Prediction of Pressure Ulcer Risk
All clients must be evaluated for the risk of developing pressure ulcers or skin breakdown on admission and regularly thereafter, according to the facility protocol. Clients in the Intensive Care Unit (ICU) and Pediatric clients usually have more frequent skin examinations. Several methods are used to predict the possibility of pressure ulcer development. Two of these are the Braden Scale (see Figure 58-5) and the Norton Scale. If a client is found to be at high risk, measures must be taken to prevent the development of pressure ulcers before they occur.
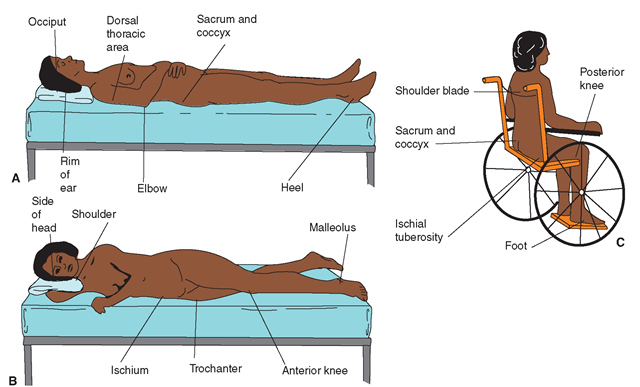
FIGURE 58-4 · Common sites for pressure ulcers. (A) Supine position. (B) Side-lying position. (C) Sitting. Included also are sites of tube insertion (e.g., IV, NG tube, catheter, drains)
Nursing Alert If a client is admitted to a facility with an existing wound or pressure area, this must be carefully documented as "present on admission." If this is not documented, the facility would become liable for this and any additional skin breakdown. In addition, if a wound exists, plans can be made to begin immediate treatment.
A "facility acquired" pressure area or ulcer is considered to be a sentinel event and must be reported to the appropriate authorities. If a stage III, IV or nonstageable ulcer develops within a facility, this usually must be reported to the Health Department and investigated.
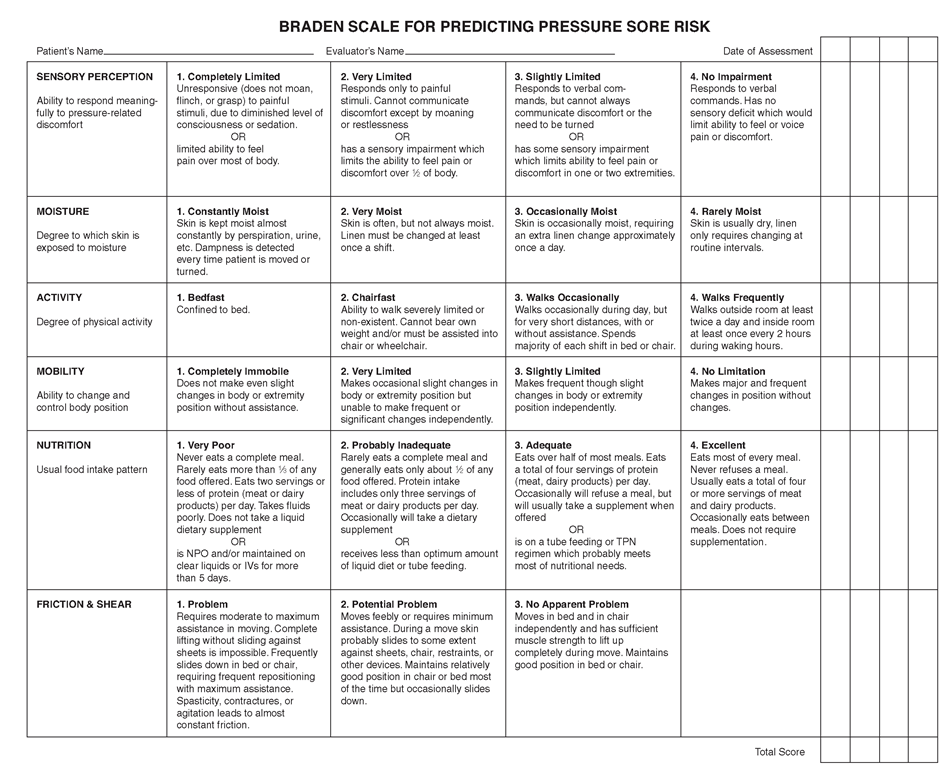
The Braden Scale. One of the evaluative scales used to predict a client’s risk of developing pressure areas is the Braden Scale (Fig. 58-5). This rating scale considers the two “primary etiologic factors of pressure ulcer development— intensity and duration of pressure . . . and tissue tolerance of pressure” (Braden, 2004, p. 240). The following factors are considered: sensory perception, moisture level, activity, mobility, nutrition, and friction/shear. The use of such a scale allows healthcare personnel to take steps to prevent the development of skin breakdown in clients at risk. (The lower the score, the greater the risk.) Table 58-2 identifies some factors in management of clients at risk for skin/tissue breakdown. All clients should have a risk evaluation on admission and regularly during their stay in the facility.
Classification of Pressure Ulcers
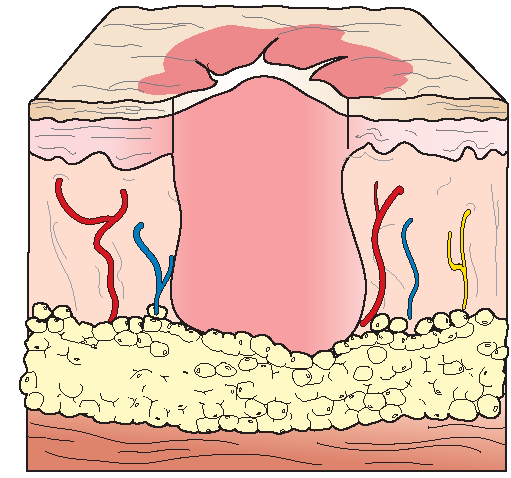
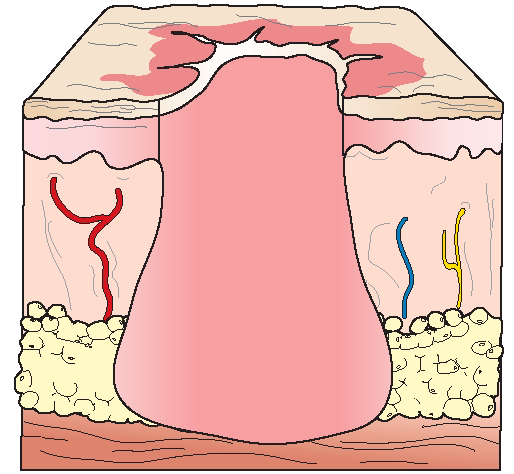
Pressure ulcers are classified according to four stages of development (Box 58-1 and Fig. 58-3). In the fourth stage, a thick, leathery black crust of necrotic (dead) tissue, called eschar, often develops around the edges (see Fig. 47-17 and Fig. 58-3C). Eschar that separates from living tissue is called slough and is often tan or yellow. Debridement (removal of dead or infected tissues) allows healthy tissue to grow, progressing from internal tissue outward. Box 58-2 lists other types of wounds that are treated in a manner similar to that used for pressure ulcers.
Key Concept Deep open wounds must granulate in (heal) from the inside outward. If the outside becomes sealed before the area underneath has healed, an abscess often forms. This abscess may be sterile or infected (containing pathogens). In any event, an abscess is painful and dangerous and must be treated. Reporting of granulation tissue is a part of pressure ulcer documentation.
Two national sources of information regarding wound prevention, and pressure ulcer staging, prevention, and treatment are the National Pressure Ulcer Advisory Panel (NPUAP) and the Wound, Ostomy and Continence Nurses Society (WOCN).
Nursing Alert If a client with a pressure ulcer or any other wound is to be sent to the operating room, x-ray or any therapy notify that department, so appropriate measures can be taken to protect the wound and prevent spreading of infection.
FIGURE 58-5 • Braden Assessment Scale for Predicting Pressure Ulcer Risk Total possible points – 23. The lower the score, the greater the riskThe client is identified as at risk for pressure ulcer development if the score is less than I 6. (Some facilities use scores from 15 to I 8 as the risk prediction score.) A modified scale (Braden Q) is available for use with pediatric clients.The Braden Q also considers tissue perfusion and oxygenation; the risk cut-off score for pediatric clients is usually 23.
TABLE 58-2. Preventive Measures for Common Causes of Wounds
|
CAUSES OF WOUNDS |
LOCATION |
PREVENTION* |
|
Pressure External force sufficient to occlude blood in capillaries resulting in tissue anoxia (lack of oxygen) and tissue death (necrosis) |
Especially bony prominences |
Establish a turning schedule at least every 2 hours. Use supportive measures to relieve pressure (see Box 58-3). Keep pressure off bony prominences and other vulnerable areas, by elevating them with pillows and by using padding and special beds. Have a minimum of linens under the client. Avoid donut devices. Assist the client to be out of bed and/or walking as soon as possible. |
|
Shear Interaction of gravity and friction against the skin’s surface |
Surfaces exposed to bed or chair; especially if skin turgor is poor; coccyx most common site |
Use draw sheet and lifting/turning sheet. Use logroll turns. Avoid dragging client’s body over sheets. Limit elevation of head of bed to 30 degrees. Position feet against footboard before head elevation. Request assistance when necessary |
|
Friction Superficial abrasion resulting from the skin rubbing another surface |
Surfaces that rub on bed or chair surfaces or against each other Sites of tube insertion, IV NG tube, drains, and so forth. |
Apply transparent dressings to areas of friction (to prevent rubbing and to facilitate observation without dressing removal). Move client carefully. Use trapeze, client lift, and so forth. Use heel or elbow protectors, or elevate heels off bed. Keep skin adequately hydrated. Use lotion and special skin barrier products. Use friction-reducing sheets for turning and positioning. Use a bridge (transfer board) to move clients (be sure linens are between client’s skin and the bridge). Use a client lift, when needed. |
|
Stripping Unintentional removal of epidermis by mechanical means, such as with tape removal |
Surfaces where applied |
Use only porous tapes and apply without tension, if possible. Use saline to help remove dressings that adhere to the skin. Remove tape by slowly pulling tape away with one hand, while supporting surrounding skin with the other Use alternatives to tape, such as Montgomery straps or Kerlix to wrap a limb, or use a stockinette. Use tube-gauze dressing, rather than tape. |
|
Urine or Stool Urinary and fecal incontinence |
Perianal skin |
Use containment equipment: absorptive products, condom catheters, or fecal pouches. Keep perianal skin cleansed, moisturized, and protected with barrier ointments. Investigate cause (e.g., urinary infection, incontinence, need for toileting schedule, impaction, diarrhea, constipation, organisms in stool, tube-feeding intolerance, lactose intolerance, reactions to medications). Offer bedpan/urinal and fluids each time client is turned. |
|
Perspiration |
Areas where moisture can get trapped and air cannot circulate (e.g., skin folds) |
Keep areas of skin folds dry Use barrier ointments, as prescribed. Use antifungal powder or other prescribed medication, if yeast infection is present. (Creams are often contraindicated.) |
|
Arterial Insufficiency Arterial perfusion jeopardized |
Feet, toes, and lower leg; edematous areas |
Avoid compression. Protect from mechanical, chemical, or thermal injuries. Provide adequate remoisturizing. Take special care with diabetic clients, paralyzed persons, or persons with a bleeding disorder Elevate edematous feet and legs. |
|
Maceration |
Under pendulous breasts or folds of abdomen |
Wash thoroughly at least once per day. Expose to air, if possible. Apply powder or prescribed medicinal cream. Encourage female client to wear a bra when up, if possible. |
*Special note: Some of these measures require a specific order by the primary healthcare provider: Check the protocols of your agency. A risk evaluation should be performed on each client and measures taken to prevent skin breakdown in all clients, particularly those most vulnerable.
IV intravenous; NG, nasogastric.
BOX 58-1.
Stages of Pressure Ulcer Classification (see also Fig. 58-3.)
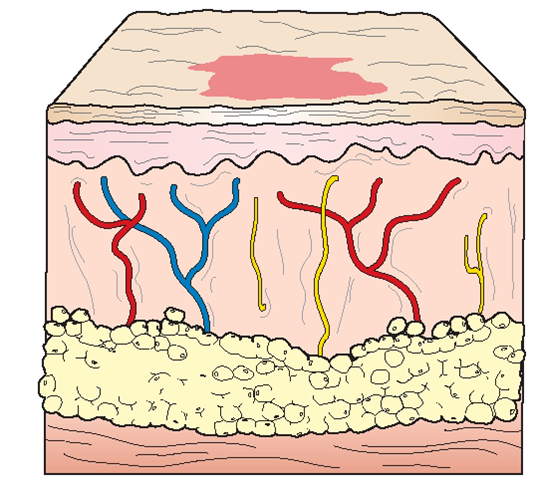
Stage 1 (I): Pressure-related alteration of intact skin, as compared with adjacent/opposite body area. May include changes in (one or more): skin temperature (warmth/coolness), tissue consistency (firm/boggy/mushy), or sensation (pain/itching). Ulcer appears as a defined area of persistent redness in lightly pigmented skin; in darker skin, ulcer may appear as persistent red, blue, or purple hue. (The color does not blanch or lighten when pressed.) Reversible, if pressure is relieved (by frequent turning, positioning, and pressure-relieving devices).
Stage 1
Stage 2 (II): Loss of epidermis with damage into dermis (partial-thickness tissue loss); appears as shallow crater/ blister with red/pink wound bed with no sloughing. May also appear as an intact or ruptured serum-filled blister or abrasion. Swollen and painful; several weeks needed to heal after pressure relieved (by maintenance of a moist environment—saline irrigation or special occlusive dressing).
Stage 2
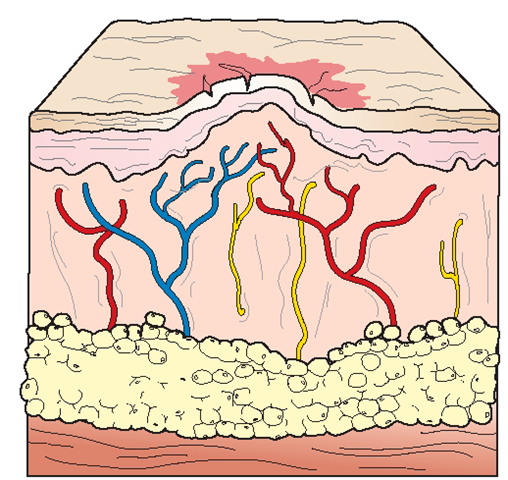
Stage 3 (III): Subcutaneous tissues involved (full-thickness tissue loss); subcutaneous fat may be visible (no bone, tendon, or muscle exposed). May show undermining or tunneling. Not painful; possible foul-smelling drainage; months may be needed to heal after pressure relieved (by debriding with wet-to-dry dressings, surgery or proteolytic enzymes).
Stage 3
Stage 4 (IV): Extensive damage to underlying structures; fullthickness tissue loss, with exposed bones, tendons, or muscles. (Wound possibly appearing small on surface, but with extensive tunneling underneath.) Slough or eschar may be present. Usually foul-smelling discharge; months or years may be needed for healing (often requires skin grafting).
Stage 4
Non-stageable: The base of a full-thickness ulcer; covered by slough and/or eschar.
Deep-Tissue Injury: Purple or maroon intact skin, or blood-filled blister
Key Concept A shallow wound on an area such as the nose, ear; occiput, or malleolus may be stage III or IV even though it is not deep.
As a pressure ulcer heals, the stages do not reverse. (For example, a stage IV ulcer cannot become a stage III ulcer.) This ulcer could be referred to as a "healing or healed stage IV ulcer” Do not confuse a pressure ulcer with skin damage caused by incontinence or friction/shear .