particles. Bile also helps neutralize the acidic chyme and facilitates excretion of waste products, including bilin and bile acids.
Cholecystokinin also stimulates the pancreas to secrete pancreatic juice, which is then changed into an active form in the small intestine. Specific enzymes (amylase, trypsin, and lipase) in the pancreatic juice digest starch, protein, and triglycerides (fats), respectively. CCK also assists in the inhibition of digestive processes in the stomach.
Key Concept The balance of acidity and alkalinity is vital.The pH in the upper respiratory tract is weakly acidic, allowing carbohydrates to begin to break down. Most digestive enzymes cannot function in the stomach, because it is too acidic, thus, carbohydrate digestion is inhibited there. However the low pH (acid) in the stomach begins protein breakdown. In the small intestine, the pH rises (becomes more basic/alkaline) owing to the addition of bicarbonates. Enzymes can now function and carbohydrate digestion resumes, along with breakdown of fats and protein.
Sucrase, maltase, and lactase—enzymes secreted by the intestinal mucosa—assist in digestion of carbohydrates (CHO). Several protein enzymes called peptidases also assist in the digestion of proteins. When digestion is completed, the simplest form of these nutrients remains. These are amino acids (proteins), fatty acids (lipids), and monosaccharides—simple sugars (glucose, galactose, and fructose). These substances can now be transferred into the blood stream for use by the body. Table 26-2 summarizes the actions of enzymes, hormones, and other substances in digestion.
Key Concept Digestion is accomplished by:
• Physical breakdown (mastication)
• Churning
• Diluting
• Chemical breakdown
• Dissolving
To be absorbed, foods must be broken into their simplest form:
• Carbohydrate to monosaccharide (simple sugar): glucose, galactose, fructose
• Protein to amino acid (and some dipeptides)
• Fat to fatty acid and glycerol
NCLEX Alert The digestive system’s physiology is important. Concepts such as liver disease, nutrition, ulcer formation, or malignancies can be seen. The NCLEX commonly provides scenarios that integrate the body’s normal anatomical functions with abnormal situations.