Learning Objectives
1. List examples of sterile and nonsterile body areas.
2. Differentiate between medical and surgical asepsis.
3. Differentiate between disinfection and sterilization.
4. List guidelines to follow when using sterile technique.
5. Demonstrate the proper technique for opening a sterile tray and a sterile package.
6. Demonstrate the correct method for handling sterile supplies or pouring solutions when working with a sterile field.
7. Describe the procedures for female and male catheterization, demonstrating each on a laboratory model. Identify what information must be documented following catheter insertion.
8. Explain the procedure for removal of a retention catheter.
|
IMPORTANT TERMINOLOGY |
|
|
autoclave disinfection |
sterile technique |
|
clean medical asepsis |
sterilization |
|
contaminated sterile |
surgical asepsis |
|
dirty |
|
Keeping the client and the environment clean is necessary to maintain comfort and well-being, as well as to reduce the risk of infection transmission. In addition, in specific circumstances, keeping aspects of the environment sterile is critical to ensure that the client does not develop an infection. This topic explains the differences between medical asepsis (clean technique) and surgical asepsis (sterile technique). This topic also discusses steps in surgical asepsis and how to perform selected procedures in which surgical asepsis (sterile technique) is necessary.
ASEPSIS
To limit the transfer of microorganisms effectively, the nurse must understand the differences between commonly used terms as they apply to medical asepsis. Dirty is a term for any object that has not been cleaned or sterilized to remove microorganisms. A contaminated object is any object that is not sterile. This includes items that are dirty, as well as those that are considered to be only clean. An object that is grossly contaminated contains visible body fluids, discharges, or dirt. (All body fluids are considered to be grossly contaminated.)
The term clean implies that many of the most harmful microorganisms have been removed. Mechanical cleansing of inanimate objects, such as tops of medication vials, counters, or blood drawing chairs, is done with a special soap or antiseptic cleanser. Careful handwashing, including careful cleaning of fingernails, is also part of this process. Both mechanical cleansing of inanimate objects and handwashing are sufficient to provide medical asepsis; the skin or countertop is now considered to be clean. Sterile means that the item or area is free of all microorganisms and spores. A spore is a resting stage of some microorganisms and is resistant to environmental changes.
Key Concept If a sterile item touches a non-sterile item, the sterile item becomes contaminated.
Many body parts are clean but not sterile. Examples include the skin, mouth, gastrointestinal tract, and upper respiratory tract. These areas are open to the outside and are inhabited by microorganisms at all times. Other body parts are considered to be sterile. Either they do not normally open to the outside (e.g., the abdominal cavity or the ovary) or they do not normally contain any microorganisms. Some areas (e.g., the urinary bladder) are susceptible to infection. The bladder is normally considered to be sterile, even though it is open to the outside.
DISINFECTION AND STERILIZATION
Disinfection
Disinfection is a process that results in the destruction of most pathogens, but not necessarily their spores. Common methods of disinfection include the use of alcohol wipes, a hexachlorophene (pHisoHex, Septisol) or chlorhexidine gluconate (Hibiclens) soap scrub, or a povidone-iodine (Betadine) scrub, to kill microorganisms on the skin. A surgical hand scrub takes longer than regular handwashing and is considered to be a disinfection process. The skin is considered to be disinfected, rather than just clean.
Stronger disinfectants include phenol and chlorine bleach, which are generally too strong to be used on living tissue. They are used on surfaces, such as floors and countertops. Boiling also can be used to disinfect inanimate objects; however, it does not destroy all organisms and does not destroy spores.
Key Concept It is possible to disinfect the skin; it is not possible to sterilize the skin.
Sterilization
Sterilization is the process of exposing articles to steam heat under pressure or to chemical disinfectants long enough to kill all microorganisms and spores. After a client leaves a healthcare facility, equipment he or she used is either sterilized or discarded. For example, at discharge a client usually takes home items such as washbasins, mouth care utensils, and incentive spirometers; if he or she does not take them, these items are discarded. Occasionally, large or very expensive medical equipment is sterilized for reuse. This includes machines such as the dialysis or heart-lung machine and nondisposable surgical equipment, such as forceps, hemo-stats, and special scissors.
As stated, sterilization destroys all organisms and spores. Exposure to steam at 18 pounds of pressure at a temperature of 125°C (257°F) for 15 minutes will kill even the toughest organisms and spores. The pressure steam sterilizer is called an autoclave.
Some chemicals also can be used to sterilize an object. However, chemical disinfectants powerful enough to destroy spores and all pathogens or extreme temperatures cannot be used on certain articles, such as plastic. Thus, most plastic items are disposable. In addition, moist heat such as that found in an autoclave dulls the sharp cutting edges of some instruments; therefore, if the items are not disposable, dry heat or chemicals are used to sterilize them. (Today, most sharps—such as scalpels and suture removal scissors—are disposable.) Needles used for injections or acupuncture are always discarded after one use. Other methods of sterilization include radiation and gas sterilization with ethylene oxide.
MEDICAL AND SURGICAL ASEPSIS
Medical asepsis is clean technique. Surgical asepsis is sterile technique.
NCLEX Alert It will be important for you to know and understand the definitions of and differences between surgical asepsis and medical asepsis, and disinfection and sterilization, as they relate to the prevention of infection and complications.
Medical Asepsis or Clean Technique
The purpose of maintaining medical asepsis is to prevent the spread of disease from one person to another, whether it is from client to nurse, client to client, nurse to client, or from a person to the environment. This is medical asepsis in action.
Surgical Asepsis or Sterile Technique
To maintain sterility, surgical asepsis or sterile technique is used. Surgical asepsis differs from medical asepsis in that surgical asepsis uses sterile technique. Use of effective sterile technique means that no organisms are carried to the client. All microorganisms and spores are destroyed before they can enter the body. The remainder of this topic explains sterile technique and selected applications.
In some cases, sterile and clean techniques are combined. For example, for many dressing changes or for procedures such as tracheostomy care or emptying a catheter drainage bag, sterile materials are used, but clean gloves are worn. This means that clean technique (medical asepsis) is performed, using sterile supplies.
In other cases, sterile technique is used throughout the entire procedure. Sterile technique (surgical asepsis) is used when administering parenteral (outside the digestive tract) medications and performing surgical and other procedures, such as urinary catheterization. With surgical asepsis, first articles are sterilized, and then their contact with any nonsterile articles is prevented. When a sterile article touches a nonsterile article, the sterile article becomes contaminated—it is no longer sterile.
Key Concept Sterile to sterile remains sterile. Sterile to clean, dirty, or contaminated becomes contaminated. Always think before you touch anything.
STERILE TECHNIQUE (SURGICAL ASEPSIS)
Reasons for Sterile Technique
To prevent the spread of infection, the supplies used for surgical and other sterile procedures must be free of all microorganisms. Anything that either touches an open wound or skin break, enters a sterile body cavity, or punctures the skin must be sterile, to prevent introducing microorganisms.
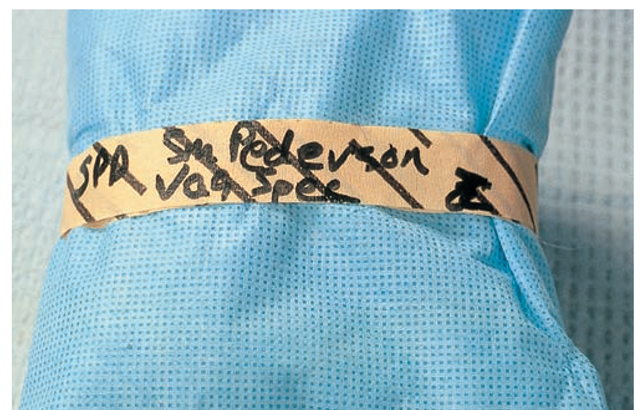
FIGURE 57-1 · Some items, such as surgical towels, nondisposable instruments, and surgical linens, are packaged, secured with special masking tape, labeled, and sterilized. The tape changes color or shows black stripes when the items are sterilized. The facility specifies the length of time the item will still be considered sterile. When that period of time has elapsed, the item must be resterilized.
Many healthcare facilities prepare sterile supplies in a central supply room (CSR), also called central sterile supply (CSS), or purchase them in a sterile package and dispose of them after use. Some items, such as surgical towels or drapes, are packaged, secured with special masking tape, labeled, and sterilized (Fig. 57-1). Items such as syringes and needles are packaged individually by the manufacturer, and are sterilized before distribution; these are discarded after one use.
Key Concept Disinfection is the destruction of most pathogens, but not spores. Sterilization is the destruction of all microorganisms and spores.
Every step in an aseptic procedure is a link in a chain. If one link is broken by contaminating anything, the entire chain has been broken, and infection can occur.
Key Concept Never touch sterile articles with nonsterile articles. Discard an article if it becomes contaminated or if you are unsure whether or not it is contaminated.
Do not risk using a contaminated instrument or needle.
Learning to perform sterile technique correctly to maintain sterility requires understanding the meanings of dirty, contaminated, clean, and sterile. Maintaining sterile technique also requires a great deal of practice. Equipment or supplies used for many nursing interventions are packaged to maintain sterility. In Practice: Nursing Care Guidelines 57-1 provides general tips for using sterile technique. In Practice: Nursing Procedure 57-1 describes the steps associated with opening a sterile package; these techniques are basic to many sterile procedures. Also refer to Figure 58-7, which illustrates the method for a clean nurse to hand sterile supplies to a nurse wearing sterile gloves and performing a sterile procedure.
IN PRACTICE NURSING CARE GUIDELINES 57-1
STERILE TECHNIQUE
• After sterile gloves or gown have been put on, the nurse cannot touch anything that is not sterile.
• Reaching over a sterile field contaminates the sterile area, unless sterile clothing and gloves are worn.
• If a sterile wrapper becomes wet, the wrapper and its contents are no longer sterile.
• If a mask becomes wet, it no longer screens out microorganisms; the mask must be changed for a new mask.
• When wearing sterile gloves to perform a sterile procedure, keep them in front, between the nipple line and waist. If gloves move above or below these areas, they are considered contaminated.
• A person’s back is not sterile, even if a sterile gown is being worn.
• Objects are considered contaminated if there is any uncertainty whether contamination has occurred. When in doubt, consider the objects in question to be contaminated.
• Skin cannot be rendered sterile; it can only be made clean.
• Parts of the body that are not normally exposed to the outside are considered sterile. These parts include the abdominal cavity the urinary bladder and usually the uterus.
Healthcare providers entering sterile environments, such as an operating room (OR), must wear sterile protective clothing to prevent contaminating the area with microorganisms that reside on the skin, hair, and clothing. Because many clients today are sent home from the hospital with catheters, intravenous (IVs) lines, and other tubes in place, it is vital to teach the client and family how to lessen the possibility of infection at home. Typically, the client and family are taught how to manage specific equipment at home; this equipment is kept sterile if possible. However, because the client will be exposed to microorganisms within his or her own home, clean technique may be used for some procedures that would require sterile technique in the healthcare facility. In these cases, the equipment is considered contaminated specifically to that person. In Practice: Educating the Client 57-1 highlights some examples and tips for teaching how to prevent spreading infection in the home.
IN PRACTICE EDUCATING THE CLIENT 57-1
PREVENTING THE SPREAD OF INFECTION AT HOME
Examples of Client and Family Teaching
• Emptying the catheter drainage bag
• Safely changing catheter tubing
• Hanging a new IV bag
• Giving an injection at home
Additional Tips for Teaching
• Demonstrate the skill to be performed.
• Ask the client and family to demonstrate the skill before discharge.
• Explain how to recognize problems or complications, such as postoperative infections.
• Describe when to seek medical care immediately
• If indicated, make a referral for home care nursing follow-up.
Hair Covering
In sterile environments (especially the OR) workers must completely cover their hair. If the hair is long, a hood is worn to cover the hair. If the hair is short, a surgical cap is used. The nurse who has a moustache or beard wears a full-face surgical hood to cover the entire face, except the eyes.