Diagnosis and Treatment
Treatment is generally palliative. Four or five outbreaks per year are common. No cure for genital herpes exists. Antiviral medications can shorten and prevent outbreaks when the client is taking the drugs.
Screening for HSV should be done at the same time as screening for syphilis and gonorrhea. Cultures should be taken for any suspicious lesion. HSV testing can include HSV-2 blood tests, which will generally be considered diagnostic for a genital herpes infection. Only viral cultures can differentiate HSV-1 from HSV-2. The virus may bury itself, perhaps in the central nervous system, between outbreaks and become nonobservable.
Key Concept If herpes is present, a condom offers minimal, if any protection against the spread of the disease.
Episodic or suppressive treatment exists using antiviral medications. Episodic treatment (i.e., antiviral medication taken only during outbreaks) helps to speed healing and shorten the length of the outbreaks. Suppressive therapy is used if outbreaks are frequent or severe; antiviral medications are taken every day.
Antiviral medications are available and can be taken for either episodic or suppressive treatment. Side effects of antivirals are generally mild and may include headache, nausea, and diarrhea. HSV is carried in the nerves at the base of the spine, so topical ointments, such as dexpanthenol (Panthoderm), may help to ease discomfort but do not prevent or suppress outbreaks.
Genital herpes is closely associated with cervical and prostate cancer. Any woman who has had HSV should have a Pap test at least every 6 months to rule out cervical cancer. Men who have had HSV should have a rectal examination and a prostatic specific antigen test yearly for prostatic cancer. An association may also exist between genital herpes and other cancers. The person with herpes also must have a complete physical examination on a regular basis to rule out the possibility of these other diseases as well.
Because HSV is not curable, the client needs emotional support. Treatment is mostly symptomatic and directed at reducing discomfort and preventing secondary infection. Oral analgesics, such as aspirin, acetaminophen (Tylenol), or other nonsteroidal anti-inflammatory drugs (NSAIDs), may reduce systemic discomfort.
Sitz baths may relieve pain, but have no effect on the course of the disease. Cleanliness and dryness are essential to promote healing. Cotton underwear is useful. Women may need to be catheterized, although extreme caution must be used to avoid spreading the infection into the bladder. The recurrence of herpes often coincides with the menstrual cycle in the woman or during times of stress. Individuals with herpes should avoid sexual contact, especially when lesions or any symptoms are present.
Client teaching includes instruction on restricting others from using items that come in contact with the lesions, such as a toothbrush. During active outbreaks, an infected person should not share food or engage in kissing. Meticulous handwashing is necessary to prevent the spread of the lesions to another part of the body.
Cytomegalovirus
Cytomegalovirus (CMV), a member of the herpes family, is transmitted by any close contact (e.g., intercourse, kissing, breastfeeding). Although individuals with CMV typically are asymptomatic, possible clinical findings include upper respiratory symptoms, fatigue, retinitis, and pneumonia. Treatment includes symptomatic relief, for example through bed rest or acetaminophen; no specific treatment or vaccine for CMV currently exists. Immunocompromised individuals (e.g., persons with HIV/AIDS or those who are undergoing cancer chemotherapy) may be given immunotherapy and an antiviral agent to control symptoms. Pregnant women should avoid contact with CMV if possible.
Genital Human Papillomavirus
Condylomata acuminatea, more commonly known as genital warts (or venereal warts), are caused by the human papillomavirus (HPV), a large group of viruses (Fig. 70-3E, F). About 30 viruses in this group are sexually transmitted, infecting the genital area, vulva, labia, or anus, and surrounding tissues. At least 10 of the known 30 HPV types can lead to development of cervical cancer. Two strains account for about 70% of HPV-related cancer cases and are linked with abnormal Pap smears, indicating cancer of the cervix. Cancer of the anus and penis is also possible with HPV.
HPV infections are very common, but have very few signs or symptoms. Any sexually active person is at risk for HPV. The male is often the carrier of HPV, which infects and can cause cervical cancer in females. Cervical cancer is the third most common malignancy in women worldwide, and about 50% of women with cervical cancer will die. Unexplained, but known to exist, is a link between cigarette smoking and cervical cancer. Therefore, women who have HPV should not smoke. Predisposing factors for genital warts include:
• Oral contraceptive use
• Frequent sexual intercourse
• Multiple sexual partners
• Cigarette smoking
• Presence of other STIs
• Sex without condom use
Signs and Symptoms
Genital warts appear as single or multiple soft, moist, pinkish growths or bumps. The virus lives in the skin, and often no symptoms are present. Sometimes the warts form a cauliflower-like shape appearing on and around the genital structures and the anus. Lesions may not appear for several weeks or 2 to 3 months after exposure. Additional clinical signs include pruritus (itching), dyspareunia, and chronic vaginal discharge.
Nursing Alert The greatest danger with an HPV infection is the predisposition to cervical cancer.
Diagnosis and Treatment
HPV infections are diagnosed by inspection; however, many individuals are not aware they are infected. The presence of a positive (abnormal) Pap test may be the first sign that the HPV is present, as well as the first indication of precancer-ous or cancerous tissue. Because HPV is often not visible and may have no symptoms, having Pap testing is crucial, even vital, to detect early cancerous changes. With early detection, cervical cancer has a high cure rate.
Treatment for HPV occurs when warts are seen or precan-cerous changes are noted in the cervix, vulva, anus, or penis. A few specific tests can indicate the presence of human papilloma viruses. Sophisticated tests or DnA techniques are available if a differential diagnosis of specific viruses is indicated.
Often only symptomatic treatment is provided, by removal of visible genital warts and/or use of topical medications. Follow-up is necessary as soon as the Pap test is positive and particularly if the virus is discovered. Lesions must be actively treated as soon as possible to reduce the possibility of cancer. The most common treatment is weekly external application of podophyllin 10% to 25% in benzoin tincture (Pod-Ben-25) directly onto any visible warts. The drug is caustic, and the treatment is sometimes painful, so this drug cannot be used if the wart or surrounding tissue is irritated or inflamed. Contraindications also include diabetes, poor circulation, or pregnancy. If topical medications are ineffective in removing visible warts, carbon dioxide, laser therapy, cryosurgery (application of extreme cold), or cautery treatments (destruction with an electric current) may be performed. In severe cases, more extensive surgery may be needed. Treating all sexual partners simultaneously is essential to prevent retransmission of the disease. Treatment assists in bringing the virus under control, but does not necessarily cure the person. If a Pap smear shows cellular abnormalities, treatment may include a hysterectomy.
Immunization against certain types of HPV is a new approach to treating specific types of the HPV family of viruses. Long-term results of the effectiveness of HPV vaccines are being monitored. Women who are already infected with HPV will not benefit from immunization. Therefore, medical scientists have suggested that the immunization be given to young females in their adolescent to young adult years, before exposure to the virus occurs.
Key Concept The best prevention of genital warts is abstinence from sexual activity Clients who choose not to abstain should consistently and correctly use latex condoms for better, but not 100% complete, protection.
Chancroid
Chancroid is caused by the organism Haemophilus ducreyi. The first symptom is a soft sore, different from the hard chancre of syphilis. Chancroid is almost always spread by sexual contact, especially in hot, humid areas. This disease is most common in tropical climates.
Symptoms occur most often in men, but women may be carriers. Lesions appear in the genital area 3 to 5 days after contact and develop into irregular ulcers, surrounded by edema and erythema. They bleed easily when touched. The infection often spreads to the inguinal lymph nodes. Treatment is with antibiotic therapy.
Other STIs
Other common diseases can be spread by sexual contact. Vaginitis is a general term that implies inflammation and infection of the vagina. Many causes of vaginitis exist, including personal hygiene products such as soap, laundry detergent, bath oil, commercial douche preparations, spermicidal jellies, tampons, diaphragms, or colored toilet paper.
Although it is not always a venereal disease (spread through sexual contact), vaginitis is a very common occurrence in women. Both sexual partners should be treated simultaneously (concomitant treatment) to prevent reinfection. The three most common causes of microorganism-produced vaginitis are vulvovaginal candidiasis, trichomoniasis, and bacterial vaginosis.
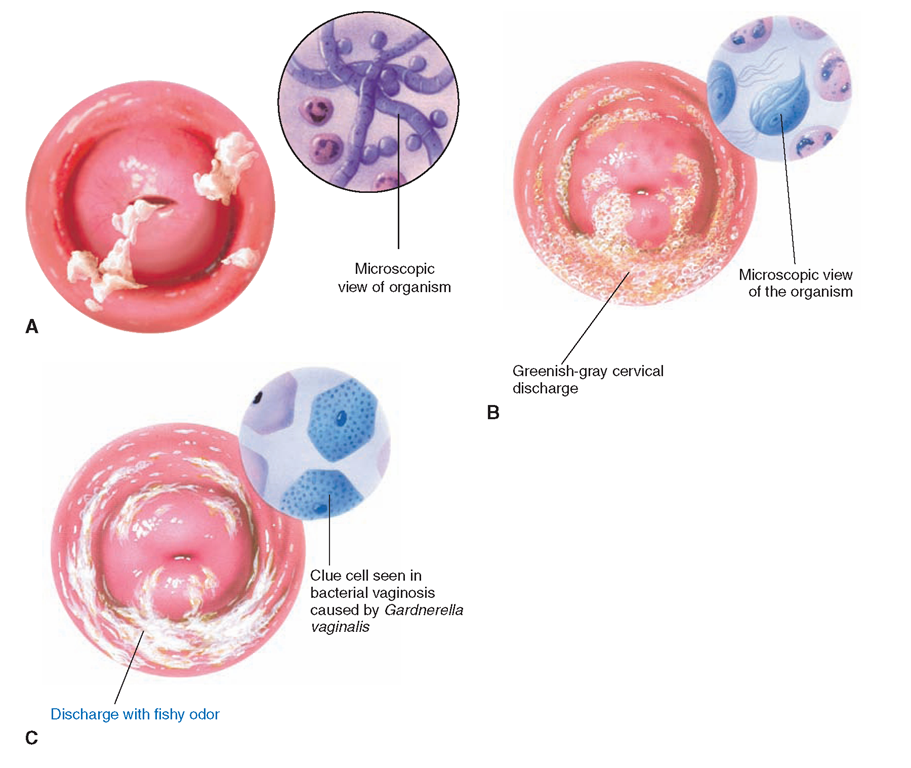
FIGURE 70-4 · (A) Vulvovaginal candidiasis is caused when the normal flora of the vaginal tract is out of balance. It commonly occurs in women who are on antibiotic therapy. (B) Trichomoniasis is caused by protozoa in the vagina. (C) Bacterial vaginosis is caused by the gramnegative bacillus Gardnereiia vaginalis.
Candidiasis
Candidiasis, also known as moniliasis, thrush, fungal infection, and yeast infection caused primarily by Candida albicans, is the most common cause of vaginitis (Fig. 70-4A). Organisms of the species Candida albicans are commonly found on the skin and in the gastrointestinal tract and may be found in the woman’s vagina. Normally, there is a homeostatic balance among this organism and others in the body. Under certain conditions, such as during a course of antibiotics, the balance is disturbed, and there is an overgrowth of candida. Overgrowth of the normal fungal population has been linked to high sugar intake, hormone disturbances, BCPs, corticosteroid therapy, malnutrition, too-frequent douching, immunosuppression, and diabetes.
Symptoms include intense itching of the vulva, which becomes inflamed and irritated; burning after urination; and a white, cottage cheese-like discharge. Diagnosis is made by putting a sample of the discharge on a microscopic slide. The physician may request a slide prepared with potassium hydroxide (KOH ).
Treatment is available with prescription and nonprescription medications. Creams or gels inside disposable applicators are used for 1 to 7 days. The 1- and 3-day fungicides are considered to be as effective as the 7-day application, and client compliance with the necessary insertion protocols is more likely to be followed. Fluconazole (Diflucan), a single-dose pill, can also be used, especially in cases of reinfection.
Self-reinfection and reinfection from the sexual partner are common. Infection is rare in a circumcised man, but candida can be found commonly under the foreskin in an uncircumcised male. Infection can be transmitted from mother to fetus during pregnancy or during delivery.
Women tend to self-treat this problem due to the availability of over-the-counter medications. Some women report relief from symptoms by swallowing acidophilus capsules, eating yogurt, or instilling yogurt directly into the vagina. Client teaching should include the awareness that a healthcare provider should be seen for persistent problems. Recurrent problems, bad-smelling greenish discharge, and severe pain are not associated with candida.
Trichomoniasis
Trichomoniasis, also known as trichomonas or “trich,” is caused by the parasitic protozoan Trichomonas vaginalis. The signs and symptoms include itching and burning of the vulva accompanied by a foul-smelling, greenish-yellow or gray, frothy or bubbly discharge (Fig. 70-4B). Red ulcerations may be seen on the vaginal wall or cervix. The parasite is usually difficult to see in men and symptoms may spontaneously disappear. However, untreated and nonsymptomatic men can still infect and reinfect female partners.
Factors that trigger growth of trichomoniasis include:
• Pregnancy
• Sexual activity
• Irritation of vaginal walls
• Trauma to the vaginal walls
• Systemic illness
• Menstruation
• Emotional upsets
Key Concept Because of the inflammation of the mucosa by the protozoa or other SlIs, women are especially susceptible to HIV infection, which can result in the further transmission of HIV to their sexual partners.
Diagnosis is confirmed by physical examination and laboratory testing. Treatment consists of metronidazole (Flagyl, Metryl, Protostat), which is a highly effective antiprotozoal and antibacterial drug. Side effects include dry mouth, nausea, bitter aftertaste, diarrhea, abdominal cramps, headache, and dizziness. Some individuals cannot take metronidazole orally. Vaginal gels and suppositories are available, but they are not as effective as oral metronidazole.
Bacterial Vaginosis
Bacterial vaginosis (BV), formerly known as Haemophilus vaginalis and now referred to as Gardnerella vaginalis, is a gram-negative bacteria. The condition also may be called nonspecific vaginitis.
Bacterial vaginosis causes a “stale fish” vaginal odor. The discharge is thin, gray-white leukorrhea that may be mild or profuse (Fig. 70-4C). Generally, no itching or burning exists, as is associated with candida or trichomonas infection.
Diagnosis is done by obtaining a vaginal smear. The physician may order a KOH preparation of the microscope slide.
Treatment is generally successful with metronidazole (Flagyl). Ampicillin and tetracycline may also be used. Sulfonamide creams or suppositories can be used but are not considered as effective as metronidazole.
Pubic Lice
Pubic lice (“crabs,” Pediculus pubis) are tiny parasites that attach themselves to pubic hair follicles and cause intense itching. The condition of having lice in the pubic area is known as pediculosis pubis. Pediculosis can spread through sexual contact, infested bed linens and clothing, or close physical contact.
Diagnosis is based on viewing the lice or their eggs (nits) attached to the hair follicles. Treatment consists of applying a drug, such as lindane (Kwell) or pyrethrins (Barc, Pyrinyl, RID), to the affected area and thoroughly cleaning all clothing and personal articles.
Because Kwell is contraindicated during pregnancy, alternate medications (e.g., Eurax) must be ordered if the woman is or suspects she is pregnant. The lice die within 24 hours after being separated from the body, but the nits can live for approximately 2 weeks. A repeat treatment is needed at that time. Sexual partners must be treated simultaneously, and household members must be carefully monitored. Other forms of pediculosis are discussed.
KEY POINTS
• Human sexuality involves the whole body, mind, and spirit. It is at the core of each individual’s personality.
• Sexual dysfunction is a person’s inability to enjoy or engage in sexual activity for any reason.
• Infertility can be caused by male or female factors. Common factors include decreased sperm production, ovulation disorders, tubal obstruction, and endometriosis.
• Infertility carries deep physiologic and psychological effects.
• Contraception is an important consideration for individuals during various stages of their fertile years. Counseling in this area must be nonjudgmental and geared to meet the needs and preferences of the individual.
• STIs have the potential to cause sterility and also, in some cases, death.