COMMON SURGICAL TREATMENTS
Plastic Surgery
Although skin disorders make clients physically uncomfortable, disfigurement is one of the most damaging psychological effects. Plastic surgery is one way to improve or correct disfigurement. It may be performed for cosmetic effects, to repair congenital defects, or to repair the results of trauma. Plastic surgery is also called reconstructive surgery.
Skin and Tissue Grafts
Skin grafts are used to cover areas of skin lost through wounds, burns, or infections. A graft is a transplant of skin that is placed on clean, viable tissue. Grafting is a painstaking procedure that may be done in stages. Grafting may take many months, depending on the size and number of areas to be covered and the success of each step.
There are two major types of grafts. One type is called a free graft, which means that skin has been completely removed from its original site and grafted onto the recipient site. The other type is pedicle graft. In this type of graft, one end of the graft remains attached to the donor site so that it can continue to receive nourishment until new circulation is established. The other end is attached to the recipient site on the same client’s body. In some situations, the client must assume an unnatural position until the graft begins to grow in the new site, at which time the graft can be separated from the donor site. A pedicle graft is used when a large area of skin is to be replaced, such as on an ear, part of a hand or foot, or a large part of the face.
Other types of grafts are named in relation to the donor and are described in more detail in the section of this topic on burns.
Nursing Considerations
Before reconstructive or graft surgery, prepare the client by explaining what he or she can expect. Postoperatively, the surgical site may be swollen and bruised. Pay scrupulous attention to aseptic technique, protect the grafts, keep new grafts immobilized, and prevent infection at donor sites.
Emotional support is an important part of nursing care in reconstructive surgery. The client is often self-conscious about his or her appearance and may avoid others. Encourage family and friends to visit. Provide the client with emotional support and reassurance.
NURSING PROCESS
DATA COLLECTION
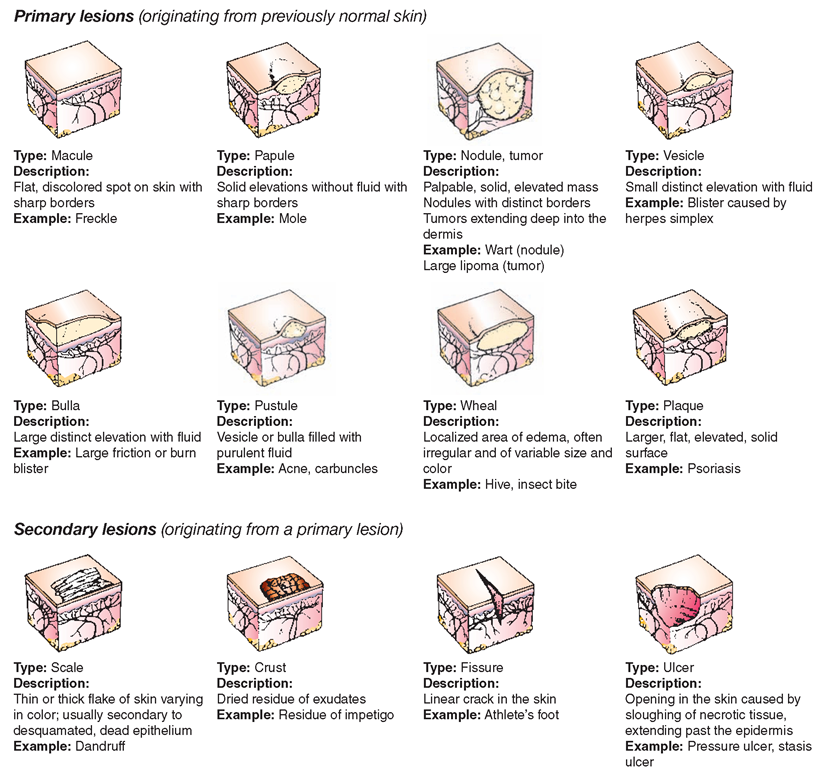
Carefully observe and document the skin condition of all clients. Establish a baseline for future comparison and report any changes that occur. Compare skin color with the client’s usual color, texture, and turgor. Note whether the skin is intact; examine for any lesions or pressure ulcers. Carefully document the size, color, texture, location, pattern of disruption, or any other distinctive characteristics of the lesion. Figure 75-1 highlights several types of common skin lesions. Always use correct terminology to describe variations from normal skin appearance (see Box 75-1). In addition, ask the client about subjective symptoms, such as itching (pruritus).
FIGURE 75-1 · Common skin lesions.
NCLEX Alert As a major component of nursing care, observation of the skin is a normal clinical task. Therefore, on an NCLEX examination, expect to answer questions relating to your observations and the priority for interventions needed for these observations.
Special Considerations: CULTURE & ETHNICITY
Variations in Skin Appearance
All color types of skin can become sunburned. Be aware of normal biocultural variations in the skin’s appearance. If possible, ask the client or family to describe any variations from normal skin appearance.
Fluid and Electrolyte Balance
Data collection should include an understanding of the client’s fluid and electrolyte status. A client’s fluid and electrolyte balance and general nutrition may be difficult to maintain because of developing exudates or serum loss stemming from inflammation or burns. Encourage the client to drink and eat. Provide a high-calorie, high-protein diet. Carefully document the client’s intake and output (I&O). Initiate a calorie count for clients who are at risk for poor nutrition. Individuals who have large surface area grafts or deep burn injuries usually require electrolyte replacement.
Allergies
As part of data collection, ask the client if he or she has known food or drug allergies. Food allergies may cause or aggravate skin disorders. Clients may also be sensitive to products such as tape, iodine, latex, or fragrances. Clients may know their allergies, or skin tests may determine them. Use more than one approach with the client when discussing allergies. For example, the client may deny being allergic to all antibiotics. Instead, ask the client specific questions such as, “Have you ever had an unexpected reaction to penicillin, shellfish, peanuts, or other foods or medicines?” Protect the client from exposure to known allergens.
Emotional Support for Clients with Skin Disorders
During data collection, determine your client’s support system and coping mechanisms. A relationship may exist between emotional difficulties and skin problems—an underlying psychological problem may manifest itself in some type of skin eruption. Furthermore, the itching that accompanies many skin disorders gives rise to emotional distress; pruritus is often more irritating and difficult to control than pain.
Observe the client’s emotional response to the skin disorder or disease by answering the following questions. Is the client so disabled by pain or itching that he or she needs assistance or encouragement to meet daily needs? Is the disorder so disfiguring that it affects social activities or selfesteem? Is the client anxious or fearful of the outcome? Is the situation life threatening?
PLANNING AND IMPLEMENTATION
Involve the client when planning effective care (based on the nursing diagnoses) to meet his or her needs. Provide preoperative and postoperative care for the client undergoing plastic surgery or skin grafting. For the client with severe burns, assist in debridement of dead tissue or in life-sustaining treatments. The client with a skin disorder also may require assistance in meeting daily self-care needs, dealing with itching or pain, or working through the emotional aspects of a disfiguring or chronic disorder. Teach the client about the disorder and its necessary treatments. Develop a nursing care plan to meet each individual’s needs.
Planning and implementing care includes relieving pruritus, providing therapeutic baths, and applying dressings. Basic nursing care, such as turning the client, assisting with hygiene, and observing and preventing pressure ulcers, also is essential.
Chronic skin problems can present emotional challenges. Often, the same disorder flares up at intervals throughout the client’s life. He or she may require assistance to cope. Group therapy may be helpful.
As a result of the skin disorder, the client may feel that his or her outward appearance is unattractive. Foster an atmosphere of acceptance and support. Allow the client to express his or her feelings and provide companionship.
The use of touch can be therapeutic. The nurse may touch the client who has a skin condition with clean, ungloved hands, unless the client is contagious or has open or draining lesions. Touch can be equally effective with gloved hands.
EVALUATION
Routinely evaluate outcomes of care. Include the client, family, and all members of the healthcare team. Have you met short-term goals? Are long-term goals still realistic? What rehabilitation, home care, or other community services (if any) does the client need, especially if the skin disorder is chronic or requires continued treatment? In planning for further care, consider the client’s prognosis, complications, and responses.
ACUTE AND CHRONIC SKIN CONDITIONS
Urticaria
Urticaria, commonly called hives, is characterized by the sudden appearance of edematous, raised pink areas called wheals that itch and burn. Hives may disappear quickly or they may remain for several days. In most instances, acute urticaria is a manifestation of an allergic reaction to medications, foods, spores, or pollens.
Contact allergens, such as face powder, can cause contact dermatitis. The most common contact allergens are soaps, nickel-based jewelry, perfumes, dyes, and plants (e.g., poison ivy), chemicals, rubber, and insecticides. Stress and anxiety are thought to be important aggravating factors.
Urticaria that lasts more than 6 weeks is called chronic urticaria. Its exact cause remains unknown in the vast majority of people. Examine the client with an unexplained rash for the possibility of Lyme disease.
Edema associated with urticaria is only a temporary annoyance, unless it involves extensive vital areas. However, angioedema (swelling) can be a life-threatening condition that is similar to urticaria, but involves deeper dermal and subcutaneous tissues. Angioedema commonly affects the lips, eyelids, skin, gastrointestinal tract, hands, feet, genitalia, tongue, and larynx. If the larynx becomes edematous, the client may develop severe respiratory distress due to airway obstruction.
The best treatment for urticaria is identification and removal of its cause. Treat mild reactions with cold compresses or tepid colloidal-oatmeal or baking-soda baths. Antipruritic lotions, such as calamine, may help. Nonsedating antihistamines, such as fexofenadine HCl (Allegra), are often used for chronic urticaria. In severe cases, epinephrine may be administered.
Nursing Alert Angioedema associated with urticaria can become life threatening. Observe closely and report any of the following findings immediately because medications and emergency interventions may be necessary.
• Extreme swelling of the lips
• Swelling around the eyes
• Dyspnea (difficult breathing)
Vitiligo
Vitiligo occurs when areas of the skin are completely lacking in pigmentation. Pigment cells (melanocytes) cannot be detected in the depigmented areas, resulting in patches or areas of very pale, white-looking skin. The cause of vitiligo is unknown. No effective remedy is known. Surgical treatments include mini-grafting and melanocyte transplantation. The treatment is prolonged and time-consuming and must take place under a physician’s supervision. Cosmetics designed to cover birthmarks may be used to mask vitiligo. Areas of skin that are not pigmented are more susceptible to sunburn and skin cancers, thus it is important for patients with vitiligo to use a high sun protective factor (SPF) sunscreens and to monitor closely for any skin changes that appear cancerous.
Special Considerations: CULTURE & ETHNICITY
Detecting Pigment Changes
Vitiligo is more obvious in darker-skinned individuals.
Eczema
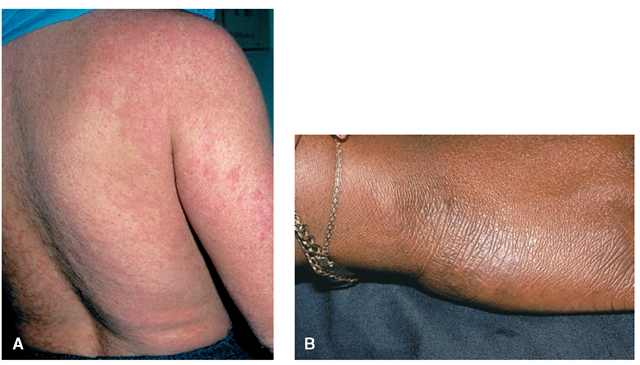
Eczema, also known as atopic dermatitis, is a form of dermatitis (Fig. 75-2). This condition causes small vesicles to appear, as well as reddened and pruritic skin. Sometimes, the vesicles burst and ooze, forming crusts. Persistent irritation and scratching make the skin appear leathery and thick. Affected individuals may develop viral, bacterial, or fungal skin infections. Eczema may spread to other areas, but is commonly found in the folds of the elbows, the backs of the knees, and on the face, neck, wrists, hands, and feet. It may disappear completely for months or sometimes years but can recur at any time.
Although the exact cause is unknown, eczema is known to be associated with heredity, allergy, and emotional stress. There may also be an autoimmune component. Sometimes, a family history indicates an allergy, such as hay fever or asthma. Children who have eczema often develop these conditions later.As a client grows older, emotional factors can aggravate eczema.
The goal of treatment is to prevent skin dryness, cracking, and itching. Treatment consists of applying moisturizing creams, corticosteroid ointments, tar solutions, or wet dressings to inflamed skin, or using starch baths. Antihistamines may relieve the itching, and antianxiety drugs may relieve the tension or anxiety that contributes to the condition. Instruct the client to use soaps that are less alkaline and contain no lanolin. Recommend the use of lanolin-free lotions. Teach clients to avoid contact with wool.
FIGURE 75-2 · Examples of atopic dermatitis (eczema).
NCLEX Alert On NCLEX examination questions, skin conditions or disorders can contain concerns related to priority observations and interventions. For example, does the clinical scenario provide an example of an emergency case of urticaria as with anaphylaxis? For other conditions, such as psoriasis, be observant for self-esteem concerns.
Psoriasis
Psoriasis is a chronic, noncontagious, proliferative skin disorder that most commonly affects young adults and people of early middle age (Fig. 75-3). Epidermal cells rapidly proliferate and form small, scaly patches of skin. The primary cause is unknown, although hereditary, environmental, metabolic, or immune factors contribute to an outbreak of psoriasis. The course of the disorder is unpredictable. In most clients, the disease remains localized.
In some individuals, however, the severity is incompatible with a productive life. Spontaneous clearing is rare, but unexplained exacerbations (flare-ups) and improvement are common. Stress and anxiety frequently precede the disease’s exacerbations.
Signs and Symptoms
The hallmark of psoriasis is red papules covered with silvery, yellow-white scales that the client constantly sheds. These patches appear mainly on the extensor surfaces of the elbows and knees, on the scalp, and on the lower back. The nails may begin to loosen at the beginning of the fingertips (onycholysis).
Medical Treatment
Generally, treatment of psoriasis is never completely successful. The main objective is to reduce scaling and itching. Therapeutic baths, wet dressings, or lubricating ointments may be helpful, followed by application of emollient creams to soften the scaling. Specialized shampoos are used to treat scalp psoriasis. Corticosteroids may be injected into psoriatic lesions. Ultraviolet (UV) light treatment or sun exposure may be useful but requires careful supervision. Methotrexate and oral retinoids (synthetic derivatives of vitamin A) are useful in clients with severe, extensive psoriasis. However, methotrexate may cause hepatic or renal damage, bone marrow suppression, nausea, and fatigue. Photochemotherapy, which combines a photosensitizing agent (psoralen) with UV light, also may be used.
FIGURE 75-3 · Characteristic primary lesions of psoriasis.